Urine is a metabolic product formed in the kidneys as a result of filtration of the liquid part of the blood, as well as the processes of reabsorption and secretion of various analytes. It consists of 96% water, the remaining 4% comes from nitrogenous products of protein metabolism dissolved in it (urea, uric acid, creatinine, etc.), mineral salts and other substances.
A general urine test in children and adults includes assessment of the physicochemical characteristics of urine and sediment microscopy. This study allows you to evaluate the function of the kidneys and other internal organs, as well as identify the inflammatory process in the urinary tract
Physicochemical studies of urine include assessment of the following indicators:
- color;
- urine clarity;
- specific gravity (relative density);
- pH;
- protein concentration;
- glucose concentration;
- bilirubin concentration;
- urobilinogen concentration;
- concentration of ketone bodies;
- nitrite concentration;
- hemoglobin concentration.
Microscopy of urinary sediment includes assessment of the following objects:
- Organized urine sediment: presence of red blood cells;
- leukocytes;
- epithelial cells;
- cylinders;
- bacteria;
- yeast fungi;
- parasites;
- tumor cells;
Physicochemical characteristics
The assessment of the physical properties of urine, such as odor, color, turbidity, is carried out using the organoleptic method. The specific gravity of urine is measured using a urometer, a refractometer, or assessed using “dry chemistry” methods (test strips) - visually or on automatic urine analyzers.
Urine color
An adult's urine is yellow. Its shade can vary from light (almost colorless) to amber. The saturation of the yellow color of urine depends on the concentration of substances dissolved in it. With polyuria, urine has a lighter color; with a decrease in diuresis, it acquires a rich yellow tint. The color changes when taking medications (salicylates, etc.) or eating certain foods (beets, blueberries).
Pathologically changed color of urine occurs when:
- hematuria – a type of “meat slop”;
- bilirubinemia (beer color);
- hemoglobinuria or myoglobinuria (black);
- leukocyturia (milky white color).
Urine clarity
Normally, freshly collected urine is completely clear. Turbidity of urine is due to the presence in it of a large number of cellular formations, salts, mucus, bacteria, and fat.
Urine smell
Normally, the smell of urine is not strong. When urine decomposes by bacteria in the air or inside the bladder, for example in the case of cystitis, an ammonia odor appears. Rotted urine that contains protein, blood, or pus, such as from bladder cancer, causes the urine to smell like rotten meat. If there are ketone bodies in the urine, the urine has a fruity odor, reminiscent of the smell of rotting apples.
Urine reaction
The kidneys excrete “unnecessary” substances from the body and retain necessary substances to ensure the exchange of water, electrolytes, glucose, amino acids and maintain acid-base balance. The reaction of urine - pH - largely determines the effectiveness and characteristics of these mechanisms. Normally, the urine reaction is slightly acidic (pH 5.0–7.0). It depends on many factors: age, diet, body temperature, physical activity, kidney condition, etc. The lowest pH values are in the morning on an empty stomach, the highest are after meals. When eating mainly meat foods, the reaction is more acidic, when eating plant foods, the reaction is alkaline. When standing for a long time, urine decomposes, ammonia is released and the pH shifts to the alkaline side.
An alkaline urine reaction is characteristic of chronic urinary tract infection and is also observed with diarrhea and vomiting.
The acidity of urine increases in feverish conditions, diabetes mellitus, tuberculosis of the kidneys or bladder, and renal failure.
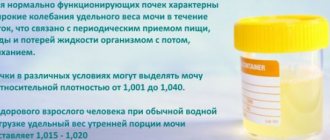
Specific gravity (relative density) of urine
Relative density reflects the functional ability of the kidneys to concentrate and dilute urine. Normally functioning kidneys are characterized by wide fluctuations in the specific gravity of urine during the day, which is associated with periodic intake of food, water and fluid loss from the body. The kidneys under various conditions can excrete urine with a relative density of 1.001 to 1.040 g/ml.
There are:
- hyposthenuria (fluctuations in the specific gravity of urine less than 1.010 g/ml);
- isosthenuria (the appearance of a monotonous specific gravity of urine corresponding to that of primary urine (1.010 g/ml);
- hypersthenuria (high specific gravity values).
The maximum upper limit of the specific gravity of urine in healthy people is 1.028 g/ml, in children – 1.025 g/ml. The minimum lower limit for urine specific gravity is 1.003–1.004 g/ml.
To assess the chemical composition of urine, diagnostic test strips (the “dry chemistry” method), produced by different manufacturers, are currently usually used. The chemical methods used in test strips are based on color reactions that produce a change in the color of the test area of the strip at different concentrations of the analyte. Discoloration is determined visually or by reflectance photometry using semi-automated or fully automated urine analyzers, and the results are assessed qualitatively or semi-quantitatively. If a pathological result is detected, the study can be repeated using chemical methods.
Protein
Protein is normally absent in urine or present in concentrations undetectable by conventional methods (traces). Several types of proteinuria (the appearance of protein in the urine) are identified:
- physiological (orthostatic, after increased physical activity, hypothermia);
- glomerular (glomerulonephritis, the action of infectious and allergic factors, hypertension, cardiac decompensation);
- tubular (amyloidosis, acute tubular necrosis, interstitial nephritis, Fanconi syndrome).
- prerenal (myeloma, muscle tissue necrosis, erythrocyte hemolysis);
- postrenal (for cystitis, urethritis, colpitis).
Glucose
Normally, there is no glucose in the urine. The appearance of glucose in the urine can have several reasons:
- physiological (stress, intake of increased amounts of carbohydrates);
- extrarenal (diabetes mellitus, pancreatitis, diffuse liver damage, pancreatic cancer, hyperthyroidism, Itsenko-Cushing's disease, traumatic brain injury, stroke);
- renal (renal diabetes, chronic nephritis, acute renal failure, pregnancy, phosphorus poisoning, certain medications).
Bilirubin
Bilirubin is normally absent in urine. Bilirubinuria is detected in parenchymal liver lesions (hepatitis), obstructive jaundice, cirrhosis, cholestasis, as a result of the action of toxic substances.
Urobilingen
Normal urine contains low concentrations (traces) of urobilinogen. Its level increases sharply with hemolytic jaundice, as well as with toxic and inflammatory lesions of the liver, intestinal diseases (enteritis, constipation).
Ketone bodies
Ketone bodies include acetone, acetoacetic and beta-hydroxybutyric acids. An increase in the excretion of ketones in the urine (ketonuria) occurs when carbohydrate, lipid or protein metabolism is disturbed.
Nitrites
There are no nitrites in normal urine. In urine, they are formed from nitrates of food origin under the influence of bacteria, if the urine was in the bladder for at least 4 hours. The detection of nitrites in properly stored urine samples indicates infection of the urinary tract.
Hemoglobin
Normally absent in urine. Hemoglobinuria - the result of intravascular hemolysis of red blood cells with the release of hemoglobin - is characterized by the release of red or dark brown urine, dysuria, and often lower back pain. With hemoglobinuria, there are no red blood cells in the urine sediment.
Microscopy of urine sediment
Urine sediment is divided into organized (elements of organic origin - red blood cells, leukocytes, epithelial cells, casts, etc.) and unorganized (crystals and amorphous salts).
Research methods
The study is carried out visually in the native preparation using a microscope. In addition to visual microscopic examination, research using automatic and semi-automatic analyzers is used.
Red blood cells
During the day, 2 million red blood cells are excreted in the urine, which, when examining urine sediment, is normally 0–3 red blood cells per field of view for women and 0–1 red blood cell per field of view for men. Hematuria is an increase in red blood cells in the urine above the specified values. There are macrohematuria (the color of urine is changed) and microhematuria (the color of urine is not changed, red blood cells are detected only by microscopy).
In urinary sediment, red blood cells can be unchanged (containing hemoglobin) and changed (deprived of hemoglobin, leached). Fresh, unchanged red blood cells are characteristic of urinary tract lesions (cystitis, urethritis, stone passage).
The appearance of leached red blood cells in the urine is of great diagnostic importance, because they are most often of renal origin and occur in glomerulonephritis, tuberculosis and other kidney diseases. To determine the source of hematuria, a three-glass sample is used. When bleeding from the urethra, hematuria is greatest in the first portion (unchanged red blood cells), from the bladder - in the last portion (unchanged red blood cells). With other sources of bleeding, red blood cells are distributed evenly in all three portions (leached red blood cells).
Leukocytes
White blood cells are found in small quantities in the urine of a healthy person. The norm for men is 0–3, for women and children 0–6 leukocytes per field of view.
An increase in the number of leukocytes in the urine (leukocyturia, pyuria) in combination with bacteriuria and the presence of clinical symptoms indicates inflammation of an infectious nature in the kidneys or urinary tract.
Epithelial cells
Epithelial cells are almost always found in urinary sediment. Normally, a urine test shows no more than 10 epithelial cells per field of view.
Epithelial cells have different origins:
- squamous epithelial cells enter the urine from the vagina, urethra, their presence has no special diagnostic significance;
- transitional epithelial cells line the mucous membrane of the bladder, ureters, pelvis, and large ducts of the prostate gland. The appearance of a large number of such epithelial cells in the urine can be observed with urolithiasis, neoplasms of the urinary tract and inflammation of the bladder, ureters, pelvis, large ducts of the prostate gland;
- renal epithelial cells are detected in cases of damage to the kidney parenchyma, intoxication, febrile, infectious diseases, and circulatory disorders.
Cylinders
The cylinder is a protein that is coagulated in the lumen of the renal tubules and includes in its matrix any contents of the lumen of the tubules. The cylinders take the shape of the tubules themselves (cylindrical cast). Normally, there are no casts in a urine sample taken for general analysis. The appearance of casts (cylindruria) is a symptom of kidney damage.
Cylinders are distinguished:
- hyaline (with overlay of erythrocytes, leukocytes, renal epithelial cells, amorphous granular masses);
- granular;
- waxy;
- pigmented;
- epithelial;
- erythrocyte;
- leukocyte;
- fatty.
Unorganized sediment
The main component of unorganized urine sediment is salts in the form of crystals or amorphous masses. The nature of the salts depends on the pH of the urine and other properties of the urine. For example, with an acidic reaction of urine, uric acid, urates, oxalates are detected, with an alkaline reaction of urine - calcium, phosphates, ammonium urate. Disorganized sediment does not have any particular diagnostic significance; one can indirectly judge the patient’s propensity for urolithiasis. In a number of pathological conditions, crystals of amino acids, fatty acids, cholesterol, bilirubin, hematoidin, hemosiderin, etc. may appear in the urine.
The appearance of leucine and tyrosine in the urine indicates a severe metabolic disorder, phosphorus poisoning, destructive liver disease, pernicious anemia, and leukemia.
Cystine is a congenital disorder of cystine metabolism - cystinosis, liver cirrhosis, viral hepatitis, hepatic coma, Wilson's disease (congenital defect of copper metabolism).
Xanthine – xanthinuria is caused by the absence of xanthine oxidase.
Bacteria
Normally, urine in the bladder is sterile. When urinating, germs from the lower urethra enter it.
The appearance of bacteria and leukocytes in a general urine analysis against the background of symptoms (dysuria or fever) indicates a clinically manifested urinary infection.
The presence of bacteria in the urine (even in combination with leukocytes) in the absence of complaints is regarded as asymptomatic bacteriuria. Asymptomatic bacteriuria increases the risk of urinary tract infection, especially during pregnancy.
Yeast mushrooms
The detection of fungi of the genus Candida indicates candidiasis, which most often occurs as a result of irrational antibiotic therapy, the use of immunosuppressants, and cytostatics.
Parasites
In the urine sediment, blood schistosome eggs (Schistosoma hematobium), elements of the echinococcal bladder (hooks, scolex, brood capsules, fragments of the bladder shell), migrating larvae of intestinal eels (strongylides), washed off with urine from the perineum of the oncosphere of taeniids, pinworm eggs (Enterobius vermicularis) can be found ) and pathogenic protozoa - Trichomonas (Trichomonas urogenitalis), amoebas (Entamoeba histolitika - vegetative forms).
Urinalysis, three-glass sample: preparation for the study
Before this test, it is recommended to refrain from urinating for 3-5 hours. Therefore, urine collected in the morning is ideal. After you finish toileting the genitals (warm water, without using any soap), you need to collect urine in a clean, preferably sterile container in the usual way, but at the same time dividing the entire volume into 3 unequal portions. Before taking the latter, if the reason for urine analysis is possible prostatitis, which needs to be diagnosed, you should massage the prostate.