general characteristics
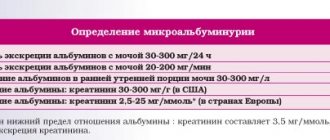
Microalbuminuria is the excretion of albumin in the urine in the amount of 30-300 mg per day. Microalbuminuria is an early sign of renal dysfunction and is one of the manifestations of target organ damage (an indicator of endothelial dysfunction, insulin resistance and hypercoagulation). This early nephropathy is potentially reversible with strict glycemic control and adequate antihypertensive therapy. Persistence of microalbuminuria during antihypertensive therapy is associated with a worse prognosis.
Total protein in urine
This is a clinical and laboratory sign of kidney damage, used to diagnose kidney diseases and monitor treatment.
English synonyms
Urine total protein, urine protein, 24-Hour Urine Protein.
Research method
Colorimetric photometric method.
Units
G/l (grams per liter), g/day. (grams per day).
What biomaterial can be used for research?
The average portion of morning urine, daily urine.
How to properly prepare for research?
- Do not drink alcohol for 24 hours before the test.
- Avoid taking diuretics for 48 hours before donating urine (in consultation with your doctor).
General information about the study
Total protein in urine is an early and sensitive sign of primary kidney diseases and secondary nephropathies in systemic diseases. Normally, only a small amount of protein is lost in the urine due to the filtration mechanism of the renal glomerulus - a filter that prevents the penetration of large charged proteins into the primary filtrate. While low molecular weight proteins (less than 20,000 daltons) freely pass through the glomerular filter, the supply of high molecular weight albumin (65,000 daltons) is limited. Most of the protein is reabsorbed into the bloodstream in the proximal tubules of the kidney, with the result that only a small amount is ultimately excreted in the urine. About 20% of the protein secreted normally is low molecular weight immunoglobulins, and 40% each is albumin and mucoproteins secreted in the distal renal tubules. Normal protein loss is 40-80 mg per day, the release of more than 150 mg per day is called proteinuria. In this case, the main amount of protein is albumin.
It should be noted that in most cases, proteinuria is not a pathological sign. Protein in the urine is detected in 17% of the population and only 2% of them cause serious illness. In other cases, proteinuria is considered functional (or benign); it is observed in many conditions, such as fever, increased physical activity, stress, acute infectious disease, and dehydration. Such proteinuria is not associated with kidney disease, and protein loss is insignificant (less than 2 g/day). One of the types of functional proteinuria is orthostatic (postural) proteinuria, when protein in the urine is detected only after prolonged standing or walking and is absent in a horizontal position. Therefore, with orthostatic proteinuria, an analysis of total protein in the morning urine will be negative, and an analysis of 24-hour urine will reveal the presence of protein. Orthostatic proteinuria occurs in 3-5% of people under 30 years of age.
Protein in the urine also appears as a result of its excess production in the body and increased filtration in the kidneys. In this case, the amount of protein entering the filtrate exceeds the possibilities of reabsorption in the renal tubules and is ultimately excreted in the urine. This “overflow” proteinuria is also not associated with kidney disease. It can accompany hemoglobinuria with intravascular hemolysis, myoglobinuria with muscle tissue damage, multiple myeloma and other plasma cell diseases. With this type of proteinuria, it is not albumin that is present in the urine, but some specific protein (hemoglobin in hemolysis, Bence Jones protein in myeloma). In order to identify specific proteins in urine, a 24-hour urine test is used.
For many kidney diseases, proteinuria is a characteristic and constant symptom. According to the mechanism of occurrence, renal proteinuria is divided into glomerular and tubular. Proteinuria, in which protein in the urine appears as a result of damage to the basement membrane, is called glomerular. The glomerular basement membrane is the main anatomical and functional barrier to large and charged molecules; therefore, when it is damaged, proteins freely enter the primary filtrate and are excreted in the urine. Damage to the basement membrane can occur primarily (in idiopathic membranous glomerulonephritis) or secondary, as a complication of a disease (in diabetic nephropathy due to diabetes mellitus). The most common is glomerular proteinuria. Diseases accompanied by damage to the basement membrane and glomerular proteinuria include lipoid nephrosis, idiopathic membranous glomerulonephritis, focal segmental glomerular sclerosis and other primary glomerulopathies, as well as diabetes mellitus, connective tissue diseases, post-streptococcal glomerulonephritis and other secondary glomerulopathies. Glomerular proteinuria is also characteristic of kidney damage associated with certain medications (non-steroidal anti-inflammatory drugs, penicillamine, lithium, opiates). The most common cause of glomerular proteinuria is diabetes mellitus and its complication – diabetic nephropathy. The early stage of diabetic nephropathy is characterized by the secretion of a small amount of protein (30-300 mg/day), the so-called microalbuminuria. As diabetic nephropathy progresses, protein loss increases (macroalbuminemia). The degree of glomerular proteinuria varies, often exceeding 2 g per day and can reach more than 5 g of protein per day.
When protein reabsorption function in the renal tubules is impaired, tubular proteinuria occurs. As a rule, protein loss with this option does not reach such high values as with glomerular proteinuria, and amounts to up to 2 g per day. Impaired protein reabsorption and tubular proteinuria are accompanied by hypertensive nephroangiosclerosis, urate nephropathy, intoxication with lead and mercury salts, Fanconi syndrome, as well as drug-induced nephropathy when using non-steroidal anti-inflammatory drugs and some antibiotics. The most common cause of tubular proteinuria is hypertension and its complication – hypertensive nephroangiosclerosis.
An increase in protein in the urine is observed in infectious diseases of the urinary system (cystitis, urethritis), as well as in renal cell carcinoma and bladder cancer.
The loss of a significant amount of protein in the urine (more than 3-3.5 g/l) leads to hypoalbuminemia, a decrease in blood oncotic pressure and both external and internal edema (edema of the lower extremities, ascites). Significant proteinuria provides an unfavorable prognosis for chronic renal failure. Persistent loss of small amounts of albumin does not cause any symptoms. The danger of microalbuminuria is the increased risk of coronary heart disease (especially myocardial infarction).
Quite often, as a result of a variety of reasons, the analysis of morning urine for total protein is false positive. Therefore, proteinuria is diagnosed only after repeated testing. If two or more tests of the morning urine sample are positive for total protein, proteinuria is considered persistent, and the examination is supplemented by an analysis of 24-hour urine for total protein.
Testing morning urine for total protein is a screening method for detecting proteinuria. It does not allow assessment of the degree of proteinuria. In addition, the method is sensitive to albumin, but does not detect low molecular weight proteins (for example, Bence Jones protein in myeloma). In order to determine the degree of proteinuria in a patient with a positive morning urine sample for total protein, 24-hour urine is also tested for total protein. If multiple myeloma is suspected, 24-hour urine is also analyzed, and it is necessary to conduct additional research for specific proteins - electrophoresis. It should be noted that analysis of 24-hour urine for total protein does not differentiate the variants of proteinuria and does not reveal the exact cause of the disease, so it must be supplemented with some other laboratory and instrumental methods.
What is analysis used for?
- For the diagnosis of lipoid nephrosis, idiopathic membranous glomerulonephritis, focal segmental glomerular sclerosis and other primary glomerulopathies.
- For the diagnosis of kidney damage in diabetes mellitus, systemic connective tissue diseases (systemic lupus erythematosus), amyloidosis and other multiorgan diseases with possible kidney involvement.
- For the diagnosis of kidney damage in patients at increased risk of chronic renal failure.
- To assess the risk of developing chronic renal failure and coronary heart disease in patients with kidney disease.
- To assess renal function during treatment with nephrotoxic drugs: aminoglycosides (gentamicin), amphotericin B, cisplatin, cyclosporine, non-steroidal anti-inflammatory drugs (aspirin, diclofenac), ACE inhibitors (enalapril, ramipril), sulfonamides, penicillin, thiazide, furosemide and some others.
When is the test scheduled?
- For symptoms of nephropathy: edema of the lower extremities and periorbital region, ascites, weight gain, arterial hypertension, micro- and gross hematuria, oliguria, increased fatigue.
- For diabetes mellitus, systemic connective tissue diseases, amyloidosis and other multi-organ diseases with possible kidney involvement.
- With existing risk factors for chronic renal failure: arterial hypertension, smoking, heredity, age over 50 years, obesity.
- When assessing the risk of developing chronic renal failure and coronary heart disease in patients with kidney disease.
- When prescribing nephrotoxic drugs: aminoglycosides, amphotericin B, cisplatin, cyclosporine, non-steroidal anti-inflammatory drugs, ACE inhibitors, sulfonamides, penicillins, thiazide diuretics, furosemide and some others.
What do the results mean?
Reference values
Concentration: 0 - 0.14 g/l.
Excretion: 0.15 g/day.
Reasons for increased levels of total protein in urine:
1. Kidney diseases:
- primary kidney diseases: lipoid nephrosis, idiopathic membranous glomerulonephritis, focal segmental glomerular sclerosis, IgA glomerulonephritis, membranoproliferative glomerulonephritis, pyelonephritis, Fanconi syndrome, acute tubulointerstitial nephritis;
- kidney damage in systemic diseases: diabetes mellitus, arterial hypertension, systemic connective tissue diseases, amyloidosis, post-streptococcal glomerulonephritis, preeclampsia, urate nephropathy, malignant neoplasms (lungs, gastrointestinal tract, blood), sickle cell anemia, etc.;
- kidney damage during treatment with nephrotoxic drugs: aminoglycosides, amphotericin B, cisplatin, cyclosporine, non-steroidal anti-inflammatory drugs, ACE inhibitors, sulfonamides, penicillins, thiazides, furosemide and some others;
- kidney damage due to poisoning with lead and mercury salts;
- renal cell carcinoma.
2. Increased protein formation and filtration in the body (overflow proteinuria):
- multiple myeloma, Waldenström's macroglobulinemia;
- hemoglobinuria with intravascular hemolysis;
- myoglobinuria due to damage to muscle tissue.
3. Transient (benign) proteinuria:
- dehydration, stress, high protein diet, significant physical activity, fever;
- orthostatic proteinuria.
4. Other reasons:
- congestive heart failure, subacute infective endocarditis;
- hyperthyroidism;
- diseases of the central nervous system;
- bladder cancer;
- intestinal obstruction;
- trauma and others.
A decrease in the level of total protein in the urine is not diagnostically significant.
What can influence the result?
A false positive indicator can be obtained when:
- use of medications (aspirin, chlorpromazine, penicillin, radiocontrast agents, sodium bicarbonate, sulfonamides, acetazolamide);
- with macrohematuria, leukocyturia;
- when the sample is contaminated with copious urethral and vaginal discharge (including purulent), sperm, feces.
A false negative result is caused by:
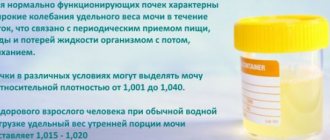
- low relative density of urine (less than 1.015), alkaline reaction of urine (pH more than 7.5), urease-positive microflora (Proteus mirabilis, Proteus vulgaris);
- the presence of specific proteins (Bence Jones protein, myoglobin).
Important Notes
- The urine total protein test is very sensitive to albumin but is not designed to detect Bence Jones protein, globulins, or mucoproteins.
Also recommended
- General urine analysis with sediment microscopy
- Complete blood count (without leukocyte formula and ESR)
- Antibodies to nuclear antigens (ANA), screening
- Antistreptolysin O
- Complement component C3
- Complement component C4
- Erythrocyte sedimentation rate (ESR)
- Plasma glucose
- Serum albumin
- Total cholesterol
- Potassium, sodium, chlorine in serum
- Ionized calcium
- Serum phosphorus
- Serum uric acid
Who orders the study?
General practitioner, nephrologist, endocrinologist, cardiologist.
Literature
- Naderi AS, Reilly RF. Primary care approach to proteinuria. J Am Board Fam Med. 2008 Nov-Dec;21(6):569-74.
- Johnson DW. Global proteinuria guidelines: are we nearly there yet? Clin Biochem Rev. 2011 May;32(2):89-95.
- Chernecky CC Laboratory Tests and Diagnostic Procedures / S.S. Chernecky, V.J. Berger; 5th ed. — Saunder Elsevier, 2008.
- Kashif W, Siddiqi N, Dincer AP, Dincer HE, Hirsch S. Proteinuria: how to evaluate an important finding. Cleve Clin J Med. 2003 Jun;70(6):535-7, 541-4, 546-7.
- Carroll MF, Temte JL. Proteinuria in adults: a diagnostic approach. Am Fam Physician. 2000 Sep 15;62(6):1333-40.
Patient preparation rules
Biological material is accepted during the working day of the departments of ML "DILA". The morning portion of urine is placed in the toilet. All subsequent urine, including the morning portion of the next day, is collected in a clean urine collection container. During collection, store the container in a cool place, protected from light and children. After collecting the last portion, mix all collected urine, measure its volume and record it. Pour 30-40 ml and deliver to the nearest branch of the medical clinic "DILA" within 2 hours. Maybe:
To collect daily urine, the patient is asked to purchase a container with a volume of 2.0 liters at the price price (the cost of the container is not included in the cost of the study).
Random urine:
Any amount of urine, regardless of the time of day. Urine is collected after toileting the external genitalia.
You can add this study to your cart on this page