Detailed description of the study
The study aims to diagnose respiratory tract tuberculosis, a disease that is the most common cause of infectious death worldwide. Highly accurate methods such as PCR make it possible to diagnose the disease before symptoms appear. In this study, urine is used as a biomaterial: it is easy to collect, and the risk of infection of laboratory workers is much lower than when testing blood or sputum.
According to WHO, 10 million people fell ill with tuberculosis in 2021, and 1.6 million of them died from the disease.
Russia is one of the countries where tuberculosis is most common. To reduce this indicator, measures are being taken for prevention and timely diagnosis: this has reduced the number of patients and carriers.
The main difficulty of diagnosis is that a person infected with tuberculosis may not be aware of his illness for a long time while his immune system restrains the pathogen - the bacterium Mycobacterium tuberculosis. It is a very insidious microorganism, with many mechanisms for defense against the immune system and long-term latent survival in the body and in the environment.
In fact, about a third of the world's population is infected with Mycobacterium tuberculosis, but only a few of them develop clinical disease. As a rule, these are those people whose immunity is insufficiently developed or weakened: children, elderly people, immunocompromised persons (HIV-infected). Or those who are in conditions of insufficient sanitation and large crowds of people in confined spaces (for example, in prisons).
Tuberculosis usually affects the lungs, but can affect other organs and even bones. The source of infection is a patient with open tuberculosis, who releases mycobacteria into the external space. There are also people with a closed form - who are sick, but not dangerous to others. The infection is transmitted by airborne droplets or from a pregnant woman to the fetus in the womb, since Mycobacterium tuberculosis can enter directly into the bloodstream.
Symptoms of the disease are:
- Weight loss/ anorexia
- Loss of appetite
- Profuse sweating at night.
- Heat
- General weakness
If we are talking about the pulmonary form of the disease, symptoms may include:
- Cough
- Hemoptysis (coughing up blood)
- Chest pain
Polymerase chain reaction (PCR) is a research method that allows you to detect pathogen DNA in biomaterial even in small quantities. The specificity of PCR reaches 100%. This method makes it possible to detect the genetic material of mycobacteria even in urine. When mycobacteria are neutralized and destroyed by cells of the immune system, fragments of their hereditary material enter the blood. They are very small, so they pass through the kidney filter and are found in the urine. Urine is the easiest biomaterial to collect and poses the least risk of infection for laboratory staff.
How?
It is advisable to collect sputum in the morning (since it accumulates at night) before meals in a sterile container, which is provided in the laboratory. 3-5 ml of sputum is sufficient for examination. Sputum analysis must be performed no later than 2 hours after collection. The closed container of sputum must be stored in the refrigerator until it is sent to the laboratory.
To detect Mycobacterium tuberculosis with a 50% probability during microscopy, 1 ml of sputum must contain more than 5000 microbial cells. The sputum of patients with pulmonary forms of tuberculosis usually contains a significant amount of acid-fast bacteria, which allows them to be confidently detected by bacterioscopy.
References
- All-Russian public organization "RUSSIAN SOCIETY OF PHTHISIATRICS": Federal clinical recommendations for organizing and conducting microbiological and molecular genetic diagnostics of tuberculosis - Moscow, 2014.
- Order of the Ministry of Health of the Russian Federation dated December 29, 2014 No. 951 “On approval of methodological recommendations for improving the diagnosis and treatment of respiratory tuberculosis”
- S.N. Skornyakov (chairman), M.V. Shulgina (coordinator), B.M. Ariel, G.S. Balasanyants, D.V.Vakhrusheva, A.V. Vladimirov, V.B. Galkin, L.M. Grinberg, V.Yu. Zhuravlev, M.A. Kravchenko, S.Yu. Krasnoborova, A.V. Mordyk, T.I. Petrenko: Clinical guidelines for the etiological diagnosis of tuberculosis - 2014.
- National Association of Phthisiatricians: Clinical Guidelines for the Diagnosis and Treatment of Respiratory Tuberculosis in Adults - 2013.
- Analytical review on tuberculosis. 2011. M., 2003 https://www.mednet.ru/images/stories/files/CMT/tbreview2011.pdf
- WHO: The Stop TB Strategy https://www.who.int/tb/strategy/stop_tb_strategy/en/National Center for
- National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Division of Tuberculosis Elimination.Tuberculosis Disease FactSheets. https://www.cdc.gov/tb/publications/factsheets/testing/diagnosis.htm
- Peter J, Green C, Hoelscher M, Mwaba P, Zumla A, Dheda K. Urine for the diagnosis of tuberculosis: current approaches, clinical applicability, and new developments. Curr Opin Pulm Med. 2010;16(3):262-270. doi:10.1097/MCP.0b013e328337f23a
For your information:
Mycobacterium is a living organism with a set of diverse and sophisticated adaptation mechanisms that are sensitive to environmental changes. Damaging external influences are countered by means of protection, leading to the emergence of a biologically transformed version of the pathogen, the identification of which requires new methods.
The diagnostic sensitivity of this method can be increased by examining multiple sputum samples from the same patient. A negative bacterioscopy result does not exclude the diagnosis of tuberculosis, since the sputum of some patients contains less mycobacteria than can be detected by microscopy. Poor preparation of sputum smears can also be the cause of a negative bacterioscopy result.
Telephone
What it is?
The content of the article
Tuberculosis of the kidneys and urinary tract is one of the most common types of extrapulmonary type of this disease. Mycobacteria penetrate the kidneys hematogenously from a hidden source of infection, so diagnosis is often made at later stages.
The first signs appear in the cortical layer of the organ - these are characteristic tubercles. Often only one of the two is affected, much less often both. Later, the process begins to develop rapidly, involving the ureters and bladder.
Drug treatment
The drug treatment regimen consists of several types of effects on the body:
- anti-tuberculosis drugs (Isoniazid, Rifampicin, Ethambutol, Pyrazinamide);
- angioprotectors to reduce vascular permeability (Detralex, Aescusan);
- antibiotics from the aminoglycoside group (Streptomycin, Kanamycin, Neomycin);
- drugs to enhance immunity (Ribomunil, Imudon);
- non-steroidal anti-inflammatory drugs (Ibuprofen, Ketofen).
- vitamins.
The regimen for taking anti-tuberculosis drugs depends on the type:
- main (first row) – highly effective and low toxic.
- reserve (second row) - ineffective, but highly toxic.
Reserve drugs are prescribed when the patient has an individual intolerance to main-line drugs. Or when the pathogen is highly resistant to chemotherapy.
At the initial stage, you need to use injections, later you can take medications in tablets.
Complications
- Chronic renal failure
due to the death of nephrons. - Amylodoise.
Deposition of insoluble protein in the kidney tissue, leading to disruption of basic functions. - Rejuvenation.
Areas affected by calcium salts form tuberculomas, which begin to cause a complete cessation of fluid outflow. Treatment is only surgical with removal of the affected organ. - Atrophy
. Tissue death followed by degeneration into fibrous tissue with loss of organ functions.
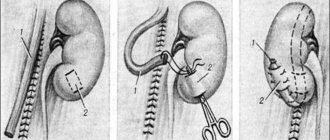
Surgery
If the outflow of urine is impaired, a catheter or drainage is installed. If nephrostomy does not help and the damage process leads to irreversible destructive consequences, then the question arises of surgery to remove the organ.
Before and after the scheduled operation, anti-tuberculosis therapy must be carried out for a month to delay the development of infection and protect a healthy kidney. The operation is partial (with the removal of one segment or cavity) or radical (complete removal of the organ).
Classification
Tuberculosis of the kidneys and urinary tract is classified into stages depending on the degree of development and manifestations of the disease:
- Parenchymal tuberculosis
. The initial form without organ destruction, the prognosis for cure is favorable. - Tuberculous papillitis.
It can be either one-sided or two-sided. It is characterized by the formation of single cavities or small papillitis, no more than one centimeter. Conservative treatment offers a good chance of cure. - Cavernous.
Damage to one of the kidney segments, characterized by the formation of a subcortical cavity. Clinical manifestations are similar to carbuncle. Usually requires surgery. - Polycavernous.
The presence of several cavities that affect almost the entire organ. Purulent melting with the formation of a fistula, pyonephrosis occurs. Filling of the caverns with calcium salts leads to fusion of the pelvis and ureters, and shrinkage of the kidney.
Causes
There are several reasons why tuberculosis can occur:
- contact with a person suffering from an open form of pulmonary tuberculosis;
- unfavorable living conditions;
- weakened immunity;
- advanced form of pulmonary type;
- consumption of contaminated cow's milk and cattle meat.
Several factors contribute to a decrease in the body’s defense reactions and the development of the disease:
- tobacco smoking, alcoholism, drug addiction;
- hazardous production;
- frequent diseases of the respiratory system;
- diabetes;
- nutritional disorders, lack of vitamins, microelements;
- depressive, neurotic conditions;
- pregnancy;
- hypothermia;
- endocrine diseases;
- unfavorable social and living conditions.
When asked whether kidney tuberculosis is contagious or not, doctors answer in the affirmative. How is the infection transmitted? There are several methods of transmission of infection: airborne, contact-household, hemato-lymphogenous, urogenic.
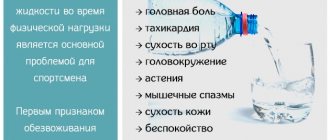
Symptoms and stages
Tuberculosis of the urinary tract is characterized by the absence of specific symptoms, which complicates the diagnosis of the disease. Clinical manifestations depend on the level of damage and the individual characteristics of the patient.
Often, at the primary stage, the disease manifests itself asymptomatically or is hidden under the clinical picture of pyelonephritis or urolithiasis.
Primary symptoms in the initial stages:
- general weakness;
- fast fatiguability;
- low-grade fever;
- constant surges in blood pressure;
- constant dull pain in the lumbar region, lower abdomen;
- frequent urination;
As the disease progresses, more serious signs are added:
- decrease in the volume of urine excreted;
- enuresis;
- pain when urinating;
- signs of intoxication;
- the appearance of blood and pus in the urine.
- a sharp decrease in the patient’s weight;
Diagnostics
Due to the hidden, long incubation period of urinary tract tuberculosis, it is often very difficult to detect in the early stages. But the sooner the mycobacterium and the affected area are identified, the more effective the treatment will be and the prognosis will be more favorable.
Therefore, when complaining of lower back pain, weakness and malaise, the doctor must carry out:
- collect anamnesis - find out about any contacts of the patient with patients with this disease, whether there was such a diagnosis previously in the family, whether there were any animal bites;
- examination and palpation (an enlarged kidney can only be felt in thin people);
- analyze all symptoms;
- order laboratory tests.
To make a correct diagnosis, laboratory tests are necessary:
- clinical blood test (leukocyte level, ESR is important);
- urine analysis according to Nechiporenko (protein, pH level, presence of red blood cells, pyuria);
- PCR and urine culture;
- radiography;
- Ultrasound of the kidneys;
- cystoscopy;
- Diaskin test (provocative tuberculin test).
To determine the exact size of the lesions and affected areas, an additional computed tomography or magnetic resonance imaging is prescribed. Also, the latest modern methods make it possible to determine the localization of lesions, the stage of the disease and the functionality of the organ:
- angiography – gives a complete picture of the renal vascular system;
- excretory urography - an x-ray with a contrast agent will help evaluate the entire functioning of the urinary system;
- nephroscintigraphy - the introduction of radioisotopes and tracking through a gamma camera provides a complete picture of the functionality of the renal structures.