Red eye syndrome - what is it?
This syndrome can be defined as a microcirculatory disorder that occurs due to expansion of the vascular wall of the sclera. It is considered the most common sign in ophthalmology, as it is included in the symptoms of a very large number of diseases. You should definitely be wary of the accompanying symptoms of red eye syndrome, such as pain and decreased quality of vision. The intensity of the vascular pattern on the protein membrane, as a rule, is not related to the degree of any pathology. Let's find out what causes red eye syndrome. Treatment depends on the etiology and nature of the development of the underlying disease.
Read also
Myopia
Vision plays a huge role for a person.
Through the eye we experience the entire amazing and diverse world. A person receives 80-90% of information from the surrounding world through vision. Therefore, it is a huge tragedy... Read more
Partial optic atrophy (PANA)
Vision is the most important function in human life. We receive 70% of information from the world around us through vision. The optic nerve is one of the most important elements of the organ of vision. It is through...
More details
Contact lenses/contact correction
Vision is one of the senses through which we learn about the world around us. Good vision is essential for a high quality of life. The most important characteristic in diagnosis is the acuity...
More details
Blindness
Vision is a unique gift that nature has given us. We can truly appreciate it only when we lose. With a number of diseases, vision loss may decrease, sometimes almost to the point of complete blindness. Often…
More details
Headache treatment
Tarasova Svetlana Vitalievna. Expert No. 1 in the treatment of headaches and migraines. Head of the Multiple Sclerosis Center. Neurologist of the highest category. Doctor of Medical Sciences Migraine is one...
More details
What causes red eye syndrome?
There are many reasons that can trigger the appearance of this syndrome. They can be combined into several large groups:
- physiological;
- environmental exposure;
- ophthalmopathology;
- diseases that are not related to ophthalmopathologies.
Physiological factors include heavy physical activity, vomiting, prolonged coughing or sneezing, the consequences of drinking alcoholic beverages, working at a computer, etc. This group can also include a factor such as discomfort caused by wearing incorrectly selected optics. The redness of the protein membrane is not accompanied by inflammation. This syndrome does not cause any complications. However, this does not mean that these causes cannot lead to the development of the disease if their effect on the eyes is systematic.
Environmental factors: exposure to sunlight, strong or cold winds, frost, changes in weather conditions, exposure to dust and other foreign objects in the eyes, mechanical injuries, chemical burns to the eyes.
Diseases in which the eyes turn red may have an infectious etiology or relate to aseptic processes. In the first case, we are talking about conjunctivitis (viral, bacterial, chlamydial), dacryocystitis, blepharitis, uveitis, keratitis, episcleritis, iridocyclitis and other diseases caused by pathogenic microorganisms. Aseptic processes of a pathological nature, in which microbes do not play any significant role, include: keratopathy, keratoconus, floppy eyelid syndrome, hemorrhagic tissue lesions, corneal ulcers, lacrimal gland tumors, glaucoma, trichiasis, mucosal detachment and other diseases. Each of these diseases has extensive symptoms and its own specific symptoms. Thus, red eye syndrome can signal relatively mild diseases, as well as pathologies that can lead to blindness.
Another group of factors are diseases that are not related to ophthalmic pathologies. The human body is a single system in which the disease of one organ often affects the condition of other organs. Red eye syndrome most often occurs with diseases that affect blood vessels: hypertension, allergies. Sometimes the sclera turns red due to an overdose of anticoagulants - medications that prevent the formation of blood clots. These causes do not lead to inflammation of the eyes and its structures.
Separately, it is worth listing the risk factors that can provoke red eye syndrome: autoimmune diseases, diabetes mellitus, dry eye membranes that develop with age-related changes, asthenopia, the use of low-quality cosmetics, infectious diseases.
Prognosis and prevention
Minor symptoms of the syndrome caused by exposure to external factors can be eliminated even at home. Severe pathology requires mandatory consultation with a doctor, however, even in this case, the prognosis is often favorable.
High-quality hygiene of the visual organs, timely treatment of ophthalmological diseases, reduction of visual stress, and prevention of injuries to the eyeballs help prevent the development of the disorder. Periodic intake of vitamin and mineral complexes, agreed upon with a doctor, allows you to maintain normal vision.
Delicious recipe! Where is the best shashlik in Kazan?
Even if it occurs with mild symptoms, red eye syndrome should not be ignored. Untimely treatment measures can cause deterioration in visual function or the development of other undesirable consequences.
As such, “red eye” syndrome does not exist; it is an artificially created concept that includes a wide range of ophthalmological diseases of various natures, united by the presence of just one symptom - redness of the eye, caused by dilation of superficial blood vessels.
In the vast majority of cases, the diagnosis of redness in one or both eyes is based on anamnesis and objective examination. It is extremely important that the general practitioner (GP) can distinguish between harmless conditions accompanied by redness of the eye and serious diseases (especially keratitis, iridocyclitis and glaucoma) that require immediate specialist attention.
Diseases included in the “red eye syndrome”
- Blepharitis (simple, scaly, ulcerative): scaly, swollen edges of the eyelids with the presence of hyperemia of the vault (in the presence of bubbles and vesicles, assume herpetic origin).
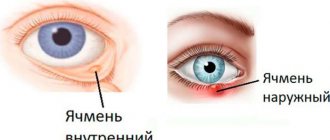
- Stye/chalazion
- Subconjunctival hemorrhages (eg, overdose of drugs that reduce blood clotting)
- Keratitis/keratoconjunctivitis
- Scleritis / episcleritis
- Conjunctivitis (often a bilateral process), superficial redness in the vault, lacrimation, sensation of itching, burning, foreign body like “sand in the eyes”, gluing of the eyelids with exudate, runny nose. Conjunctivitis is predominantly viral in nature (adenovirus), except in cases where there is purulent discharge (bacterial conjunctivitis) or itching, sneezing, runny nose in combination with allergic rhinitis or asthma (allergic, atopic conjunctivitis). In case of itching, differentiate with contact allergies (cosmetics, eye drops, contact lens care products). Dry conjunctivitis (conjunctivitis sicca): feeling of sand in the eyes or burning in elderly patients.
- Iridocyclitis
- Acute attack of glaucoma (sharp and very painful increase in intraocular pressure, which leads to visual disturbances)
- Dacryoadenitis/adenitis
- Edematous endophthalmos
Other reasons:
- redness of the eyes is possible due to eye fatigue;
- with physical impact - particles of dust, sand, smoke, cosmetics, etc. getting into the eyes, improper use of contact lenses
- due to chemical exposure (chlorinated water, cosmetics, soap, chemical reagents, etc.
- when exposed to allergens;
- for dry eye syndrome.
- Cluster headaches (the eye is often bloodshot, the pupil becomes temporarily constricted, vision may be blurry, and the eyelid on the affected side of the head droops and may appear swollen)
- Sjögren's syndrome (Due to impaired secretion of tear fluid, patients experience chronic inflammation of the outer membranes of the eye - the conjunctiva and cornea. Patients are concerned about the red color of the whites of the eyes, pain and burning, sensation of a foreign body in the eye, itching, photophobia. When crying, tears are not released)
Differential diagnosis
Patient complaints
- Pain. One of the characteristic complaints with red eye syndrome is pain, accompanied by photophobia, lacrimation, and blepharospasm. This is one of those complaints that serves as an indicator of the severity of the process. It is this complaint that is key for such emergency conditions as part of the “red eye” syndrome such as: acute attack of glaucoma, keratitis, adenoviral conjunctivitis. Analysis of the nature of pain in combination with data from anamnesis, clinical examination and data from additional research methods allows us to gradually exclude a number of pathologies, settling on the only correct option.
- According to the scheme, one of the first and most urgent pathologies in the red eye syndrome is an acute attack of angle-closure glaucoma . The leading signs of an ongoing attack are, first of all, severe pain radiating to the corresponding half of the head and shoulder, as well as diffuse congestive injection of conjunctival vessels, cloudy edematous cornea, and rigid pupil. The absence of discharge and the rather rare occurrence of this pathology serve as additional confirmation in favor of an acute attack. Anamnesis data on the presence of glaucoma in close relatives are a risk factor for the manifestation of this pathology. However, the most significant differential sign that objectively confirms an acute attack of glaucoma is the presence of high intraocular pressure (IOP).
- With keratitis, the intensity of pain can vary from moderate to severe. A characteristic symptom in this case is a violation of the integrity of the corneal epithelium, accompanied by pronounced pericorneal injection, purulent or mucopurulent discharge, and sometimes infiltration of the cornea. Secondary evidence may include a history of recent stress or trauma. The differential sign in this case will be the presence of a defect in the corneal epithelium when stained with a fluorescein solution and the identification of microorganisms during bacteriological examination.
- One of the most common pathologies with a fairly acute onset is adenoviral conjunctivitis (AVC). The intensity of the pain is less pronounced (from moderate to weak) than with the pathologies described above, but in combination with intense lacrimation and photophobia it brings significant inconvenience to patients. As with conjunctivitis of other etiologies, AVK is characterized by the presence of serous discharge and diffuse injection. But the key signs of this process (although not always apparent) are characteristic films on the conjunctiva of the eyelids and infiltrates on the cornea. A recent history of acute respiratory viral infection or contact with a patient with VKA may provide additional evidence in favor of this process. A differential sign can be the characteristic dynamics of the clinical course of the disease: a bright onset, gradual involvement of the second eye in the process, regional lymphadenitis, somatic malaise.
Itching. Less common, but no less significant, is the complaint of itching. Most often it is associated with allergic eye damage. However, itching can also accompany other inflammatory eye diseases, such as VKA.
- This complaint is key at an early stage in the differential diagnosis of conjunctivitis. The combination of itching sensation with signs: diffuse small folliculosis of the conjunctiva and severe swelling on biomicroscopy and with anamnesis data: characteristic seasonality (spring or autumn) is specific for allergic conjunctivitis. Of course, various variations in the course of the disease are possible depending on the severity and severity of the process. Moreover, if the acute allergic process rarely raises doubts, then chronic allergies (especially due to irrational pharmacotherapy) require careful analysis. In this case, the differential sign can be considered rapid (from several minutes to several days) relief of clinical signs with antihistamines.
- However, itching can accompany the course of AVC . Differential diagnosis is difficult at the initial stage of development of AVC before the appearance of characteristic clinical signs (formation of films on the conjunctiva and the appearance of pinpoint infiltrates on the cornea). In contrast to the allergic process, with VKA the main symptom is more pronounced hyperemia of the conjunctiva, sometimes with small petechial hemorrhages. In combination with medical history (recently suffered from acute respiratory viral infection or contact with a virus carrier), the results of biomicroscopy suggest the viral nature of the inflammatory process. The differential feature that ultimately determines the nature of the process is the further characteristic stage of the disease with a specific clinical picture and the involvement of the second eye in the process.
- Complaints of itching are also common when dry eye syndrome is combined with blepharoconjunctivitis . Signs characteristic of this process are the absence of a “tear meniscus” visible during biomicroscopy (a sign of “dry eye”) and the presence of muffs and scales around the roots of the eyelashes (a sign of blepharoconjunctivitis). Anamnesis data indicate a significant duration of the process, sometimes lasting for years. The differential sign will be the patient's complaint of instability of visual acuity when blinking.
Delicious recipe! Food ppt recipes delicious dishes
Detachable. An important complaint for differential diagnosis is the presence of discharge. The nature of the discharge varies depending on the etiology of the process. It should be borne in mind that patients often describe the appearance of any discharge with the expression “the eyes fester.” To really assess the nature of this complaint, it is necessary to clarify what color the discharge is: green, yellow, white or colorless. The consistency is also important - hard dried grains of sand, slimy or foamy.
- Allergic conjunctivitis is characterized by discharge in the form of strands of serous-mucosal type.
- The differential sign for bacterial conjunctivitis is purulent discharge.
- With adenoviral conjunctivitis, the discharge will be serous.
Anamnesis data
For greater reliability of the proposed diagnosis, in addition to complaints, it is important to analyze the anamnesis data.
- Onset of the disease. Indications of the nature of the onset of the disease can serve as a guide for differential diagnosis already at the stage of interviewing the patient. An acute onset is characteristic of an acute attack of glaucoma, AVC, keratitis, including herpetic etiology, as well as a bacterial corneal ulcer. Dry eye syndrome is characterized by a gradual onset. And with bacterial and allergic conjunctivitis, the onset of the disease can be either acute or gradual.
- The nature of the disease or the frequency of exacerbations. A striking and informative addition to the analysis of anamnesis data is the nature of the course of the disease. At the same time, the constant sluggish nature of the course of the disease can be considered a differential sign for this indicator in dry eye syndrome. In the allergic process, the seasonality of exacerbations is characteristic: spring, autumn. The development of herpetic lesions is usually preceded by stress provocation (physical, emotional stress, hypothermia, overheating). I would especially like to note the lack of regularity of exacerbations during chlamydial infection, which creates certain difficulties in diagnosis. Acanthamoeba lesions, which have recently become widespread among contact lens users, are characterized by periodic exacerbations with increasing symptoms with each subsequent exacerbation.
Inspection data » >
Inspection data
The final stage of confirming the suspected diagnosis is the analysis of the patient’s examination data.
When examining a patient using biomicroscopy, it is first necessary to assess the intactness of the cornea. Corneal lesions can be of various types.
- Small pinpoint infiltrates are characteristic of AVC.
- A lesion in the form of a “twig” corresponding to the course of the nerve ending indicates herpetic keratitis.
- A white, round infiltrate with the most common paralimbal localization indicates an allergic etiology of the process.
- A round infiltrate with a yellowish center is a sign of a bacterial process.
- If biomicroscopy reveals corneal erosion with torn edges, this indicates either a traumatic lesion or a deeper herpetic lesion such as “card-shaped” keratitis.
If the corneal lesion is not determined, it is necessary to pay attention to the condition of the eyelid conjunctiva. The nature of folliculosis is decisive for a number of pathologies.
- Thus, the presence of large homogeneous follicles located in rows in the arch of the lower eyelid is most often a manifestation of chlamydial conjunctivitis.
- Medium or mixed (medium in combination with small) folliculosis speaks in favor of AVC.
- The detection of multiple small follicles is a characteristic sign of an allergic process or dry eye syndrome.
- The presence of complaints in the absence of a clinical picture of folliculosis often occurs with long-term dry eye syndrome.
- Folliculosis may be completely absent in bacterial conjunctivitis.
The presented differential diagnostic algorithm can only serve as the basis for express analysis of examination data. For a complete and competent diagnosis, a combination of step-by-step analysis of patient survey data (complaints, anamnesis) and examination results is required.
Surveys
- It is necessary to carefully examine the affected eye and eyelids: pay attention to the presence of exudate, redness, the condition of the cornea and anterior chamber of the eye. If a superficially located foreign body is detected, remove it; if chemically active liquids come into contact, rinse the eye thoroughly with plenty of water.
- Determination of visual acuity, according to Sivtsev’s table
- Direct and indirect reaction of the pupil to light
- Ophthalmoscopy
- Transmitted light examination (pink reflex): presence of turbulent inclusions in the cornea, anterior chamber of the eye, vitreous body
- Violet filter ophthalmoscopy after fluorescein staining of the cornea (to diagnose corneal damage)
- (if necessary) study of the reaction of photophobia and pain after instillation of a local anesthetic
- Ophthaltometry
- Eye movements and eyeball position (only for blunt eye trauma)
Evaluation of the information received:
- Decreased visual acuity: keratitis, iridocyclitis, glaucoma or trauma.
- Corneal clouding: keratoconjunctivitis.
- Retention of contrast (fluorescein drops) on the cornea: corneal erosion or ulcer in keratoconjunctivitis due to superficial trauma.
- Tree-like ulceration of the cornea: herpetic keratitis.
- A narrow pupil, sometimes losing its spherical shape, there may be clouding in the anterior chamber of the eye, hypopyon, discoloration of the iris - iridocyclitis. Impaired direct or indirect reaction to light; pain that does not go away after adding local anesthetic; changes in visual acuity and light perception accompany iridocyclitis.
- Severe headache, nausea, vomiting, redness of the eye, decreased visual acuity, clouding of the cornea and a wide pupil frozen in one position: an acute attack of glaucoma. If in doubt, it is necessary to palpably compare the intraocular pressure with the other eye.
- In case of severe eye injury, the following are noted: decreased visual acuity, changes in the pupils, blood in the anterior chamber of the eye, clouding of the transparent media of the eye, changes in the movements of the eyeballs and the position of the eyes.
Differential diagnosis:
- in newborns, gonorrheal conjunctivitis, starting from the third day of life and chlamydial or herpetic - from the tenth day; with prolonged and significant accumulation of purulent exudate, assume a congenital disorder of the outflow of tear fluid;
- episcleritis (localized redness, deep and superficial, with local pain on palpation, with the conjunctiva intact;
- subconjunctival hemorrhage (sharply limited red varnish color, painless redness of the eyeball).
| Conjunctivitis Iridocyclitis Keratitis O. attack of glaucoma By type of injection Mixed, straight, blood-filled vessels. Red eye syndrome is a symptom complex that develops with inflammatory damage to the eyelids, tear ducts, conjunctiva or cornea. Clinically, the disease is manifested by hyperemia, increased tearing, swelling, pain, and visual dysfunction. To establish the causes of development, biomicroscopy, visometry, perimetry, ultrasound, gonioscopy, tonometry, and ophthalmoscopy are performed. Conservative therapy includes the use of antibacterial drugs, NSAIDs, glucocorticosteroids, antihistamines, mydriatics and antiseptics. |
Pathogenesis of red eye syndrome
All structures of the eye need nutrients that come along with the blood through the vessels. If the walls of blood vessels expand and stretch greatly, they are filled with more blood than required. A vascular pattern begins to appear on the surface of the sclera. Due to the transparency of the mucous membrane, it is very clearly visible. Dilatation of blood vessels can lead to thinning of their walls. This becomes a predisposing factor to hemorrhages. Redness occurs in different parts of the protein membrane. Sometimes they cover the entire sclera, in some cases they are localized in the corners of the eyes.
Symptoms of red eye syndrome
The syndrome develops in three stages. In the first, superficial, redness is noticeable on the periphery of the conjunctival sac, which indicates hyperemia - overcrowding of blood vessels. You need to visit an ophthalmologist in the next 1-2 days. At the deep (ciliary) stage, a bright red border forms around the limbus, the junction of the cornea and the sclera. This suggests that inflammation is occurring inside the eye. The mixed stage is accompanied by hyperemia of the vessels of the mucous membrane and sclera around the limbus. If you notice a symptom, consult your doctor immediately. This is the big picture. Each pathology has its own symptoms.
With episcleritis, redness is usually one-sided; they develop in parallel with such signs as irritation and lacrimation. Scleritis is accompanied by acute pain in the eye and profuse tear production. An attack of glaucoma is manifested by pain, nausea, the appearance of halos around light sources, clouding of the cornea and decreased visual acuity. With uveitis, photophobia develops and flashes appear before the eyes. The vascular pattern is pronounced. Allergic reactions are almost always accompanied by itching, burning in the eyes, and tearing.
Stages of the syndrome and disease
There are three stages of red eye syndrome:
- Superficial. Swelling in the area of the conjunctival sac.
- Deep. Inflammation inside the eye.
- Mixed. The combination of the first three.
Edema can be infectious or non-infectious. Infectious edema is discussed in more detail below. Depending on the location of the edema, there are diagnoses in medicine.
Conjunctivitis
This is an inflammation of the conjunctiva (the transparent layer of the eyeball and the inside of the eyelid). The following types are distinguished:
- Bacterial (redness, swelling is small and barely noticeable, hemorrhages of a single distribution).
- Hemorrhagic (noticeable hemorrhages on the eyeball and eyelids).
- Adenoviral (lacrimation, pinpoint hemorrhages). The cause is infection of the upper respiratory tract.
- Allergic (symptoms directly depend on the source of the allergy).
- Atopic (seasonal, pain, photophobia, redness, swelling). Most often as an addition to rhinitis.
- Fungal. Sources of infection: humans, animals, fruits and vegetables.
Keratitis, cellulitis and abscess
This is an inflammation of the cornea. There is superficial and internal. Symptoms: narrowing of the palpebral fissure as a result of swelling, lacrimation, itching, pain.
Cellulitis and abscess are inflammation of the orbit. The cause of infection is infection. General symptoms: redness of the eyelids, soreness, swelling, decreased vision. In addition, phlegmon is characterized by the following: increased body temperature, headaches, eyes do not open or with difficulty. With an abscess, ulcers form.
Tenonite
This is inflammation in the Tenon's part. Tenonitis is a disease that occurs as a result of a previous illness: influenza, sinusitis, sore throat.
There are purulent and serous. The second is the result of an allergy. Symptoms: swelling, pain. The difference between types lies in the presence (or absence) of an abscess.
Stye, blepharitis, herpetic infection, chalazion
Inflammation can appear on the upper, lower, or both eyelids at once. All these eye diseases have common symptoms, swelling and redness. Causes: micromites, high sugar levels, problems with the gastrointestinal tract and immune system. Consequences: loss or deformation of eyelash growth, eye inflammation, itching, lacrimation.
Uveitis and dacryocystitis
Uveitis is inflammation of blood vessels. There are anterior (iridocyclitis) and posterior (chorioretinitis). Signs: photophobia, blurred vision, pain. Causes: high sugar content, infectious diseases, rotavirus infection.
Dacryocystitis is an inflammation of the tear ducts as a result of their obstruction. Symptoms: swelling, redness, pain in the corners. Causes: trauma, infectious eye diseases.
Diagnosis of red eyes
To establish an accurate diagnosis, a complete examination is required. After collecting anamnesis, a primary ophthalmological examination is performed, including:
- visual acuity test;
- assessment of the oculomotor system;
- slit lamp examination;
- eye pressure test;
- fundus examination.
Bacteriological analysis is carried out if an infectious disease is suspected. The composition of the tear film is determined using the Schirmer test - this is a test using special paper strips. Other diagnostic methods may be required: gonioscopy, ultrasound of the eye.
Diagnostics and examination methods
Methods and techniques for eye examination in modern ophthalmology make it possible to accurately and quickly identify the cause of eye redness and prescribe competent and effective treatment.
After examining and collecting an anamnesis (history of the disease), studying the patient’s complaints, the doctor will prescribe tests and examination methods necessary in this particular situation.
Modern methods of diagnostic examination of patients with eye diseases:
- Biomicroscopy is a visual examination of the structures of the eye using a slit lamp (SL).
The method allows you to examine in detail the fundus, lens, anterior chamber, vitreous body, sclera, iris, conjunctiva, and identify most eye diseases in the early stages of development.
In addition, biomicroscopy allows you to detect traumatic perforations of the eyeball, small foreign bodies that are not detected by x-ray examination, for example: glass, eyelashes, coal dust particles.
- Visometry is a method of testing visual acuity using tables with printed letters, symbols or drawings (for young children).
- Tonometry is a method of measuring intraocular pressure.
- The Norn test and the Schirmer test allow you to assess the fullness of the tear production function.
- Fluorescein test is a method for identifying defects in the conjunctiva and cornea of the eye using a fluorescein solution. Based on the ability of the indicator to color damaged areas.
Treatment of red eye syndrome
There is no general approach to treating the syndrome, as it is caused by various reasons. The doctor’s task is to identify the pathology, if any. In accordance with what factor, that is, the disease, manifests itself in the “red eye” syndrome, treatment is prescribed. In case of allergic conjunctivitis, it is necessary to eliminate the allergen. Symptoms of the disease are relieved with anti-allergic ophthalmic drops. Viral forms of the disease require antibacterial and antiviral therapy. For glaucoma, beta blockers, carbonic anhydrase inhibitors, pilocarpine and other drugs are taken. When they do not bring a positive effect, surgery is prescribed.
You almost always need to take vitamins and medications containing antioxidants and mineral complexes. Vitamin A strengthens the immune system, ascorbic acid has a healing effect. Some pathologies are treated using physiotherapeutic procedures. These include ultrasound, laser, and magnetic stimulation. Folk remedies - herbs, infusions, lotions - can only be used after consultation with a doctor. Otherwise, they can aggravate the situation and cause complications. In any case, you should not self-medicate. If the symptoms of the syndrome do not go away, appear too often, or are accompanied by other symptoms, visit the clinic.
Treatment
Each type of disease requires an individual approach and a special drug course of treatment. Each of them may include the following groups of drugs:
- antibacterial and anti-inflammatory;
- glucocorticosteroids;
- mydriatics;
- antiseptic and histamine;
- vitamins.
If you find an error, please select a piece of text and press Ctrl+Enter.
11/23/201702/12/2018 eye diseases, ophthalmology, red eyes, red eye syndrome
What complications does red eye syndrome cause?
Lack of treatment can subsequently cause complete loss of vision. Such complications are rare, but no one is immune from them. The syndrome should not be ignored under any circumstances. Blindness can be caused by keratitis and scleritis. Dry eye syndrome in its advanced form leads to corneal clouding, scarring, and amblyopia. Long-term and ineffective treatment of iridocyclitis causes overgrowth of the pupillary opening. Because of this, the outflow of aqueous humor from the eye is disrupted. This becomes the cause of glaucoma. In most cases, red eye syndrome is not serious. It is only important to identify its etiology in time and begin treatment.