Author: Soldatenkov Ilya Vitalievich
, for sindrom.info ©
Empty sella syndrome is a complex of clinical and anatomical disorders that arise due to insufficiency of the sella diaphragm. In the temporal region there is a peculiar obstacle that prevents the penetration of cerebrospinal fluid into the subarachnoid space. It is in this cavity that the pituitary gland is located, which regulates the level of hormones, metabolism and accumulation of substances in the body, and is responsible for human reproductive functions. If the cerebrospinal fluid enters the sella turcica without any obstruction, the pituitary gland begins to deform. Often it finds itself pressed against its own bottom and walls, which leads to disruption of its functioning.
The syndrome was discovered in 1951 by V. Bush, who studied the causes of death of more than 700 people. 40 of them (34 were women) had practically no diaphragm at all, and the pituitary gland lay along the bottom of the “pit” of the sella, which seemed completely unfilled - empty. The anomaly gets its name from the special appearance of the sphenoid bone, which actually resembles a saddle needed for horse riding.
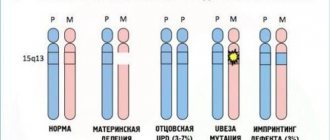
Most often, obese women over the age of 35 suffer from empty sella syndrome (ESTS). There may also be a genetic predisposition to the disease. That is why scientists divide the anomaly into 2 types:
- Primary syndrome that has been inherited;
- Secondary – arose as a result of a malfunction of the pituitary gland.
The pathology can be asymptomatic or manifest itself as visual, autonomic, or endocrine disorders. Along with this, the psycho-emotional state of the patient often changes.
Causes of the anomaly
Empty sella syndrome has not yet been fully studied by scientists. It has only been proven that pathology can appear as a result of surgery, radiation therapy, mechanical damage to brain tissue or diseases of the pituitary gland.
Experts suggest that one of the reasons for the development of SPTS may be insufficiency of the diaphragm, which separates the space of the sphenoid bone from the subarachnoid cavity. At the same time, it excludes the small “hole” where the pituitary stalk is located.
During menopause or pregnancy in women, during puberty, or any similar conditions that are accompanied by a restructuring of the endocrine system, hyperplasia of the pituitary gland itself may occur, which will also lead to pathology. Sometimes the disorder is caused by hormone replacement therapy or contraceptives.
Any variant of congenital anomaly in the structure of the diaphragm can cause the development of a dangerous syndrome. But along with them, the following factors can also affect the patient’s condition:
- Rupture of the suprasellar cistern;
- Increased internal pressure in the subarachnoid cavity, increasing the effect on the pituitary gland, for example, with hypertension and hydrocephalus;
- Reduction in the size of the pituitary gland and the ratio of volumes to the sella;
- Problems with blood circulation in benign tumors.
What is sella turcica?
The sella turcica is a small bone formation located in the middle of the skull. Its shape resembles a saddle, hence the name.
In the bed of this bone formation there is a very important neuroendocrine organ - the pituitary gland. This is an endocrine gland that produces many hormones, including sex hormones.
Cases of sella turcica pathology can manifest themselves in completely different ways: in the form of a disorder of the nervous system, disruption of female reproductive function, hormonal imbalance, visual impairment, and so on.
The human body functions correctly and harmoniously, thanks to the regulation of the work of all systems and organs by the pituitary gland. Therefore, in cases of failure of this correct operation, doctors may be interested in the condition of the gland. X-ray changes in the sella turcica provide valuable diagnostic information about the pituitary gland.
Symptoms of SPTS
Usually the anomaly occurs unnoticed and does not cause any discomfort to the patient. Often, the syndrome is discovered by chance during a routine X-ray examination. The pathology occurs in 80 percent of women over the age of 35 who have given birth. Approximately 75% of them are obese. However, the clinical picture of the disease can vary dramatically.
Most often, the syndrome reduces a person’s visual acuity, causes a generalized narrowing of peripheral fields, and bitemporal hemianopsia. Patients also complain of frequent headaches and dizziness, lacrimation, and fogginess. In rare cases, swelling of the optic disc is observed.
Many nasal diseases result from rupture of the sella, which occurs due to excessive pulsation of the cerebrospinal fluid. In this case, the risk of developing meningitis increases several times.
Almost all endocrine disorders lead to pituitary dysfunction and the occurrence of SPTS. Among them are both rare genetic abnormalities and:
- increased, decreased levels of tropic hormones;
- excessive secretion of prolactin;
- metabolic syndrome;
- dysfunction of the anterior pituitary gland;
- increased production of adrenal hormones;
- diabetes insipidus.
The following disorders can be noticed from the nervous system:
- Regular headache. Occurs in approximately 39% of patients. Most often, it changes its location and strength - it can go from mild to unbearably regular.
- Disorders in the functioning of the autonomic system. Patients complain of surges in blood pressure, dizziness, spasms in various organs, and chills. They often lack air, feel unreasonable fear, and are overly anxious.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 3 | 5 | 7 | 13 | 15 | 18 | 21 | 6 | 10 | 14 | 16 | 26 | 36 | 42 |
Diagnostics
Diagnosis of the disease includes several most important stages, including:
- Collection of patient history and complaints. If his medical history revealed severe traumatic brain injuries, brain tumors, especially the pituitary gland, recent radiation therapy or surgery, then all this should alert an experienced doctor. Also, several pregnancies of a woman after 30 years or a long-term course of treatment with hormonal contraceptives can cause doubts.
- Laboratory research. In addition to basic blood and urine tests, first of all, the patient needs to undergo hormonal tests. Most often, this is an analysis that determines the level of pituitary hormones in the body. This method helps to notice even the most minor disruptions in the patient’s condition. But normal levels of hormones in the blood do not always indicate healthy pituitary function. Sometimes hormonal disorders do not accompany the disease.
- Instrumental examination. To identify and define the syndrome, computed tomography and pneumoencephalography are usually used, along with the introduction of contrast agents into the cerebrospinal fluid. The syndrome can also be detected by MRI examination, which will indicate the expansion of the ventricles of the brain and any other spaces containing cerebrospinal fluid. If such equipment is not available, you can undergo examination using a regular X-ray machine.
Most often, the diagnosis of SPTS is established when the patient undergoes an examination aimed at identifying a pituitary tumor. However, not in all cases, neuroradiological data indicate the presence of a tumor. The frequency of such disorders is approximately equal to the empty sella syndrome – 36 and 33%.
The presence of pathology can be assumed if the patient exhibits at least minimal clinical symptoms. Pneumoencephalography is not required in this case; you just need to monitor the patient’s condition. The main thing is not to confuse SPTS with a tumor or pituitary adenoma. It is differential diagnosis that is aimed at identifying hyperproduction of hormones.
What diseases can it be associated with?
- Acromegaly is a neuroendocrine disease that develops with overproduction of growth hormone (somatotropin, growth hormone); The reason for this is usually pituitary adenoma (somatotropinoma), which is a benign tumor; simultaneous hyperproduction of somatotropin and prolactin by the tumor is common.
- Itsenko-Cushing's disease is a hypersecretion of adrenocorticotropic hormone, which develops mainly as a result of head contusions, concussions, traumatic brain injuries, encephalitis and other lesions of the central nervous system.
- Hyperprolactinemia - can develop as an independent or concomitant disease (against the background of hypothyroidism or adrenal insufficiency), is treated with hormone replacement therapy; may develop while taking certain medications, the abolition of which allows the condition to normalize.
- Hypopituitarism (Sheehan syndrome) - develops as a result of destruction of the adenohypophysis with a subsequent persistent decrease in the production of tropic hormones and disruption of the activity of peripheral endocrine glands; The main cause of hypopituitarism is circulatory disorders in the hypothalamic-pituitary region that develop after childbirth, complicated by massive blood loss, thromboembolism, and sepsis.
- Primary hypothyroidism - replacement therapy (mostly carried out for life) of hypothyroidism can provoke a secondary pituitary adenoma and, as a result, an empty sella turcica.
- Pituitary microadenomas (prolactinomas and somatotopinomas) - treatment of such with dopaminomimetics and somatostatin analogues, respectively, provoke changes in the location of the pituitary gland; the clinical picture corresponds to pituitary disorders associated with the hormonal activity of the pituitary tumor.
Treatment of pathology
If you suspect the occurrence of SPTS, you should definitely consult a therapist. Based on the patient's complaints, test results and various studies, the doctor will send the patient to one of the following doctors, who will treat him. This could be an ophthalmologist, neurologist or endocrinologist.
The choice of treatment methods depends on the main symptoms of the pathology. The specialist must correct disorders that arise as a result of visual impairment or the functioning of the nervous and endocrine systems. The clinical picture of the disease and the severity of the anomaly help to choose the truly correct path of treatment: through medications or surgery.
If the syndrome does not cause much discomfort and does not manifest itself in any way, then the patient does not need treatment for this disease. In this case, patients only need to register, monitor their well-being and regularly undergo all the necessary examinations aimed at monitoring their condition.
Drug treatment
If laboratory tests have revealed a deficiency of any hormone in the body, or even a whole group of them, drug therapy will be aimed at hormonal replacement from the outside. That is, the patient will have to take a course of contraceptives for some time.
In case of disorders of the autonomic system, the patient must take sedatives, painkillers, as well as medications that normalize blood pressure.
Surgery
This type of therapy is used in rare cases, usually only when there is a threat of vision loss. Thanks to surgery, it is possible not only to restore the diaphragm, but also to remove a dangerous tumor. Indications for the operation also include:
- Sagging of the optic nerves into the cavity of the diaphragm.
- Leakage of cerebrospinal fluid through the bottom of the subarachnoid cavity. To eliminate liquorrhea with muscle, tamponade of the sphenoid saddle is performed.
It was revealed that treatment of pathology with traditional medicine does not bring any improvement. In this way, you can only influence the signs of an anomaly. Experts advise following a healthy lifestyle: exercise, eat only healthy foods and stick to the most comfortable daily routine. In this way, you can not only prevent the occurrence of complications of the syndrome, but also get rid of the accompanying signs of the disease.
How to treat empty sella syndrome?
Treatment for empty sella syndrome depends entirely on its causes. Most often, therapy consists of methods of treating the underlying disease against which the syndrome developed. Symptomatic treatment is no less popular.
Treatment methods, determined by the underlying disease, can be divided into drug and surgical treatment:
- medicinal - taking medications that correspond to a specific endocrine disorder, pain relief therapy and symptomatic treatment of autonomic dysfunctions;
- surgical - it is advisable in case of sagging of the optic chiasm into the opening of the diaphragm of the sella turcica with compression of the optic nerves, leakage of cerebrospinal fluid through the thinned bottom of the sella turcica.
The operation consists of either transsphenoidal fixation of the chiasm or sella turcica tamponade.
Treatment for empty sella syndrome is not prescribed if it is diagnosed as an MRI phenomenon. Correction of endocrine, visual or neurological disorders may be separately applicable.
Consequences
The syndrome can cause disruption of the normal functioning of the brain and its membranes. This disorder ultimately causes the pituitary gland to shrink in size and move toward the walls of the subarachnoid space due to the pressure placed on it. The consequences of this condition include:
- endocrine disorders: thyroid disease, decreased immunity, reproductive system disorders;
- micro-strokes, regular migraines and various neurological diseases;
- impaired visual acuity, eye function, and in advanced cases, blindness.
Statistics show that about 10% of babies are born with congenital SPTS, but only 3% of them are actually bothered by the disease. The remaining 7% are not even aware of the existing anomaly in the body during their lifetime.
In any case, if the patient is predisposed to developing the disease or already has it, he should seek advice from an experienced, qualified doctor who will prescribe appropriate and adequate treatment.
Forecast
About 10% of the world's inhabitants have the syndrome. It can occur either in a latent form or with a fairly large number of signs accompanying the disease. Sometimes such symptoms can significantly reduce the patient’s quality of life. The prognosis directly depends on the severity of the disease and its clinical manifestations. Most often, patients with the syndrome do not even suspect the presence of the disease, from which we can conclude that the prognosis is only favorable. But stories are also familiar with opposite situations, when patients have to take medications all their lives to improve their well-being and fight for their health. Although in this case, to improve well-being, it is enough only to eliminate the symptoms associated with the disease.