Installing an eye prosthesis is the only way for patients who have lost one eye to return to normal life. The degree of effectiveness of prosthetics depends on the correct selection of the product - the higher the degree of its correspondence to the human natural eye, the better the rehabilitation will be. Medical products can be standard or individual; special attention in clinical practice is paid to their safety. High-quality dentures must come with certificates of conformity, which you can request from the seller at the time of purchase.
When is prosthetics necessary?
Eye prostheses solve not only the patient’s aesthetic and psychological problems. If a person who has lost an eye does not wear a substitute, over time the conjunctival cavity will become smaller, and the eyelashes will begin to curl inward, causing a lot of inconvenience and becoming the main cause of the development of chronic inflammatory processes.
Eye prosthetics solves important aesthetic, physiological and psychological problems.
Prosthetics play a particularly important role in children - the presence of an eye substitute in the conjunctival cavity stimulates the growth processes of the orbital bones. If prosthetics are not performed, bones grow slowly and facial asymmetry develops. When necessary, before prosthetics, doctors perform eyelid surgery, correction of the conjunctival cavity, create a musculoskeletal stump, perform enucleation, evisceration, or evisceroenucleation with implantation.
As a rule, prosthetics are prescribed in case of partial or complete removal of the eyeball due to the following diseases:
- Extensive eye injury followed by its removal.
- Congenital anomalies, as a result of which atrophy of the visual organ developed, followed by necrosis.
- Atrophy of the optic nerve in combination with infectious neuritis, which gave a complication in the form of infection of all tissues of the eye.
- Cancerous tumors.
Partial prosthetics is the replacement of the lens for cataracts, the vitreous body for extensive hemophthalmos, aphakia is the complete absence of the lens, severe coloboma, affecting the quality of visual acuity.
Implants in the brain and eyes
The Biomolecule has already described the Argus bionic system, which transmits signals from the camera to an implant in the retina and then to the brain [10]. To obtain such “bionic vision”, the patient must pay $150,000. However, the resulting vision does not become normal in our understanding - these are flashes of light and sparks, sometimes silhouettes of people and objects. The first bionic eye, Argus II (Fig. 4), was implanted into a patient in 2009 by doctors at the University of Manchester. Now, 10 years later, the creators of Argus II are testing a more effective artificial vision system, Orion, which is implanted directly into the patient's brain.
Figure 4. Bionic vision: Argus II system diagram
Anthony Buchbinder
Like the Argus II before it, the Orion system consists of a small camera mounted on glasses to capture images, a unit that converts video into electrical impulses that the user can interpret, and an implant that stimulates the user's brain. However, unlike the Argus II, which used implants clamped onto the patient's optic nerves, the Orion implant is located directly in the brain. The main disadvantage of the new product compared to its predecessor is the need to remove a small part of the skull in order to expose the area of the brain where the electrode array is located, and these represent additional clinical risks.
The developers plan to improve the accuracy of the image by adding more electrodes, and also experiment with thermal imagers - they will allow the blind to see the hot stove and people in the room. One way or another, the technology requires improvement and FDA approval, but the cost of treatment is unlikely to change downward.
These systems have analogues: Boston Retinal Implant and IRIS, which work on a similar principle. Only Retina Implant AG differs significantly from its competitors - this system does not have an external camera, but captures photons and activates the optic nerve.
Kinds
Taking into account the production technology used, eye structures are divided into individual and standard. All products are made manually in specialized laboratories - attempts were made to automate their production processes, but did not give the desired result.
All prosthetic products are made strictly by hand.
Standard products are universal, and the characteristics of the eye cavity of a particular patient are not taken into account. Individual ones are made to order, taking into account the structural features of the conjunctival cavity of a particular patient, the color, relief characteristics of the sclera and iris of the healthy eye.
The sizes of dentures are:
- small;
- large;
- average;
- micro.
On the wearing side:
- left;
- rights.
By form:
- ball;
- ellipse;
- etc.
When classifying products, such characteristics as the fit of the iris, the colors of the sclera and iris, and the material of manufacture are also taken into account. Plastic ones are in greater demand today than glass ones because they are more durable, safer, and do not break. Also distinguished are thin-walled products used during the formation of the eye cavity and for cosmetic camouflage of eye defects with cataracts, thick-walled, double-walled - they are used in the complete absence of their own eyeball.
Prostheses for children and adults are not divided into categories - the selection of products is carried out by size.
The bionic eye and the great mystery of vision
Author:
Reznik Irina
7 minutes
In Russia, for the first time, an operation to implant a bionic retina was carried out, and soon a person who lost his sight 25 years ago will be able to see the world again. Although not in the same way as healthy people. Heading the surgical team, the director of the Research Center of Ophthalmology of the Federal State Budgetary Educational Institution of Higher Education Russian National Research Medical University named after N.I. Pirogov, created on the basis of the Federal Scientific Research Center of Otorhinolaryngology FMBA, Professor Hristo Takhchidi told Mednovosti how the bionic eye works, when it will become available to thousands of other patients, the importance of this experiment for science, and what is needed for the success of any scientific and clinical project.
{#vrez.59796}
Hristo Periklovich, a week has passed since the operation, can we already draw any conclusions?
— It’s still early. Now all electronics are turned off, the classic postoperative period is underway: wounds close and scar, tissues adapt, eye tone, circulation of intraocular fluid improve. And we monitor these processes, calm the eye, bringing it back to normal, and wait for the end of the biological response to implantation of foreign materials. All these materials are non-biological (that is, we are not talking about an immunological reaction to a foreign protein), they are almost completely inert and are accepted by the human body.
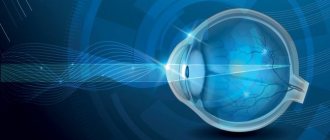
What exactly is a bionic eye?
— This is an electronic system designed to perform the function of the eye. It allows you to establish a connection with the brain through electronics and thus recreate the natural chain disrupted by retinal disease. The outer part of the structure is glasses with an antenna and a micro-camera, which captures the image and transmits it to the converter, which is attached to the side of the person’s belt. Here the image is transformed into electrical microimpulses, which then enter the retina and stimulate its remaining functional neurons, after which the image enters the brain.
The internal part - the bionic eye itself - also consists of several elements. One of them, an electronic chip with 60 electrodes, is implanted inside the eye, and the others are attached to the eyeball on its surface. But we also immersed them a little deeper so that they would not interfere and would not be visible. This was our first time working with electronics; we had to check them at every stage of the operation, during which the implant could be damaged. The electronics will start up two weeks after the operation, sometime after July 19. By this time, the eye tissues should have recovered naturally. And then we will look to see whether the retina responds to an electrical stimulus and whether there is a connection with the brain.
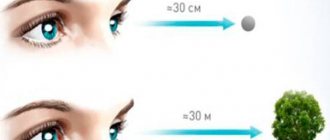
What will your patient see?
“These systems make it possible to see an abstract black and white image in the form of certain configurations of light figures. It resembles a pixel picture, albeit with a very low resolution. But this gives a person social rehabilitation; it will be much easier for him to navigate space. Having undergone training in a special program, he will know what the light figures coming to his retina and then into the brain mean - a door, a window or a plate. Over time, the device will, of course, improve and provide a picture closer to that conveyed by natural vision.
Can such a design help any blind person? What are the general criteria by which patients are selected?
— The criteria are quite specific. First, the patient must have retinitis pigmentosa (retinal degeneration). This is a classic disease that affects the periphery of the retina, gradually narrowing the field of vision until, ultimately, this window closes completely. This is a disease with a certain hereditary component, which develops according to its own biological scenario, which, unfortunately, is not yet under our control, although the gene responsible for its development has already been found. The process goes on for decades, affecting mainly boys who go blind at the age of 30-35.
But, although a person lacks objective vision, this is not absolute blindness, when there is no sensation of light at all. And this facet is the second condition for implantation; a person must retain light perception with an incorrect projection. That is, he does not see where the light comes from, but the concepts of light and darkness exist for him. In addition, there are requirements for general health, and chronic diseases of the same eye are taken into account.
Our patient is 59 years old and has not seen for more than 25 years. He is from Chelyabinsk, in his youth he managed to get a profession, he worked as a milling machine operator. Today, he also has seriously reduced hearing (until now there have been no hearing-impaired patients among those who have had a bionic eye implanted), and a hearing aid helps him communicate. He is an optimist, determined to succeed, and this helps a lot in our common cause.
{#vrez.59797}
What requirements must a clinic that can perform implantation meet?
- There are a lot of them. The clinic must have the most modern equipment and highly qualified specialists who own the most advanced technologies, only then is the issue of participation in the program even considered. Annual testing is carried out to evaluate equipment, equipment, and consumables. Specialists are trained and tested, and after some time some are given the go-ahead. Our Center, created in 2020 on the basis of the Federal Scientific and Clinical Center of Otorhinolaryngology of the Federal Medical and Biological Agency of Russia, passed this selection.
It is also needed because now we are at the very beginning of work in this direction. The project is undergoing clinical testing. The small world experience includes about 300 similar operations carried out over the ten years of the technology’s existence. And if we talk about this more advanced model - the Argus-II bionic implant - then only a few dozen operations. Therefore, you should completely eliminate the human factor and be sure that only the system itself is tested - how it works, what is positive or negative about it, what should be improved, what the next modification should be.
Who owns the authorship of the methodology?
— The engineering part is the job of the system developer. This is an American company, one of the major manufacturers of cochlear hearing implants. Conceptually, the idea is the same - cochlear implants are similar in design to this system. Electrodes are inserted into the inner ear to contact the auditory nerve, which is stimulated by microelectric impulses coming from the transducer. When experience with cochlear implants showed their effectiveness, the company had the idea to do something similar in ophthalmology. But, of course, working with the retina is several orders of magnitude more difficult than working with the auditory nerve - these are completely different systems.
As for surgery, ophthalmological technology was developed by our foreign colleagues, who became pioneers in this matter. We are now involved in this scientific and clinical process, using this technology, we are noting some nuances that can be changed and, in our opinion, made better. Human thought is always looking for an answer to the question: how to achieve maximum efficiency, and to do this technically more simply. Now we have assembled this structure, and it has already become clear that if it is made half as large, it will be easier to implant and it will be more convenient to manipulate it.
If we look at this story from a scientific point of view, then a small step has been taken towards understanding how our visual system functions. Today we know a little more about the eye, less about the retina, and even less about the optic nerve and the pathways of the cortical analyzer. There are, of course, certain hypotheses, but how this actually happens remains to be deciphered. The connection between the brain of a patient implanted with a bionic retina and the image will occur through an electronic system that is created by a person who understands how it works. And, thanks to this, a code element appears for deciphering the great secret of nature called vision.
Have you already started preparing for the next such operation? Is it even planned?
— Yes, it is planned for the fall.
And such operations can be put on stream? How many Russians in general need bionic retina implantation?
— The incidence of this pathology is approximately one person in 4-5 thousand. That is, about 40-50 thousand for the whole of Russia. And this means that in the coming years several thousand people will need such an operation. The Argus II system itself costs about 10 million rubles, and several charitable foundations have now taken upon themselves to pay for it. (“Connection”, “Art, Science and Sports”). But in principle, everything is possible if you set such a task. At one time, the task was set to introduce microsurgical technologies and provide the population with implantation of an artificial lens.
And at first this also seemed like a fantasy.
— In March 1986, a government program of the MNTK “Eye Microsurgery” was created, headed by Academician Svyatoslav Nikolaevich Fedorov. I've been in this project from day one. And one of the godfathers of this program was Prime Minister Nikolai Ivanovich Ryzhkov, thanks to his assistance, within three years we built 12 centers throughout the country. The construction of each clinic cost 9-10 million rubles, and about 1.5 million more rubles went for equipment - that’s the price of the issue. For the Soviet Union it was generally pennies. They are now functioning safely and meeting the needs of the entire country and, moreover, they have also trained other doctors in this technology. And already in 2010, the Ministry of Health reported that more than 95% of operations in the country are performed using microsurgical methods. That is, the task that the Union government once set for us was fully completed.
That is, in 20-25 years the problem was solved on a national scale.
— Yes, and it was decided in such a way that we reached the highest level in world ophthalmology. Patients from developed countries began to come to us. When I was the general director of MNTK MG, we operated on up to five thousand foreigners - Germans, Italians, residents of rich Gulf countries. And in 2009, we celebrated our five millionth operation. The system screened a million patients annually. And this was not the limit; in individual branches where relations with regional health authorities were worked out, sending patients here in a timely manner, the figures were twice as high.
What was needed for this? People. First of all, a leader who is able to gather around himself the same enthusiasts, young charged guys, a little money and a lot of desire. And the main thing was not to interfere with the development of the project. We were able to understand all the pros and cons of existing technologies in the world, improve them and thereby bring domestic ophthalmology to the world level.
So, I have a wealth of practical experience in introducing technologies into Soviet and Russian ophthalmology that simply did not exist before, as well as experience in constantly improving the implemented techniques. And this became another serious competitive advantage that influenced the choice of our clinic at the Scientific Research Center of Ophthalmology, Russian National Research Medical University, to carry out the first implantation of a bionic eye.
Caring for your prosthesis
Before performing operations to insert and remove an eye prosthesis, wash your hands thoroughly and prepare eye drops, wipes, and a suction cup. Be sure to sit at a table covered with a soft cloth and place a mirror in front of you.
Removing the prosthesis
The procedure for removing the prosthesis is as follows:
- lift the upper eyelid;
- moisten the suction cup;
- Apply the compressed suction cup and press it to the simulated pupil;
- release the suction cup;
- run a little air under the prosthesis along the upper edge;
- slowly pull the suction cup forward;
- remove the prosthesis downwards.
Removing the eye prosthesis
How to install
How to insert a prosthesis yourself? Proceed as follows:
- Wash the product and carefully insert it under the upper eyelid (it is best to do this while the prosthesis is still wet).
- Look up and gently pull down your lower eyelid.
- Finish inserting the product by slightly turning it to the temporal side.
- Press down on the prosthesis and move it a little - this is necessary to release the air.
Installation of an eye prosthesis
How to clean
The prosthetic eye is washed in warm water and soap - alcohol should not be used. The postoperative product may not be removed. Be sure to strictly observe the rules of personal hygiene, keep your eyes closed while washing.
If the prosthesis remains in the eye cavity for a long time, it begins to irritate the conjunctiva.
How often is cleaning required?
Standard cleaning is done once every two weeks. Check with your doctor for details.
Cleaning the prosthetic eye
Installation of an artificial eye
Eyeball implantation is performed in ophthalmology clinics equipped with specialized equipment. Surgical interventions include microsurgical removal of the affected structures of the native organ of vision and transplantation of biological or artificial implants. The operations are performed under local or general anesthesia. They include several steps that must be performed consistently and scrupulously to avoid complications. In the postoperative period, the patient is given immunosuppressive therapy to reduce the rejection reaction. The rehabilitation period takes from several months to a year.
Conditions for replacement and storage
Adult patients wear the prosthesis for 8-10 months and then replace it with a new one. This must be done, since the surface of the product becomes rough as a result of constant wear, grooves and small cavities appear on it, injuring the mucous membrane of the eye.
Necessary attributes for storing a prosthesis
Planned replacement of plastic products is carried out once every two years, glass products annually.
You need to wear a prosthesis constantly. If you take it off at night, do not put it in water or a disinfectant solution - wash it with warm water and soap, and place it on a cloth.
Types of operations
They are isolated based on the parts of the eyeball that are transplanted. Therefore, there is such a classification of transplantations:
Both donor and artificial corneas are used for replacement.
- Corneal transplant. This operation is simple because superficial structures are transplanted without penetrating into the deeper layers of the organ.
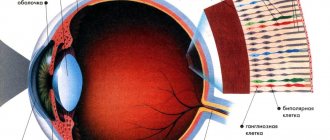
- Retinal implantation. This is a more complex surgical option. Nerve cells - rods and cones - are capable of destruction at the slightest mechanical or chemical impact.
- Lens replacement. This natural lens has no antigenic factors to which the human immune system would react. Therefore, the new lens takes root well.
- Bioprosthesis transplantation. The latter is an artificial eye, which is a cluster of electrodes implanted into the fundus of the eye instead of the retina. Signal converters go from them to special glasses.
- Transplantation of the simulator. It refers to an artificial eyeball that does not perform visual functions, but only replaces a removed organ for aesthetic purposes.
- Iris replacement. It is performed for aniridia - complete damage or absence of the iris.
conclusions
Ocular prosthetics allows a patient who has lost an eye to return to normal life. Both in adulthood and in childhood, wearing prostheses is mandatory. Scheduled replacement is carried out 1-2 times a year (glass products need to be changed more often).
Ophthalmological surgeons resort to prosthetics only in advanced cases when no other corrective practice is capable of restoring the eyeball. Until then, various ophthalmological techniques can be used to preserve the eye, even taking into account the loss of its main function.
From the history of the use of the bionic eye
Linda Morfoot from California suffered from retinitis pigmentosa at the age of 21. After 29 years, the woman was almost blind, only her left eye reacted slightly to light. It was 2004. Doctors suggested that Linda test a bionic eye with a mother of 16 electrodes. After installing the sensor, Linda began to distinguish the outlines of objects. She recognized buildings, structures, urban infrastructure, people and city lighting.
Later, the bionic eye was implanted after vision loss in patients aged 50+. Peter Lane had controllers implanted in his eye that transmit signals from special glasses to his brain. Lane and 32 other volunteers lost their sight as a result of retinal dystrophy in their youth. Lane began to distinguish the outlines of objects in the room and recognize graphic symbols. Lane was 51 years old at the time of the operation. Other operations also turned out to be successful.
For 10 years, researchers have been optimistic about the bionic eye. It was assumed that by 2009 a bionic eye with a matrix of 2.5 thousand pixels would sell for 15,000 pounds, but the forecast did not come true.
Indications and contraindications for prosthetics
So, an “artificial eye” is usually installed on a person for the following reasons:
- subatrophy of the eyeball or its atrophy after illness or injury;
- anophthalmos after enucleation or evisceration of the eyeball;
- microphthalmos, anophthalmos (anomalies in the development of the eyeball).
There are also contraindications to its installation:
- It is prohibited to install an eye implant less than 6 months after injury;
- uveitis;
- high intraocular pressure;
- foreign body in the eye;
- symblepharon;
- swelling in the eye;
- keratoconus;
- dystrophic keratitis.
In any case, you should consult an ophthalmologist before surgery.