Nutrition for hemodialysis
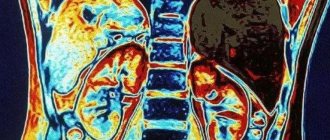
Chronic renal failure (CRF) is the final stage of all renal diseases.
Program hemodialysis is one of the methods of its treatment. If a person’s diet in the pre-dialysis period depended on what kind of kidney disease he suffered from, then during program hemodialysis the recommendations may be completely different.
But specific recommendations on the patient’s nutrition should be given by the attending physician. After all, they depend on the duration of the patient’s hemodialysis experience, residual renal function, the presence of complications and many other reasons.
We can only give general recommendations.
Contraindications
Only emotionally stable and cooperative patients are subject to long-term dialysis treatment. P. d. is not performed in patients with dystrophy, malignant neoplasms, hematological malignancies, incurable heart or pulmonary failure, cirrhosis of the liver, hemiplegia, or contagious chronic infection. P. d. is contraindicated in cases of suspected damage or disease of the abdominal organs and diaphragm, with paralytic ileus, limited peritonitis, infection of the abdominal wall, colostomy. Catheterization of the abdominal cavity and P. d. are difficult in the presence of extensive peritoneal adhesions, hepatosplenomegaly, large polycystic kidneys, pregnancy, and scars of the anterior abdominal wall.
Protein intake during hemodialysis
The first concerns protein intake. In the conservative period (before prescribing hemodialysis), the patient is usually limited to 0.5 g per 1 kg of weight per day. Table salt - up to 5 g per day. In case of severe arterial hypertension, a completely salt-free diet is even prescribed, since salt is contained in foods in sufficient quantities for the patient’s body. Although this regime is not controversial. It may be better not to sit on a low-protein, salt-free diet for a long time, but to start treatment earlier with one of the types of dialysis (programmed hemodialysis or peritoneal dialysis).
During hemodialysis, it is not only allowed, but in most cases it is recommended to consume more protein than a healthy person. Because in the process of hemodialysis blood purification, patients also lose useful substances: amino acids, oligopeptides, water-soluble vitamins, microelements. That is why the diet for hemodialysis should be as complete as possible, and first of all, in terms of animal protein content. The recommended optimal amount is 1.2 g per 1 kg of weight per day.
Naturally, the diet should be balanced: in addition to proteins, you need to consume fats and carbohydrates in sufficient quantities. But here you should keep in mind what disease led to hemodialysis. If, for example, chronic renal failure is caused by diabetes mellitus, then carbohydrates in the diet of such a patient are, of course, limited.
Prevention of kidney diseases
In order to prevent the body from causing serious “failures”, you should not neglect a preventive medical examination. Your kidneys will enjoy excellent health if you follow these simple rules:
- Diet. Protein and fatty foods should be kept to a minimum.
- Refusal of salt and alcohol.
- Drinking regimen: 30-40 ml/kg body weight. (The norm is for a healthy adult; for a child the numbers are slightly different).
- Gut health (avoid constipation).
- Temperature balance and strengthening the immune system. (Protect yourself from hypothermia).
Yoga and oriental dancing are very useful. But heavy physical activity can only bring harm.
Water consumption during hemodialysis
The second recommendation relates to water consumption. A patient undergoing hemodialysis inevitably experiences a further decline in kidney function, including a decrease in water excretion, up to the complete cessation of urine output. And although before this moment the presence of urine in the patient does not provide a significant effect in reducing the level of azotemia (excessive content in the blood of nitrogen-containing products of protein metabolism - urea, creatinine, etc.), it maintains the body’s water balance. As the disease progresses, when the water-excreting function of the kidneys disappears, it is necessary to introduce restrictions on fluid consumption. This is especially true for patients with symptoms of heart failure and arterial hypertension.
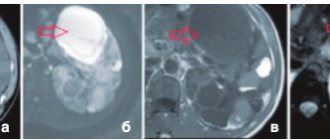
But an individual approach is very important here, because the preservation or decline of the water-excreting function of the kidneys depends on the disease. For example, with congenital kidney dysplasia, polycystic disease, pyelonephritis, it can persist for a very long time. At the same time, with glomerulonephritis and diabetes mellitus, it fades very quickly. Depending on this, the doctor will prescribe a completely different water regimen. The general recommendation is: during the interval from one hemodialysis session to another, take in fluids of no more than 5% of body weight.
At the same time, the recommendation to eat normally does not in any way contradict the restriction of fluid: the approximate water content in foods is 50-70%.
During the procedure, along with nitrogenous metabolites and other toxic substances, excess fluid is removed. When the patient gains too much of it, problems arise due to the early development of heart failure and poor tolerability of hemodialysis.
What can you eat?
Patients undergoing kidney hemodialysis can eat:
- chicken protein prepared in any way;
- steamed or boiled fish with vegetables;
- first courses with vegetables;
- up to 300 g of unsalted black or bran bread;
- lean meats prepared by any method other than frying;
- watermelons, pumpkin, dried apples, pears;
- vegetable or butter;
- low-fat milk;
- juices from fruits or vegetables diluted with water, tea;
- vermicelli, stewed vegetables.
Limiting foods containing potassium
Third recommendation: limiting foods containing large amounts of potassium. The body is extremely sensitive to fluctuations in potassium levels in the blood. Since our patients have no renal function (and potassium is excreted primarily by the kidneys), hyperkalemia develops (increased potassium concentration in the blood). And this condition can sometimes even be fatal. The fact is that if the patient does not consume any products containing potassium from session to session, a blood test will still show an increase in its content in the blood - by approximately 1 mmol per 1 liter per day. The physiological limit of potassium content in the blood is 3-5.5 mmol per 1 liter. Potassium is found in large quantities primarily in dried fruits, fresh vegetables, and fruits. To a lesser extent - in products of animal origin. Only the attending physician can recommend exactly how many oranges a particular patient can eat, relatively speaking, per day.
Corrections of phosphorus-calcium metabolism
The fourth recommendation concerns the correction of phosphorus-calcium metabolism, which is usually impaired in patients on hemodialysis. This condition must be identified by the attending physician: the levels of phosphorus and calcium in the blood need to be examined. The phosphorus-calcium product is calculated and bone density is assessed using densitometry. For correction, special medications can be prescribed (phosphate binders, calcium supplements, vitamin D3) while simultaneously limiting foods containing large amounts of phosphorus, for example, dairy products.
Limiting medications containing aluminum
Another very important recommendation is to limit medications containing aluminum. It is extremely toxic for a patient with renal failure and causes a number of serious complications: aluminum dementia (severe damage to the nervous system), bone damage, anemia. It is no coincidence that hemodialysis departments use special water purification systems aimed, among other things, at getting rid of aluminum. But often aluminum-containing drugs are prescribed to treat concomitant diseases. For example, Almagel, phosphalugel - for gastritis, peptic ulcers. This causes serious harm to kidney patients.
Patients should also not cook food in aluminum containers and take multivitamin complexes containing vitamin A and mineral supplements without consulting a nephrologist.
In conclusion, we emphasize once again: the diet for hemodialysis should be balanced, complete and, in the absence of complications, not significantly different from the diet of a healthy person.
Sample menu
It is known that patients with kidney failure undergoing dialysis are required to follow a strict and correct diet. This means that various snacks and thoughtless snacks, which busy people with busy work schedules love to abuse, are thrown out of the daily diet.
Breakfast. Typically, nutritionists recommend starting the day either with an egg omelet with herbs and vegetables, or with brewing various cereals and porridges. This is especially true for rice, since it can be consumed unlimitedly. In addition to the food you have already eaten, you can add a salad with a dressing of olive oil, yogurt or sour cream.
Dinner. A mandatory point about it: it should have three positions consistently every day. For the first course - soup (meat broth, borscht), for the second - chicken with a side dish (pilaf, rice, buckwheat) without spices or salt. Kissel is suitable for dessert, as it has a positive (from the point of view of a healthy diet) effect on the functioning of the kidneys.
For dinner, you can prepare mashed potatoes with meat or vegetables, and then treat yourself to a cup of fresh herbal infusion or tea. Speaking of coffee, it should be noted that lovers of this drink can enjoy it, but only once a week.
- 1st meal – rice porridge or omelet with milk, black tea.
- 2nd meal – fruit salad (recipe including any fruit indicated for consumption) with sour cream or vegetables with olive oil.
- 3rd meal – puree soup or sour cream beetroot soup, steamed beef or boiled chicken breast, vegetable salad with vegetable oil or fruit jelly.
- 4th meal – fruit jelly or 2 pieces of watermelon or melon.
- 5th meal - boiled potatoes or potato zrazy, boiled chicken fillet in sour cream sauce or fresh vegetable salad, herbal infusion or berry jelly.
Sources
- Sulistyaningsih DR., Nurachmah E., Yetti K., Hastono SP. Nurses' experience in improving adherence to fluid intake and diet in hemodialysis patients. // Enferm Clin - 2021 - Vol31 Suppl 2 - NNULL - p.S20-S23; PMID:33849163
- Kishimoto N., Hayashi T., Mizobuchi K., Kubota M., Nakano T. Vitamin A deficiency after prolonged intake of an unbalanced diet in a Japanese hemodialysis patient. // Doc Ophthalmol - 2021 - Vol - NNULL - p.; PMID:33544296
- Limwannata P., Satirapoj B., Chotsriluecha S., Thimachai P., Supasyndh O. Effectiveness of renal-specific oral nutritional supplements compared with diet counseling in malnourished hemodialysis patients. // Int Urol Nephrol - 2021 - Vol - NNULL - p.; PMID:33452957
- St-Jules DE., Rozga MR., Handu D., Carrero JJ. Effect of Phosphate-Specific Diet Therapy on Phosphate Levels in Adults Undergoing Maintenance Hemodialysis: A Systematic Review and Meta-Analysis. // Clin J Am Soc Nephrol - 2021 - Vol16 - N1 - p.107-120; PMID:33380474
- Byrne FN., Gillman BA., Kiely M., Palmer B., Shiely F., Kearney PM., Earlie J., Bowles MB., Keohane FM., Connolly PP., Wade S., Rennick TA., Moore BL ., Smith ON., Sands CM., Slevin O., McCarthy DC., Brennan KM., Mellett H., Dahly D., Bergin E., Casserly LF., Conlon PJ., Hannan K., Holian J., Lappin DW., O'Meara YM., Mellotte GJ., Reddan D., Watson A., Eustace J. Pilot Randomized Controlled Trial of a Standard Versus a Modified Low-Phosphorus Diet in Hemodialysis Patients. // Kidney Int Rep - 2021 - Vol5 - N11 - p.1945-1955; PMID:33163715
- Stanford J., Charlton K., Stefoska-Needham A., Zheng H., Bird L., Borst A., Fuller A., Lambert K. Associations Among Plant-Based Diet Quality, Uremic Toxins, and Gut Microbiota Profile in Adults Undergoing Hemodialysis Therapy. // J Ren Nutr - 2021 - Vol31 - N2 - p.177-188; PMID:32981834
- Palmer B.F. Potassium Binders for Hyperkalemia in Chronic Kidney Disease-Diet, Renin-Angiotensin-Aldosterone System Inhibitor Therapy, and Hemodialysis. // Mayo Clin Proc - 2021 - Vol95 - N2 - p.339-354; PMID:31668450
- Welte AL., Harpel T., Schumacher J., Barnes JL. Registered dietitian nutritionists and perceptions of liberalizing the hemodialysis diet. // Nutr Res Pract - 2021 - Vol13 - N4 - p.310-315; PMID:31388407
- Khosroshahi HT., Abedi B., Ghojazadeh M., Samadi A., Jouyban A. Effects of fermentable high fiber diet supplementation on gut derived and conventional nitrogenous product in patients on maintenance hemodialysis: a randomized controlled trial. // Nutr Metab (Lond) - 2021 - Vol16 - NNULL - p.18; PMID:30911321
- Alipoor E., Karimbeiki R., Shivappa N., Yaseri M., Hebert JR., Hosseinzadeh-Attar MJ. Dietary inflammatory index and parameters of diet quality in normal weight and obese patients undergoing hemodialysis. // Nutrition - 2021 - Vol61 - NNULL - p.32-37; PMID:30684849