Changed urine color with prostatitis
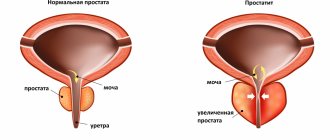
The male gland contains the urethral canal. It is in it that inflammatory and pathological processes occur. The thickness and color of urine changes in chronic prostatitis, accompanied by malfunctions of the genitourinary organs during functioning. The presence of inflammation is possible if the following characteristic signs are found:
- Urine is orange when the number of red blood cells is increased. This means that the patient eats certain types of foods or takes medications. But when prostatitis is detected, red blood cells in the urine also exceed the permissible limits.
- Urine is red in case of prostatitis that has passed into the acute phase, and other problems in this area. A changed shade indicates the development of pyelonephritis or the presence of stagnant blood after prostate injury.
- Pink color indicates fresh blood present in the urine. It is possible to diagnose prostate cancer.
- Clots and characteristic thread-like inclusions gradually settle, and the color of urine with prostatitis in men indicates the beginning of a purulent process with increased temperature and pain when urinating. Urgent medical attention is required, as an abscess may form and peculiar “sacs” filled with pus will spread.
- Whitish flakes indicate the presence of protein in the urine with prostatitis and related kidney and bladder problems. The excreted fluid changes structure if severe pyelonephritis and cystitis develop - constant companions of the purulent form of prostatitis.
- Sticky urine characterizes immunodeficiency that has developed in the patient’s body for many reasons, which include chronic prostatitis, cancer and other disorders.
- Sediment in foamy and cloudy urine with chronic prostatitis can signal the onset of cancer. The liquid has a high density.
Urine in chronic prostatitis changes its normal appearance and becomes like a thick and cloudy jelly, with floating thread-like whitish inclusions. If the problem has been troubling the patient for a long time, then he has a serious reason to consult a specialist to diagnose the health of the prostate gland and the entire body. The results of the study will accurately show the possibility of developing pathology in the urinary canal.
Decoding the results
A general urine test for prostatitis has the following indicators:
- Normal density is 1020-1022 g/l, deviations indicate pathologies.
- Acidity 5-7.
- Epithelial cells are normally absent or present in small quantities.
- Bilirubin and ketone bodies are normally absent.
- There are normally no blood spots.
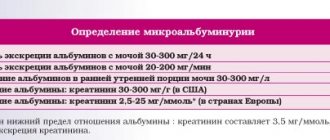
- Protein in the urine indicates prostatitis or kidney pathology at a concentration above 0.033 g/l. Normally this indicator is 0.
- Red blood cells are present in numbers of more than one per field of view. The indicator may also indicate oncology. Normally it is 0.
- Leukocytes in the urine with prostatitis are in the amount of 4 or more units in the field of view.
- In the calculous form of inflammation, phosphates are also present in the urine.
A urine test after prostate massage may give incorrect results. In addition, it is influenced by many other factors, so most often the analysis is ordered again after some time. This increases the information content and allows for a more accurate diagnosis.
What do urine tests tell you about chronic prostatitis?
A study conducted at a professional level helps to determine the threat of developing pathology at the first stage. If a urine test for prostatitis in men showed the presence of foreign microorganisms that are completely absent in the normal state, it means that the tissues of the urinary tract are inflamed. The presence of red blood cells in prostatitis is almost always determined in a urine test.
The diagnosis of “prostatitis” by urine analysis is established with an accuracy of up to 60%. In other situations, malfunctions in the genitourinary system will tell the doctor about renal failure in the patient, who may suffer from cystitis, complicated by inflammation of the urethra.
Clinical changes in a general urine test for prostatitis and other diseases may not be detected. The doctor uses research results for differential diagnosis when instrumental examination methods are indispensable. The result of a general urine test for prostatitis will help determine:
- characteristics of physical properties obtained during inspection of the sample,
- The volume of fluid per day decreases in pathological disorders, and urine collection becomes more difficult, until the process of urination completely disappears.
According to the signs and symptoms that can be determined by laboratory analysis of urine for prostatitis, indicators indicate the development of an inflammatory process. A man experiences pain in the toilet, it hurts him to have sex, and dysuric disorders increase the risk of prostatitis by up to 70-80%.
Studying the composition of urine does not make it possible to accurately diagnose prostatitis; urine can only determine the presence of an infectious agent. Although these data are very important for identifying the onset of the inflammatory process for establishing a diagnosis and prescribing an optimal treatment regimen.
Chronic prostatitis, known to medicine for more than a hundred years, remains at present a very common, insufficiently studied and difficult to treat disease. It affects predominantly young and middle-aged men, i.e., the most sexually active, and is often complicated by impaired copulatory and generative functions.
Obviously, not only the medical, but also the social significance of the problem of increasing the efficiency of diagnosis and treatment of chronic prostatitis.
Most experts believe that chronic prostatitis is an inflammatory disease of infectious origin with the possible addition of autoimmune disorders, characterized by damage to both parenchymal and interstitial tissue of the prostate gland.
Information on the epidemiology of chronic prostatitis is limited and contradictory. According to domestic authors, it affects from 8 to 35% of men aged 20–40 years. The leading expert on this issue, J. Nickel (1999), believes that approximately 9% of the male population has manifestations of prostatitis, of which 2/3 seek medical help.
Etiology, pathogenesis
Modern medicine does not have in-depth and reliable information about the causes and mechanisms of development of chronic prostatitis, especially abacterial. In most cases of chronic prostatitis, its etiology, pathogenesis and pathophysiology remain unknown.
The existence of bacterial and abacterial prostatitis is now recognized. However, it is not clear whether the process can be initially abacterial or whether the disease, having begun as a result of the penetration of infectious agents into the gland, subsequently proceeds without their participation, i.e., passes through infectious and post-infectious phases. Obviously, it is impossible to identify microorganisms cultured from prostate secretions with the etiological factor of the disease, since in most cases this flora is saprophytic, relatively pathogenic, or a consequence of contamination with the contents of the urethra.
The frequency of certain types of prostatitis, according to summarized literature data, is: acute bacterial prostatitis – 5–10%, chronic bacterial prostatitis – 6–10%; chronic abacterial prostatitis – 80–90%, including prostatodynia – 20–30%.
Reputable microbiological studies indicate that the most common causes of chronic bacterial prostatitis are gram-negative microbes; gram-positive bacteria are rare. Most experts who have studied this issue include chlamydia, ureaplasma, anaerobic bacteria, fungi, and Trichomonas as possible causative infectious agents of abacterial prostatitis.
We believe that in our country there is a sharp overdiagnosis of urogenital chlamydia, mycoplasmosis, caused, among other things, by its variety - ureaplasma, as well as bacterial vaginosis (gardnerellosis). The following arguments confirm this.
The difficulties of identifying these pathogens and the lack of completely reliable tests are obvious. Non-cultural methods, which are predominantly used in practice, are clearly not reliable enough. Doctors often experience uncertainty and awkwardness when determining treatment tactics in situations where the patient’s pathogens are identified by some tests as sexually transmitted infections (STIs), but not by others; in one laboratory they were detected, in another - not, in one of the sexual partners they were detected, in the other - not.
STIs in men primarily and predominantly affect the urethra. All of the above applies mainly to urethritis. The question of the etiology of chronic inflammatory lesions of the accessory sex glands is even more complex. Most foreign experts believe that chlamydia, mycoplasma and trichomonas are only probable etiological factors of chronic prostatitis. The causative role of gardnerella and viruses has not been proven at all.
The role of these microorganisms in the genesis of chronic inflammatory lesions of the accessory sex glands and infertility in men is given too much importance. This is influenced by two factors. Firstly, having discovered, for example, chlamydia in material obtained from the urethra, the doctor makes a conclusion about the chlamydial nature of prostatitis, and secondly, the likelihood of contamination of the ejaculate and prostate secretion by the microflora of the urethra is not taken into account.
In the domestic specialized literature, a strong opinion has formed about the resistance of a number of STI pathogens, primarily chlamydia, to antibacterial drugs. This is fundamentally different from the point of view of leading foreign experts. One of the reasons for the false-positive interpretation of research results is that after an adequate course of ABT, rapid elimination of chlamydia does not occur; their antigens and DNA continue to persist in the genitourinary system for up to 3 weeks. During this period, the results of immunofluorescent and enzyme immunoassay methods, as well as polymerase chain reaction, may be positive. Another kind of misconception is that the absence of a rapid or any clinical effect after ABT, which is natural for any chronic inflammation, is interpreted as the persistence of the microbial agent.
We believe that specialists should be alarmed not only by the frequency of STIs, but also, no less, by overdiagnosis and exaggeration of antibacterial resistance of urogenital chlamydia, mycoplasmosis, bacterial vaginosis, as well as their role in the genesis of inflammatory lesions of the accessory gonads and male infertility. Due to these errors, long, repeated and completely unjustified courses of antibacterial therapy, which are prescribed to young people, not only to falsely infected people, but also to their sexual partners, have become our daily practice.
Our answer to the question “what to do?”, given the current state of knowledge, is as follows:
- firstly, expect the creation and implementation of more reliable laboratory methods for identifying STI pathogens, facilitating this as far as possible;
- secondly, the diagnosis of urogenital chlamydia, mycoplasmosis, ureaplasmosis is considered valid if the results of several complementary laboratory tests are positive;
- thirdly, take into account that in the presence of an active inflammatory process and the absence of clear laboratory data on the nature of the infectious agent, the most likely causative agent of urethritis and prostatitis is chlamydia. In such cases, carry out antibacterial therapy, including 1-2 courses of drugs of the appropriate spectrum of action, and then general and local anti-inflammatory effects.
The most likely route of infection of the prostate is ascending or urogenital, with a high frequency of a combination of urethritis and prostatitis. Lymphogenous (from the rectum and urethra), hematogenous, and routes of pathogen penetration associated with endourethral manipulation are also possible. The possibility of infection of the prostate by urine microflora has been discussed for a long time. R. Kirby et al. (1982), using a carbon suspension, proved the existence of urinary reflux into the prostate ducts. In this case, not only infection of the prostate is possible, but also the influence of urine as a chemical agent that can cause and maintain an abacterial inflammatory process. Reflux of urine into the excretory ducts of the prostate was confirmed by W. Hellstrom et al. (1987), E. Meares (1992). There is an assumption that this reflux may occur against the background of turbulent movement of urine in the prostatic urethra due to insufficient opening of the bladder neck of various origins.
Classic studies on the anatomy of the prostate gland have shown the feasibility of dividing it, taking into account the characteristics of the ducts, stroma and epithelium, into a central zone located cranially and a peripheral zone located caudally. The acini tubules of the central zone flow into the urethra almost parallel to the flow of urine, and the peripheral ones - at a right or acute angle. This circumstance apparently determines the development of the inflammatory process mainly in the peripheral zone of the prostate.
A number of factors predispose to the development of chronic prostatitis. These include close vascular and lymphatic connections with other organs, structural features of the prostatic glands that impede their complete drainage, pathological changes in the pelvic organs and nervous structures leading to venous stasis, impaired microcirculation and autonomic innervation of the prostate (A.S. Segal et al. ., 1983; M.I. Kaplun, 1984; I.F. Yunda, 1987; V.N. Tkachuk et al., 1989, 1994; O.L. Tiktinsky, 1990; N.A. Lopatkin, 1998; V A. Molochkov, I. I. Ilyin, 1998; N. I. Tarasov et al., 1999; O. L. Tiktinsky, V. V. Mikhailichenko, 1999; J. Nickel, 1999).
In chronic prostatitis, the barrier function of the prostate is disrupted (the content of zinc and lysozyme decreases), all parts of the immune system suffer: phagocytic, cellular (decrease in absolute and relative indicators of T-lymphocytes and their subpopulation - T-helpers), humoral (increase in the content of antigen-specific immunoglobulins in prostate secretions – IgA and IgG). Having begun as an infectious-inflammatory process, the further persistent course of chronic prostatitis is supported by autoimmune mechanisms. The reality of the existence of autoaggression is confirmed by the detection of circulating serum autoantibodies to prostate tissue and the deposition of immune complexes in the affected tissue (I.I. Ilyin, 1970, 1994; M.I. Ukhal, 1984; V.P. Chernyshev, 1984; G.N. Drannik et al., 1986; Yu.N. Kovalev, 1987, 1995; N.I. Tarasov et al., 1999).
Classification, diagnosis
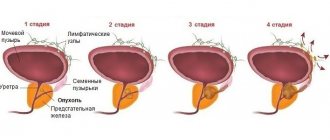
- Various authors, including domestic ones, have proposed several classifications of chronic prostatitis. The most common abroad and, in our opinion, correct classification of prostatitis is currently proposed by the US National Institutes of Health (NIH, 1995).
- Category I. Acute bacterial prostatitis.
- Category II. Chronic bacterial prostatitis.
- Category III. Chronic abacterial prostatitis.
- Category III A. Chronic inflammatory pelvic pain syndrome.
- Category III B. Non-inflammatory chronic pelvic pain syndrome (prostatodynia)
- Category IV. Asymptomatic inflammatory prostatitis.
We previously proposed to call the syndrome of non-inflammatory chronic pelvic pain neurovegetative prostatopathy (1983), meaning damage to the prostate gland due to disruption of its innervation and hemodynamics, which has symptoms similar to chronic prostatitis in the absence of signs of inflammation. In recent years, reports have appeared confirming our point of view about the specific role of detrusor-sphincter dyssynergia, activation of the sympathetic part of the autonomic pelvic innervation, as well as neurosis-like conditions in the genesis of prostatodynia.
We believe that this classification should be supplemented by a characteristic of the activity of the inflammatory process: the phases of active inflammation, latent and remission.
Currently, the desire of clinical medicine for maximum objectification and quantitative expression of indicators characterizing the patient’s condition is clearly manifested. Moreover, this applies not only to instrumental and laboratory studies, but also to information of a subjective nature. One of the features of chronic prostatitis is the paucity of detectable pathological changes. The main criteria for making a diagnosis (data from palpation of the prostate, laboratory tests and ultrasound) do not have a clear delineation and generally accepted interpretation. Of particular importance are the identification and objectification of complaints of a patient with chronic prostatitis, which are distinguished by diversity, uncertainty and psycho-emotional dependence.
We proposed (2001) a system for the summary assessment of symptoms of chronic prostatitis (SOS-CP). The system includes a number of indicators (questions) relating to the presence, severity and persistence of symptoms, as well as the quality of life of patients. This system does not include questions regarding copulative disorders, since they do not have a clearly defined relationship with chronic prostatitis and are subject to independent analysis using the ICF scale (O.B. Laurent, A.S. Segal, 1998). The questionnaire completed by the patient is analyzed by the doctor. First of all, the sum of the points scored is calculated for the main groups of questions: pain and paresthesia, dysuria and quality of life. Then the symptom index (SI-CP) is determined - the sum of points reflecting pain, dysuria and prostatorrhea. The last one to establish is the clinical index of chronic prostatitis (CI-CP) - the sum of indices of symptoms and quality of life. Depending on the severity of clinical manifestations, CI-CP can be divided into minor (0–10), moderate (11–25) and severe (26–50). Thus, all clinical manifestations of chronic prostatitis can be represented by the following numerical series: Pain = _____. Dysuria = ____. Quality of life = ____. Symptom Index (IS-CP) = ____. Clinical index (CI-CP) = ____. We are convinced that the developed system for the summary assessment of symptoms in chronic prostatitis (SOS-CP) simplifies the identification and analysis of patient complaints, makes it possible to quantify the symptoms of the disease, obtain a summary objective characteristic of the entire variety of clinical manifestations of the disease in a particular patient, expressing them in a digital series . It is very effective for monitoring the dynamics of patients’ condition and assessing the results of therapy.
Based on a systematic review of the literature on the problem of diagnosis and treatment of chronic abacterial prostatitis for 1966–1999, carried out taking into account the requirements and principles of evidence-based medicine (M. Collins, R. McDonald, T. Wilt, 2000), the authors came to the conclusion that Currently, there are no clear diagnostic criteria for chronic abacterial prostatitis, the quality of the methodology is low, and the most common methods of treatment (prescription of antibiotics and α1-blockers) require further study and analysis.
Palpation of the prostate gland and examination of its secretions remain of paramount importance in the diagnosis of chronic prostatitis.
Of the laboratory diagnostic methods, the “gold standard” remains the classic test by E. Meares and T. Stamey (1968): collecting the first and second portions of urine, obtaining prostate secretion by massage and then the third portion of urine. Based on microscopic and bacteriological indicators, the presence of an inflammatory process and its localization are determined. It should be remembered that not every microorganism isolated from prostate secretion or the third portion of urine should be considered as an etiological factor of prostatitis, taking into account the possibility of contamination of the material with urethral microflora. Consequently, the diagnosis of chronic bacterial prostatitis is confirmed by the results of bacteriological examination; only taking this into account is it possible to differentiate bacterial and abacterial prostatitis.
A number of physicochemical and biochemical changes in prostate secretion have been established, which serve as additional diagnostic criteria for identifying chronic prostatitis.
The capabilities of ultrasound sonography to confirm the diagnosis of chronic prostatitis are limited. Uroflowmetry is a simple and reliable way to determine the state of urodynamics in patients with chronic prostatitis; it allows you to promptly detect signs of bladder outlet obstruction and carry out dynamic monitoring (N.A. Lopatkin, 1998).
It is advisable to perform urethroscopy in all patients with long-term inflammatory process in the prostate gland. An endoscopic examination confirms or rejects concomitant urethritis and reveals changes in the mucous membrane of the prostatic urethra and seminal tubercle characteristic of inflammatory lesions of the prostate gland, which, according to our data, occur in approximately 70% of patients.
If urethral stricture or sclerosis of the bladder neck is suspected, urethrocystography is performed. Puncture biopsy of the prostate gland remains mainly a method of differential diagnosis of chronic prostatitis, prostate cancer and benign hyperplasia.
Treatment
It should be recognized that at present there are no sufficiently substantiated approaches to the treatment of chronic prostatitis. Treatment should be aimed at eliminating the infectious agent, normalizing the immune status, regressing inflammatory changes and restoring the functional activity of the prostate.
The basic principles of therapy include the following:
- impact on all parts of the etiology and pathogenesis of the disease;
- analysis and recording of activity, category and degree of prevalence of the process;
- application of a complex of therapeutic measures
Most experts consider the following indications for antibacterial therapy (ABT) for chronic prostatitis:
- chronic bacterial prostatitis;
- chronic abacterial prostatitis (category IIIA), if there is clinical, bacteriological and immunological evidence of prostate infection (“atypical microorganisms”).
Domestic specialists, much more often than foreign ones, use drugs that correct immune processes for chronic prostatitis.
The widespread use of non-steroidal anti-inflammatory drugs in patients with chronic prostatitis is completely justified and pathogenetically justified, and the rectal route of administration seems especially successful.
The effectiveness of enzyme preparations for chronic prostatitis has been repeatedly emphasized in the domestic literature.
A new approach in the treatment of chronic prostatitis is the use of a1-blockers; it was predetermined by the following circumstances:
- Elimination of lower urinary tract symptoms caused by BPH with these drugs;
- the presence of a large number of a1-adrenergic receptors in the prostate gland and bladder neck;
- the concept of the pathogenesis of the disease, based on the occurrence of turbulent urine flow in the prostatic urethra due to insufficient dilatation of the bladder neck;
- a number of researchers have described urination disorders in chronic prostatitis of a very different nature: from urination at low intravesical pressure to increased intravesical pressure (A.V. Sivkov, S.S. Tolstova et al., 2000, etc.).
- An increase in the activity of the sympathetic part of the pelvic innervation, including α1-adrenergic receptors, was detected in a number of cases of chronic abacterial prostatitis.
Based on the understanding of the mechanism of action of a1-adrenergic blockers and the changes described above that are characteristic of chronic abacterial prostatitis, the positive effect of the use of this group of drugs becomes clear. At the same time, their ability to influence individual links in the pathogenesis of the disease and lead to regression of symptoms is explained.
The use of a1-blockers for chronic prostatitis, which was initially empirical in nature and then increasingly substantiated, showed the effectiveness of this method of treatment and the prospects for its further use and study (D. Osborn et al., 1981; J. de la Rosette et al., 1992; D. Neal, T. Moon, 1994; G. Barbalis et al., 1998; A. S. Segal et al., 2000; V. N. Tkachuk, 2000; V. N. Tkachuk, S. Kh. Al-Shukri et al., 2000; A.V. Sivkov et al., 2002). Various α1-blockers have proven themselves to be positive, such as alfuzosin, doxazosin, terazosin, etc.
In our clinic, over the past 6 years, alfuzosin has been successfully used for chronic abacterial prostatitis at a dose of 5–10 mg per day for one to several months. We are convinced that the greatest effect in treatment with a1-blockers can be achieved in patients with chronic prostatitis with severe urination problems in the absence of an active inflammatory process.
An analysis of the literature shows that the effectiveness of a1-blockers in chronic prostatitis ranges from 48 to 80%, and the total positive result is 64% (J. Rosette et al., 1992).
We consider it most appropriate to prescribe a1-blockers for chronic prostatitis category III B (prostatodynia) in cases where dysuria predominates in the clinical picture, the treatment period is from 1 to 6 months. Moreover, they can be used both as monotherapy and in combination with other medications and treatments.
Among herbal remedies that have proven themselves in the treatment of chronic prostatitis, we should note imported preparations from Pygeum africanum and domestic ProstaNorm, consisting of extracts of four well-studied medicinal plants (A.S. Segal et al., 2000; L.M. Gorilovsky, M.A. Dobrokhotov, 2001).
We believe that in most cases of chronic prostatitis it is necessary to normalize the patient’s mental status using both medications and rational psychotherapy.
We would like to note that, while sharing the ideas of the Cochrane Collaboration, which aims to promote medical decision-making based on reliable facts, we are very reserved about the widespread use of a number of drugs that have appeared in recent years, including domestically produced immunocorrectors.
Domestic urologists, much more widely than foreign ones, use a variety of physiotherapeutic interventions to treat chronic prostatitis.
Along with the majority of domestic and foreign urologists, we believe that finger massage of the prostate gland can and should be used for chronic prostatitis, taking into account known indications and contraindications.
An independent problem is the treatment or correction of disorders of generative and copulative functions that arise as a result of chronic prostatitis or against its background. We, like most specialists at present, do not see an organic connection between chronic prostatitis and erectile dysfunction. Thus, all aspects of the problem of chronic prostatitis require further in-depth study.
D.Yu. Pushkar, A.S. Segal Department of Urology, Moscow State Medical and Dental University
Literature
- Krupin V.N. Urology. 2000; 5; 20–22.
- Guide to urology. Ed. ON THE. Lopatkina. T.2. M., 1998; With. 393–440.
- Laurent O.B., Segal A.S. Materials of the X Russian Congress of Urologists. M., 2002; pp. 209–222.
- Sivkov A.V., Tolstova S.S., Egorov A.A., etc. Materials of the All-Russian conference “Modern aspects of diagnosis and treatment of chronic prostatitis”. Kursk, 2000; With. 145–146.
- Tiktinsky O.L., Mikhailichenko V.V. Andrology. 1999; With. 109–223.
- Tkachuk V.N. Modern methods of treating patients with chronic prostatitis. A manual for doctors. St. Petersburg, 2000
Types of tests for accurate diagnosis of prostatitis
To identify inflammation in the prostate tissue, the doctor prescribes various examinations. The patient will have to give not one, but several urine samples at once. General changes in its structure are most clearly visible through a comprehensive analysis, which identifies pathogenic microbes and disorders in cells.
ORDER
Typically, the doctor prescribes a general urine test, cytological examination and samples to determine the bacteriological and infectious components. In case of a suspicious urine test for prostatitis, the indicators need to be clarified if the number of leukocytes and erythrocytes is significantly increased. The patient additionally undergoes a urine test for the prostate with changes according to Dr. Nechiporenko’s method. It will help identify concomitant diseases such as cystitis, urethritis and other pathologies.
OAM as the main research method
In case of deviations from the norm, the doctor must prescribe a detailed analysis as a diagnostic procedure. The main goal of this activity is to identify changes in color and structure in collected urine samples. The laboratory technician should pay attention to factors such as:
- appearance, changes in shade, smell, the presence of foreign organisms and an increase in density, which makes it possible to identify related diseases;
- physicochemical characteristics, including the level of acidity, which is 5-7 pH in the normal state of the body. Elevated levels indicate an inflammatory process, which will ultimately lead to the diagnosis of prostatitis;
- Biochemical composition.
During clinical studies, it is possible to reliably determine the number of leukocytes in the urine; with prostatitis, this figure increases significantly. An increase in the amount of oxalates, protein and red blood cells in the urine with prostatitis is very likely, and the doctor may suspect infectious or calculous prostatitis in an acute form.
Urine in the prostate may become cloudy due to inflammation of the genitourinary system. Therefore, a general analysis makes it possible to characterize the patient’s general condition. Cloudy urine is highly likely to indicate a diagnosis of prostatitis.
Now everyone knows what kind of urine for prostatitis will help determine the exact form of inflammation, which occurs as a purulent process in chronic or acute form.
Cytology
Prostate cancer is often diagnosed after a long, chronic illness, which the man tried to ignore. These diseases have very similar symptoms. Cytology studies help differentiate the oncological problem. With any form of prostatitis, protein is often present in the urine, and if the inflammation has developed into a malignant tumor, under a microscope, particles of the epithelium are clearly visible in the liquid. Therefore, preparation for an accurate diagnosis of prostate diseases includes not only a biopsy, but also a cytological examination to exclude oncological diseases.
Bacteriological method for diagnosing male disease
With the help of bacterial culture, it is possible to determine the catalyst for inflammation associated with an acute infectious disease. This role is usually played by fungi such as Candida and numerous microbes of pathogenic flora. The normal state of the urine of a healthy man is complete sterility. Infectious prostatitis is detected when bacteriological examination reveals traces of pathogenic microorganisms and fungal spores. In other cases, the current inflammation is determined to be acute or chronic.
A urine culture test will help identify infection with STI infection. To restore health, the doctor will select the most effective antibiotic for a specific situation. To clarify the diagnosis, the patient is examined using MRI, ultrasound, computed tomography and other instrumental methods. An experienced dermatovenerologist talks about reliable methods for diagnosing prostate diseases in the video:
How material is taken
There are 2 main methods for collecting urine for research - 3 and 4 glass samples. More often a 4-glass dose is prescribed, because it gives more informative results. Its difference from the 3-cup bottle is that liquid is also taken after the release of prostatic secretion. The material is collected as follows:
- The morning discharge is collected, the first drops need to be flushed down the toilet, the middle portion is divided into 2 containers, the remaining portion is also not suitable for analysis.
- Next, the prostate secretion is collected into the 3rd container.
- After this, you also need to urinate, already in the 4th container.
For the accuracy of the study, it is important that the first portion of urine is collected after a night’s sleep, so you should not urinate before conducting it. You should also abstain from sexual intercourse the day before. In addition, you should thoroughly wash and dry the penis and surrounding areas of the body. A few days before the test, you should stop taking uroseptics and antibiotics, which the urologist will warn you about.
Inflammatory prostatitis
Inflammatory prostatitis - type III A can be caused by the viruses Chlamydia trachomatis, Trichomans vaginalis, Mycoplasma hominis, Ureaplsama urealiticum, Candida albicans. The cause may also be chemical factors or autoimmune processes.
Similar to the bacterial form, it is necessary to examine the sexual partners of patients.
A PSA test should also be considered in patients at risk for prostate cancer.
PSA test
This form of inflammation is treated in the same way as the bacterial form. After determining the etiological factor, the inflammation is treated for six to twelve weeks. If necessary, treatment is extended with a maintenance dose up to several months.
Depending on the etiological factor, targeted drugs are used, for example, doxycycline, tetracycline, minocillin, erythromycin, and antifungal drugs. In addition, in the second stage of treatment, alpha-blockers, anti-inflammatory drugs and prostate massage are used for patients with urinary disorders. Transurethral thermotherapy and herbal medicine procedures can be performed. 5-alpha reductase inhibitors are also used.
Asymptomatic prostatitis
Asymptomatic prostatitis – type IV. The doctor recognizes this type of inflammation based on the results of a prostate biopsy, as well as examination of secretions and sperm. Patients do not report any symptoms, and a biopsy is performed when diagnosing, for example, prostatic hyperplasia or fertility problems.
Prostate biopsy
This form is treated by eliminating the hypothetical cause of the histopathological changes. However, visible inflammatory changes in prostate tissue are not an indication for antibiotic therapy.