In the practice of a doctor of any profile, one of the most frequently used diagnostic methods is clinical urine analysis, and pediatrics is no exception.
This is one of the most accessible and common screening tests in children of all age groups (from newborns to older children).
According to recommendations for the early detection of kidney pathology, in children in the first year of life, examinations should be performed frequently, which often poses certain difficulties for parents.
Introduction to Terminology
A general urinalysis is a routine screening laboratory test of a patient's midstream morning urine sample, which allows one to evaluate:
- 1Physical characteristics - color, smell, level of transparency, density.
- 2Acidity (pH).
- 3Chemical composition - determination of the content in urine of such components as glucose, urobilinogen, protein, ketone bodies, salts, bilirubin, etc. Normally, these substances are not detected in humans or are detected in such small quantities that they are called traces.
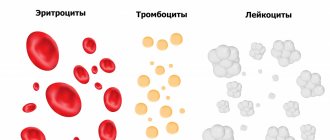
- 4The nature and composition of urinary sediment - microscopy of urinary sediment is performed to detect leukocytes, erythrocytes, crystals and bacteria. Thanks to this diagnostic stage, it is possible not only to determine the content of the listed elements, but also to calculate their exact quantity within the field of view of the laboratory technician, which is important in terms of further differential diagnosis.
The analysis is used for early detection of pathology of the urinary system, both congenital and acquired, in children of all age groups.
Main difficulties
The information content and reliability of the analysis largely depend on when and how the material for the study was collected. It is known that the qualitative composition of urine, as well as its density and chemical structure at different times of the day can fluctuate significantly.
To obtain the most reliable result, it is necessary not only to collect the material correctly, but also to deliver the material to the laboratory on time.
During the collection and transportation stages, parents, especially newborn children, may experience some difficulties, such as:
- 1Inability to accurately predict the time of the child’s next urination.
- 2Inability to explain to the child the need to urinate in the container or container provided to him.
- 3It is impossible to “plant” a newborn or infant over a specially prepared container.
- 4Low awareness of what containers the material can be collected in and how to do it correctly.
What not to do:
- There is no need to squeeze the described diaper into a container and submit such an analysis to the laboratory: the results will be unreliable, because various microorganisms and tissue fibers will get from the diaper into the contents of the container.
- There is no need to use homemade urine bags. For example, making them from a plastic bag is both inconvenient and unhygienic.
- You cannot freeze the container with the analysis (any kind). The material collected the day before is unsuitable for research.
- Enemas and laxative suppositories should not be used to stimulate bowel movements, otherwise the laboratory material will contain foreign impurities and the study will be unreliable.
When the baby grows up, the procedure for collecting tests will become much simpler. Both urine and feces can be collected from the potty. The main thing is that before collecting samples, the pot must be washed clean, but without using cleaning products. Just wash it with baby soap or baking soda and rinse thoroughly with water.
Preparation for collecting material
For analysis, it is preferable to use the “morning” portion, which collects in the bladder cavity during sleep. This reduces physiological daily fluctuations in urine values and allows for more reliable interpretation of the result.
Basic rules for preparing material:
- 1Urine is collected ONLY after preliminary toileting of the external genitourinary organs.
- 2The genital toilet is performed using clean (preferably running) water, from front to back, without the use of detergents. You should not use soap or local antiseptics for washing - this leads to a distortion of the result. In boys, it is necessary to retract the foreskin and rinse the base of the glans penis with running water (unless physiological phimosis prevents this).
- 3After the morning toilet, the baby must be wiped dry with a clean towel. Wiping is done by several successive soft blots. You should not rub the genital area.
- 4Urine collection is carried out only in a clean and DRY container. It is recommended to use special pharmacy disposable plastic containers for these purposes.
- 5 It is recommended to skip the first portion, however, in infants, due to physiological reasons (low volume of diuresis, inability to control urination, etc.), it is permissible to collect all available urine.
- 6For children of a later age who are capable of full-fledged dialogue, the first portion must be drained. The child should be instructed in advance.
- 7It is strictly PROHIBITED to pour urine into a prepared container from a baby potty, or to wring out nappies or nappies. With such manipulations, massive bacterial contamination of the biological material occurs and the result is distorted.
Preparing for blood tests
Recommendations for drawing blood from children under 14 years of age:
Psychological preparation of a child before donating blood:
- The main requirement for mom is to remain completely calm. Children, especially toddlers, feel their mother’s mood very keenly and also begin to get nervous if she is afraid of the upcoming procedure. With a child who has already reached preschool or school age, discuss what will happen. You should not scare him, especially if he is donating blood for the first time. You can also warn that the child will most likely experience discomfort.
- Make sure your child is not bored before the blood is drawn. Take with you a book, his favorite toy, a coloring book with markers - depending on the age of the child. This will not only take up his time, but will also not allow him to concentrate on the fear of the upcoming procedure.
- Decide whether you need to be present in the doctor's office during the test. Of course, it will be needed if the child is very small, but for some schoolchildren, even in the lower grades, the presence of parents can only interfere and provoke tears or protest. Focus on the child's psychological characteristics.
- During the blood collection procedure, small children should be held in your arms. If a child feels the warmth and protection of his mother, he reflexively calms down even in an unfamiliar and frightening environment.
- It is advisable to begin drawing blood not immediately after entering the treatment room. You need to give the baby a couple of minutes to get acquainted with the situation and the stranger who will take him by the hands.
- Preparation before donating blood:
- Remember that the best time to take a blood test is in the morning; the standards for all tests were developed specifically for the time interval of 8-11 am.
- Blood samples should be given strictly on an empty stomach. At least 8 hours must pass between the last meal and the blood draw. It is quite difficult to adhere to this rule with children, but it is quite possible. Drinking juices, tea, or eating cookies in the morning is prohibited, as this can significantly distort the results. You only need to drink water. Before going to the laboratory, take something tasty with you so that you can eat immediately after leaving the treatment room.
- The child's diet 1-2 days before the blood test should exclude fatty and fried foods and sweets.
- For better blood filling of the vessels, it is advisable to give the child 100-200 ml of water to drink 30 minutes before blood sampling (for children from 1 year).
- After the analysis, think about how you can please your child for good behavior. A small surprise gift will help smooth out the unpleasant impressions of the hospital.
- Features of preparing for blood donation for children from 1 day to 12 months:
- Try to take blood samples from infants between feedings, closer to the second feeding.
- 30 minutes before the procedure, the child should drink 50 ml of the liquid that you usually give him.
- At the time of drawing blood, the child’s hands must be warm. If you come from a cold street or the room is not that warm, you need to warm it up. This is a mandatory and very important condition, because the amount of blood that will be received by the health worker depends on its fulfillment.
- · Immediately before taking blood, the child should be positioned so that he is as comfortable as possible. A couple of minutes should pass before the nurse begins drawing blood. This time will be enough for the baby to calm down and get used to the environment a little.
Urine collection in young children
It is difficult for children to prepare material for research before they reach the age of two; it is difficult for parents to explain the rules to their child.
Therefore, there are several tricks:
- 1For infants, especially newborn girls, it is most convenient to collect material in special adhesive urine collection bags. To prevent the urine bag from being pulled off from above, you can wear thick panties, pants or diapers.
- 2 In children 1.5-2 years old who are accustomed to visiting the toilet, it is possible to use the so-called “grabbed” morning portion of urine, which is collected into a sterile container immediately after the start of urination.
- 3Before gluing the urine collection bag, the external genitourinary organs are toileted according to the same rules. The bag should be removed immediately after urination is complete.
- 4If no urination occurs within 30-60 minutes of gluing the bag, it should be replaced with a new one.
- 5Urine collected using adhesive bags is suitable for OAM using test strips, but should not be used for culture.
- 6 Urination in infants is often interrupted and occurs in small volumes. Therefore, it is possible to use several sterile urine bags in a row. To do this, immediately after finishing urination, the bag is immediately removed and the contents are poured into a sterile container. Then the baby should be washed a little with water, blotted with a clean towel and a new clean bag should be glued on. The process can be repeated until the required volume of material for research is collected.
Sputum analysis.
The analysis is collected in a sterile laboratory container. Before collecting sputum, you need to brush your teeth and rinse your mouth and throat.
II. ULTRASONOGRAPHY
Ultrasound examinations have several undeniable advantages:
- Suitable for all categories of patients, even newborns and pregnant women. Does not carry ionizing radiation (unlike X-rays).
- Can be used frequently. This may be relevant for assessing the effectiveness of treatment or monitoring the performance of manual operations.
- Ultrasound is not painful and does not require anesthesia.
- But the main advantage is its high information content. Ultrasound can detect injuries, age-related changes in bone structure, or incipient deformation.
The doctor sent the baby for an ultrasound. How to prepare him for this study? The answer depends on which organ the doctor has doubts about.
The ultrasound method is based on the property of ultrashort waves to pass through organs and tissues, reflecting from them differently. Then the doctor sees a general picture of the internal organs on the monitor.
Working positively
The most important preparation for an ultrasound is the child’s positive attitude. Agree, performing a procedure on a sobbing baby is not the most pleasant task, and the results in this case are unlikely to be correct.
Has your baby never had an ultrasound before? This means he doesn’t know what it is and how we all fear the unknown. Parental calm and the necessary information can relieve fear and set the child up for positivity. Even a three-year-old toddler is able to understand your explanations about what awaits him at the doctor.
For example, tell them that during the examination the doctor will use a special and maybe cold gel, which he will spread on the skin; he may ask the little one to turn from side to side, hold his breath for a while or inflate his tummy. The child just needs to know about this, be prepared and accept it in a friendly manner.
Don’t say “it won’t be scary”; such phrases have the opposite effect. When we are told that it will not be scary, painful or bad, the brain does not perceive the particle “not” and therefore automatically tunes in to the negative.
Just tell them how everything will be and assure you that you will definitely be there. The procedure itself will not take more than 15-20 minutes if the preparation is carried out effectively.
Stimulation of the urination process
Although the process of collecting material for analysis today is somewhat simplified by the presence of special children's containers and containers, often the main problem of parents is the inability to predict the time of the child's next urination.
To solve this problem, it is possible to use reflex stimulation of the process of emptying the bladder:
- 1The process of urination in infants is reflexively associated with eating and drinking, so they can be breastfed or bottle-fed.
- 2 Urination in an infant can also be induced by gentle pressure and stroking in the suprapubic area.
- 3Collecting urine from an infant and a one-year-old baby is sometimes easier to do in the bathroom, “planting” him over the container, that is, giving the baby a semi-sitting position in the arms of one of the parents.
- 4Additionally, to stimulate the process of urination, it is possible to use the sound of pouring water, which also reflexively leads to emptying the bladder.
How much urine is needed for analysis?
The answer to this seemingly simple question directly depends on the level of equipment of the laboratory to which the material is submitted.
When performing the analysis “with the hands” of a laboratory assistant, the minimum permissible amount of urine is 50 ml. If the laboratory has analyzers - special devices aimed at speeding up and automating sample processing, the minimum volume is much smaller and is about 20 ml.
The same volume will be sufficient when performing express analysis using express test systems (test strips).
Figure 1 — Automatic urine analyzer
As can be understood from the above, it is advisable to know the capabilities of the laboratory where the material for research will be delivered.
Almost all modern laboratories use automatic analyzers, however, if there are deviations in the results obtained automatically, urinary sediment elements are always recalculated manually. This eliminates technical failures and minimizes the number of false results.
Thus, to perform a urine test on an infant, it is better to fill a container of 50-70 ml.
What containers are best to use?
It is best to place the material in a ready-made sterile pharmacy container. You should not purchase non-sterile containers from the pharmacy; they may be contaminated.
See the picture below for what ready-made sterile containers for collecting urine look like. Please note that such containers always have a sterilization date and expiration date indicated on the packaging. Containers without packaging cannot be sterile and, therefore, require pre-treatment.
Figure 2 - Sterile container
For OAM, it is permissible to use reusable, cleanly washed, sterilized with boiling water and dried containers (for example, glass jars). Such containers are still used in some hospitals and clinics.
However, if you are submitting material for bacteriological research, the use of such containers should be avoided, as the result will be distorted. Urine for bacterial culture is collected only in sterile containers.
In infants, disposable sterile urine bags are often used (Figure 3).
Figure 3 - Disposable, universal, sterile container bag
These urine bags have an outer sticky edge that can be used to attach the device to the baby's skin. The hole in the urine bag can be universal, or it can be adapted for boys or girls (Figure 4).
Figure 4 - Sterile urinals for infants (oval hole - universal; ovoid hole - for boys; hole of complex shape - for girls)
How to properly collect urine from a child
It is permissible to collect the analysis only in a sterile container (sold in pharmacies and costs 12-20 rubles). Do not use mayonnaise jars for this - containers that are poorly rinsed from food and soap will distort the final result.
Do not collect material for analysis in the evening: urine should be delivered to the laboratory no later than 2 hours from the moment the container is filled.
If the material is left for a longer period of time, the analysis may be unreliable due to sedimentation.
Ideally, more than 5 hours should have passed since the last urination. However, for a baby who may urinate more than 15 times per day, it is impossible to fulfill this requirement. Therefore, try to collect urine immediately after your baby wakes up.
Features and preparation:
- Transport urine carefully - frost or heat can distort the results. If you are not sure about the weather, use a thermal bag.
- The day before, do not give your child unfamiliar foods (and do not eat them yourself if the child is breastfed), and do not feed vegetables and fruits that can color the urine.
- Try to keep your baby from overheating, sweating and freezing before donating urine - all this can negatively affect the final result.
- Try to make sure that the child does not cry - the emotional state also affects the performance.
Important: you must give urine on an empty stomach. You should collect an average portion of the very first morning urination!
Transportation rules
The reliability of the OAM result is influenced not only by the correct collection of the test material, but also by its correct transportation. Basic rules for delivering material to the laboratory:
- 1Transportation should be carried out only at positive air temperatures, otherwise salts may precipitate, which may be mistakenly taken for pathology.
- 2Collected urine is stored for no more than two hours. Prolonged storage of urine at room temperature leads to excessive bacterial growth, destruction of urinary sediment elements and changes in pH. If you need to store more than 2 hours, you can use the refrigerator, but do not forget that freezing urine and excessive cooling are undesirable.
- 3The sample must be delivered to the laboratory closed, with the cap tightly screwed on.
- 4The container must be marked according to the direction. It is necessary to indicate on it the patient’s full name, date and time, as well as data from the referral: office or site number, type of study (OAM), date of birth of the patient. Following this simple rule will help you avoid losing your container. The guide can be attached to the container using a thin rubber band, but this is not necessary.
- 5 During transportation, you must avoid not only freezing, but also heating, shaking and accidental opening of the lid, this will lead to contamination of the material and distortion of the result.
The OAM result is usually ready on the day of delivery in a few hours. In a clinic setting, the result form may be delayed in the laboratory for 1-2 days (the influence of the human factor). In paid laboratories, the period for performing OAM can sometimes be extended; in this case, a special preservative is added to the research material.
How to decipher the results?
Normal values of TAM indicators in children differ somewhat from those in adults, which is associated with the functional immaturity of the urinary system.
Intrauterine development of the kidneys ends around the third month of gestation. The number of structural renal elements (nephrons) in a newborn is equal to that of an adult (about 1 million), but their structure and morphology are different.
Children have a smaller renal nephron, less permeability of the renal filter, short proximal tubules, this affects the processes of filtration and concentration of urine.
Gradually, as the baby grows, the renal tubules mature, which is why the norms for OAM indicators in children depend on their age.
The table below shows the norms that are used to decipher the result. Next, we will consider the most common deviations in results and their causes.
Table 1 - Standards for deciphering the results of OAM in infants and children after one year
10. “Dirty” analysis
Contamination of collected urine occurs in the following cases:
- 1Poor toileting of the external genitalia before collecting biological material for research.
- 2No drying of the skin.
- 3Pour urine from a child's potty.
- 4Use of reusable containers, plastic containers, insufficiently processed glass containers, wet containers, etc.
- 5 Use of simple plastic bags in infants instead of special urinals.
- 6Overheating of the container before delivery to the laboratory, long-term storage in the light.
- 7 Failure to comply with the terms of application of disposable urine bags (wearing more than 40-60 minutes).
The features of this analysis are:
- 1A large number of squamous epithelial cells in the field of view, sometimes the number of epithelial cells is so large that they cannot be counted by a laboratory assistant. In such cases, they are designated on the study form as “epithelial layers.”
- 2The number of leukocytes, as a rule, is not changed or increased slightly, because there is no process of inflammation.
- 3An increase in protein may be detected in the sample, but the deviation is often minor.
- 4The level of bacteriuria can range from moderate (++) to significant (++++).
- 5 The sample may contain a small to moderate amount of mucus.
- 6Levels of red blood cells, glucose, urobilinogen and ketone bodies are within normal limits.
- 7An increase in density may be observed.
- 8The color of the sample is not changed, but it often becomes cloudy and has an unpleasant odor.
Figure 6 — Contaminated OAM sample
Hygiene before urine test collection
Remember that cleanliness of the external genitalia is the key to an accurate urine test result.
Bacteria that accumulate on the skin with the material end up in the container, causing the laboratory technician to write an unreliable result.
However, a large number of bacteria in the urine, while other indicators are normal, almost always indicates poor hygiene before the test, and the doctor requires a urine retake.
How to wash a child?
Both girls and boys should be washed from front to back.
to prevent bacteria from the external opening of the rectum from reaching the external genitalia:
- We wash with warm water and a small amount of baby soap, which we then rinse well.
- We do not use herbal decoctions - they can cause allergic reactions.
How to collect urine from a newborn?
Usually there are no problems with an older child:
- If the child already understands that he needs to go to the toilet, we simply ask him to do it. It is advisable to carry out the procedure in a bathtub so that an average portion of urine can be collected in a container.
- We put the baby in the bath and turn on the water. The baby will react to the pouring liquid by urinating.
- You can give water during the process so that the child urinates faster.
- If possible, turn on the sounds of running water on your computer or phone.
- You can provoke urination by placing the child’s palm in a bowl of warm water.
How to collect urine from a small child?
You can buy special urine bags at the pharmacy - they are glued to the skin around the external genitalia, and urine is collected in a sterile container:
- If you don’t have a urinal, you can patiently wait with a jar in your hands for the next urination, but this method only works with babies 1-2 months old: more active children will not lie still!
- Another option is a thick, sterile disposable bag, but this method is only suitable for boys.
- For girls, the option for collecting urine is a shallow plate or saucer, but if possible, you should still use a sterile disposable urine bag.
How much urine is needed for analysis?
The minimum amount of material is 50 ml.
For newborns, at least 20 ml is usually sufficient.
A smaller amount of urine will not allow you to determine all the parameters that a general urine test usually requires.
Urinary tract infection
The most common urinary infections in children are cystitis and pyelonephritis. These diseases are infectious-mediated, which means they are accompanied by the presence of not only abnormalities in the TAM, but also the development of clinical symptoms of inflammation.
In early childhood, the symptoms of inflammatory diseases are usually nonspecific, and collecting complaints is difficult, which presents certain difficulties for the attending physician and parents.
That is why OAM is the main screening method to confirm or refute the presence of inflammation in the urinary system.
Differences that allow one to suspect an infectious-inflammatory process in the urinary system in a child are:
- 1Leukocyturia (increased number of leukocytes in the field of view). Abnormalities in the number of white blood cells in the urine directly correlate with the severity of the infection.
- 2Moderate proteinuria (moderate increase in the amount of protein in the urine, not exceeding 2 g/day). The more severe the infectious process, the greater the amount of protein is detected, but no significant deviations in this indicator occur, since the renal filter remains intact.
- 3Microhematuria (slight increase in the level of red blood cells) may be observed. Red blood cells are mostly unchanged. They enter the urine directly in the ureters or bladder.
- 4 In OAM, a large amount of mucus can be detected (more often with urethritis and cystitis). The severity of mucus contamination is indicated on the form using the “+” sign. The more “+” there is in the “mucus” column, the greater its amount in the sample. The maximum value is "++++".
- 5The acidity of urine can shift towards the alkaline side, which is due to the vital processes of pathogenic microorganisms.
- 6Bacteria are always present in the baby’s urine; bacteriuria can vary from “+” to “++++” depending on the severity of the infection.
- 7In case of urinary tract infection, it is possible to detect nitrites, phosphates, and less often other salts (metabolic products of uropathogenic flora).
Figure 7 - Form for urinary tract infection. Leukocyturia, moderate proteinuria, bacteriuria, oxalates are observed
If abnormalities are detected that indicate the presence of an infection in the urinary system, the baby needs to be further examined:
- 1Nechiporenko test - to assess the number of leukocytes and erythrocytes in 1 milliliter of urine.
- 2 Urine culture - to determine the degree of contamination and detect a specific uropathogen.
- 3 Ultrasound of the kidneys and urinary tract - to exclude organic pathology of the kidneys, structural anomalies and stones.
Errors
What not to do when collecting urine:
- You cannot take urine for analysis from a potty, from an oilcloth, and even more so from squeezing it out of a diaper. The results of such analyzes will be distorted.
- You cannot take urine for analysis from the second, third and subsequent “trips to the toilet”.
- Do not keep urine in the refrigerator for a long time or freeze it.
- Use a dirty container for urine or fail to wash the baby.
- Donate urine after the child’s intense stress - physical or emotional.
- It is also not worth giving urine immediately after vaccination.
Why do you need a general urine test?
- This study is prescribed to children during medical examination.
Usually it is carried out in the maternity hospital, then at 1, 3, 6, 12 months, 2 years. Further - according to indications. - Examinations before admission to kindergarten and school.
- OAM must be taken after treatment of various diseases, for example, ARVI. It will display the functioning of the kidneys, digestive system and other organs. It is important to know how the infection has affected the body, as well as the medications prescribed
(especially antibiotics). - A urine test shows how the kidneys and the urinary system in general are working.
- It is important to donate urine after a child has had bacterial infections,
which often impair kidney function. - OAM is prescribed before vaccination to make sure that the baby is healthy.
- For the diagnosis of diabetes mellitus
as a screening.
Example of a urine test form:
Glomerulonephritis and nephropathy
Glomerulonephritis and nephropathies of various origins are diseases characterized by damage to the glomerular apparatus of the kidneys without involving other parts of the urinary system.
Most often, the pathology is based on autoimmune damage to the glomeruli due to the deposition of damaging immune complexes on their membranes.
At the initial stages, the disease occurs with minimal clinical manifestations, which increases the informativeness of TAM for confirming the diagnosis. Early detection of glomerulonephritis and autoimmune nephropathies can prevent the development of severe renal failure.
Suspicion of the presence of damage to the glomerular filter arises from the following deviations in the TAM:
- 1The main role is played by an increase in protein levels in the urine (proteinuria). The severity of proteinuria can range from moderate to significant, which is associated with a violation of the filtration process of blood plasma proteins.
- 2Hematuria (increased number of red blood cells in the urine) is no less significant. Red blood cells are mostly changed. The severity of hematuria varies from microhematuria (invisible to the eye) to macrohematuria (pink and red coloration of the sample).
- 3The content of leukocytes and epithelium is most often within normal limits.
- 4With long-term damage to the renal glomeruli, a decrease in urine density is observed, which is due to a violation of concentration processes.
Figure 8 — OAM in a child with chronic glomerulonephritis
With long-term nephropathies, a child may develop the so-called nephritic syndrome, when massive proteinuria is accompanied by edema, a decrease in blood plasma protein levels, and an increase in vascular pressure.
Swelling occurs in the face (eyes) and ankles, then spreads and becomes denser. Generalized edema and anasarca are observed in severe cases of the disease.
A child with suspected glomerulonephritis/nephropathy undergoes further examination, including:
- 1Urine analysis for daily proteinuria - to assess the degree of daily protein loss.
- 2 Nechiporenko test - for quantitative counting of red blood cells and leukocytes in 1 milliliter of urine.
- 3Zimnitsky test - to determine the concentration ability of the kidneys.
- 4Determination of glomerular filtration rate.
- 5Ultrasound of the kidneys - to exclude organic pathology of the renal tissue.
- 6Biochemical blood test (BAC), with mandatory determination of the level of total protein, albumin, urea and creatinine.
- 7Determination of the level of pathological immunoglobulins, circulating immune complexes, antistreptococcal antibodies.
- 8The most accurate result is achieved with a puncture biopsy of the kidneys. Although this study is not always available, it allows us to most accurately determine the type of glomerulonephritis and select adequate treatment for the disease.