Birth injuries of newborns are a group of pathologies associated with damage to the child’s body as it passes through the birth canal or is removed from the mother’s womb. The reasons for the appearance are many factors: the anatomical and physiological characteristics of the woman, the biomechanism of the patient’s childbirth, the incompetence of medical personnel, etc. There are different types of birth injuries, but they all have a significant impact on the health of the child.
The consequences of birth trauma can manifest as developmental delays, severe deformities, and the inability to move independently and care for oneself. Symptoms of the disease are not always detected immediately after birth; sometimes they appear as the child grows and develops. For timely diagnosis and correction of pathological abnormalities, it is recommended to make an appointment with a doctor and, if necessary, undergo sessions of osteopathic procedures.
Causes
Birth injuries in newborns are most often caused by the non-physiological course of the labor period in a woman. The immediate causes are usually:
- disruption of labor (violent, weak or discoordinated);
- traction of the child with forceps or vacuum extraction;
- violation of the technique of performing a cesarean section and pulling the baby by the head through an incision on the uterus that is too small;
- acceleration of labor by drug stimulation or “squeezing” the fetus out of the uterus by pressing on the abdominal wall;
- clinically or anatomically narrow pelvis in a woman;
- asymmetry of the pelvis, limitation of physiological mobility of the sacrum during childbirth;
- epidural anesthesia;
- breech presentation of the fetus.
The listed reasons lead to difficulty in passing through the mother’s genital tract during childbirth, contributing to trauma, or directly cause injury to the child due to external mechanical influence.
Predisposing factors of birth trauma
Factors that indirectly influence the risk of injury during childbirth are considered predisposing. These include obstetric and somatic diseases in women:
- pathologies of the endocrine and cardiovascular system – diabetes mellitus, arterial hypertension;
- bad habits;
- malnutrition during pregnancy;
- the presence of foci of infection, including sexually transmitted infections;
- poor physical fitness of the expectant mother;
- anomalies in the structure of the reproductive system.
The likelihood of birth injury is also increased in premature or post-term newborns with large body weight, with intrauterine infection of the fetus and fetoplacental insufficiency. In this case, even with the normal course of labor, serious birth injuries in children are possible.
Hemorrhage into the adrenal glands
Pathology of the adrenal glands is the result of thrombosis of the veins of this organ or necrological processes occurring in the glands. It is characterized as a rather dangerous disease, which occurs relatively rarely in the adult population. This is mainly the prerogative of newborns and young children.
Sometimes in adults this disease can manifest itself as a secondary disease, against the background of another progressive disease. Its painful symptoms may be associated with the extent of the affected organ area and the duration of bleeding.
In the initial stage, it is quite difficult to identify this pathology, so if you do not take drastic measures to identify the cause and prescribe treatment, the prognosis is very depressing; death can occur within two days.
The causes of hemorrhage in the adrenal glands in adults can be characterized by several factors:
- Half of the occurrences of this pathology occur due to: stress, heart failure and myocardial infarction.
- Bleeding can occur with infectious lesions of the adrenal glands.
- Severe pregnancy associated with toxicosis, bleeding before and after childbirth, torsion of an ovarian cyst, as well as self-termination of pregnancy.
- If both adrenal glands are simultaneously affected in paired organs, this can provoke malignant neoplasms or tuberculosis.
- Quite often, hemorrhages occur during inflammatory processes of the gastrointestinal tract and cirrhosis of the liver.
- Injuries received during road accidents and at work can lead to hemorrhages.
As a rule, most patients complain of acute pain in the lumbar region, chest, and hip. Dizziness, nausea and vomiting, general weakness occur, and blood pressure can drop and rise sharply. External signs of pathology are rashes on the skin of bloody spots that merge into plaques. Quite often, patients develop a fever.
Hemorrhage into the adrenal glands. Source: bolimed.ru
If the above symptoms appear, the patient is urgently hospitalized. Here, data preceding the disease is immediately collected. Biochemical and instrumental diagnostics are prescribed, which includes MRI and CT. The blood is tested for the level of cortisol hormones, which plays a major role in this case.
Treatment is aimed primarily at lowering the temperature to reduce blood loss. This is followed by intravenous and drug therapy. If these methods do not bring a positive result, then the only possible option to save a person’s life is surgical intervention.
Pathology of newborns
This pathology is especially dangerous for newborns. Since untimely diagnosis and treatment can lead to the development of chronic adrenal insufficiency, and in severe cases, almost one hundred percent death.
This disease is registered in 20% of newborns; as a rule, this is a difficult birth with a breech baby. It is diagnosed in both boys and girls. An adrenal hematoma in a newborn is quickly saturated with calcium salts, which leads to its hardening.
According to medical research, this pathology is caused by a number of reasons, among which two main ones stand out:
- Damage to the body by infectious diseases, these include: measles, typhoid fever, scarlet fever. As these diseases progress, the inner surface of the blood vessels is affected by toxins. Blood clotting increases, which inevitably leads to the formation of blood clots; the vessels stop supplying oxygen to the body, resulting in numerous hemorrhages.
- Quite often, hematomas in the adrenal glands occur during difficult childbirth and medical errors. Their failure to provide the necessary assistance to the child in a timely manner led to oxygen starvation. The result is damage to the adrenal glands by decay products and the formation of hematomas. The risk group also includes newborns with entanglement in the umbilical cord, congenital diabetes mellitus, and infants whose umbilical cord was cut before the blood pulsates completely.
Symptoms
Damage to the adrenal glands in newborns is divided into several stages, each of which is characterized by the following symptoms.
- During the first stage, pigmentation of the baby’s skin and mucous membranes occurs. His appetite worsens, his blood pressure drops sharply, which can be normalized by administering adrenal hormones, which stop being produced during hemorrhage.
- If such therapy is not carried out, then in the second stage the baby’s temperature rises to critical levels and vomiting begins. As a result, the body becomes dehydrated, urine practically does not pass away, and convulsions are possible.
- The most dangerous is the third stage, during which the child falls into a coma, urination is completely absent, a state of shock sets in and the temperature drops. This is almost always accompanied by death.
There are several forms of this pathology: meningoencephalitic, cardiovascular, gastrointestinal and mixed. Each of them has its own signs and symptoms.
Classification of birth injury
The type of birth injury affects the symptoms and treatment tactics of the child. In clinical practice, there are several classifications of birth injuries in children that systematize childhood postpartum trauma, but the anatomical division is generally accepted.
Hypoxic injuries associated with acute or chronic oxygen starvation of the child’s body, especially nervous tissue, are considered separately. There are no visible birth defects. Violations occur at the physiological and biochemical level.
Let's look at what types of birth injuries there are depending on the anatomical location.
Birth trauma of soft tissues
This group of pathologies makes up the vast majority of injuries during childbirth. They are characterized by damage to the skin, subcutaneous fat, ligaments, muscles and fascia due to compression or overstretching and occur during passage through the birth canal or as a result of physical impact during obstetric care.
Birth injuries of soft tissue include various hemorrhages. The most common cephalohematoma is the accumulation of blood in a pocket between the periosteum and the overlying soft tissues in the parietal or temporo-occipital region. At first, it looks like a natural birth tumor, but has clear edges and does not go away for a long time.
Less commonly observed are the consequences of childbirth in the form of damage to the sternocleidomastoid muscle (spasmodic torticollis) or the chewing muscles of the face. These birth injuries to newborns are less dangerous than damage to the nervous or skeletal system and internal organs. They often go away on their own.
Traumatic brain birth injury
This group of injuries is a dangerous form of birth trauma in a child. Such birth injuries in newborns occur infrequently, but 30% of them are fatal, especially in children born before the normal gestational age.
Damage to bone structures is represented by fractures of the bones of the skull and facial area; it is extremely rare that the scaly part of the occipital bone can be torn off. The severity of the injury depends on the location and extent of the injury.
Intracranial birth trauma comes in several types:
- hemorrhages in the epi- and subdural space;
- damage to the tentorium (tentorium cerebellum) in the form of hyperextensions, ruptures and hemorrhages;
- ruptures of veins and plexuses;
- brain compression.
Intracranial birth injury is caused by various factors, but the main ones are violation of obstetric technique, the use of auxiliary methods of obstetric care, a large fetus and breech presentation.
Injuries of the skeletal system
Common types of birth injuries in children include collarbone fractures. They are caused by difficulty in passing the shoulder girdle through the birth canal due to the discrepancy between the size of the mother's pelvis and the volume of the fetus. Clavicle fractures usually occur in the outer third without displacement of the fragments. Sometimes obstetricians have to specifically break the collarbone for vital reasons in order to help the baby be born.
Femur fractures are less common. The reason is the removal of the child by the pelvic end with excessive traction. In this case, the bone breaks, and the fragments are displaced in different directions. Trauma in a child can also be represented by fractures of the tibia (tibia and fibula).
Injuries to the internal organs of a newborn
Internal organs are most often damaged in large or post-term babies, especially with breech presentation. Common birth injuries include injuries to the liver, adrenal glands, and spleen.
Liver damage occurs when the head is removed when the organ experiences excess pressure. In this case, hemorrhages occur under its capsule - subcapsular hematomas. When a hematoma ruptures, profuse intra-abdominal bleeding occurs, and if it is intact, the injury may go unnoticed. In the postpartum period, routine baby care procedures can contribute to its rupture and subsequent bleeding. Less commonly observed are intrahepatic hematomas or ruptures of the liver lobes.
Birth traumatic injuries of the adrenal glands are manifested by hemorrhages in the tissue of the organ. A hematoma most often forms in one of the adrenal glands in its capsule or cortex. Sometimes it can rupture into the retroperitoneal tissue with the formation of a new hematoma outside the site of its original formation.
Birth trauma to the spleen manifests itself in the form of partial ruptures in the area of the capsule and root of the organ. In rare cases, in premature babies or with hemolytic disease of the newborn, complete avulsions of the spleen occur with profuse bleeding.
Birth injury of the spinal cord and spine
Spinal injuries are the most common complication of non-physiological childbirth. Fractures of the spinal column occur in the upper or lower cervical and upper thoracic region. Injuries to the lumbosacral region are less common. A common type of neck injury during childbirth is subluxation of the first vertebrae with a displacement relative to the normal axis of the spine.
Cervical injuries occur during breech presentation or attempts to extract the fetus through the natural birth canal due to labor anomalies. Traction on the head during slow passage of the child leads to excessive flexion or extension, and in the case of traction on the pelvic end, the child’s head is well fixed in the birth canal, and it has to overcome the resistance of soft tissues with the help of non-physiological movements (hyperextension, flexion, rotation). In this case, the load on the spinal column is distributed unevenly, and the greatest mechanical impact occurs on its upper parts, which leads to neck injuries during childbirth.
Birth injuries to the spine in newborns also occur during cesarean section, when the baby is pulled by the head from the uterine cavity. Neck injuries in such situations are represented by vertebral subluxations and hemorrhages in the ligamentous apparatus with subsequent pinching of the spinal nerves. Undoubtedly, an emergency caesarean section is more traumatic for a child when his head is already firmly inserted into the birth canal.
Hemorrhages in the spinal cord are more common with obstetric aids (forceps, vacuum extraction) or breech presentation of the fetus and are observed in 40% of cases. According to the mechanism of development, they are classified as mechanical birth injuries. These injuries occur at any level of the spinal canal, but cervical and thoracic localization is more common.
Based on their location relative to the structures of the spinal cord, epidural, subdural and subarachnoid hemorrhages are distinguished. Until now, medicine does not have a clear understanding of the immediate causes of hemorrhage of a certain localization, but it is believed that not only the fact of the presence of spinal injuries in newborns, but also anatomical and physiological factors play a role in the mechanism of their development: pneumopathy, venous congestion of the plexuses, extreme prematurity.
Spinal cord ischemia and neuronal death may also be a late consequence of natal neck trauma during childbirth. When the cervical spine is damaged, hemorrhage occurs in the intervertebral discs and the canal where the vertebral arteries pass. During movements of the child's head, compression of the arterial vessels supplying the spinal cord occurs, which leads to episodes of oxygen starvation of certain segments. Ischemia after cervical birth injury leads to persistent neurological and movement disorders.
Birth trauma of the dura mater
One of the most common injuries during childbirth is damage to the dura mater. This structure resembles a tight elastic stocking surrounding the brain and spinal cord. It is also called the dural sac, from the Latin dura mater. At the level of the tissue structure, microtears occur in it. The reason is excessive stretching of the spine (usually the neck) when removing the child from the birth canal.
Birth trauma of the peripheral nervous system
Damage to the peripheral nervous system includes types of birth injuries with damage to the nerves responsible for the motor and sensory spheres. Postpartum neuropathy is often associated with damage to the brachial plexus. Injury to nerve fibers occurs during breech and breech presentations when obstetric care is provided or shoulders are wedged into the birth canal. Depending on the location of the damage to the brachial plexus, paralysis and paresis are observed at different levels (Erb's, Klumpke's palsy). The most severe forms of paralysis of the upper body and limbs occur when the injury is simultaneously localized in the spine and brachial plexus.
Cranial nerves can also be damaged during childbirth. For example, severe compression of the back of the head can lead to excessive compression and damage to the hypoglossal nerve, which usually manifests as difficulty swallowing, choking, and subsequently speech disorders. After incorrect use of forceps during cephalic presentation, damage to the facial nerve passing in the temporomasticatory region may occur. In this case, paresis occurs, caused directly by compression of the nerve with forceps and swelling of the soft tissues around. It is easy to notice by the asymmetry of the child’s facial expressions.
Ultrasound characteristics of the adrenal glands in newborns
Introduction
In the process of adaptation of newborns to extrauterine life, the endocrine system plays a decisive role. The adrenal glands make a significant contribution to ensuring the adaptation of all the most important functional systems of the body of a child of neonatal age. They produce a number of hormonal substances that play a significant role in the implementation of protective and adaptive reactions of the body, stress reactions under stressors, including participation in the mechanisms of adaptation of newborn children to extrauterine life. In this regard, an adequate assessment of the state of the adrenal glands in young children is especially important. Unfortunately, in the domestic and foreign literature there is a small number of works devoted to the problems of imaging the adrenal glands in newborns [1, 2]. In addition, the measurement results given by the authors of these publications differ significantly from each other, which is due to the use of different measurement methods, the level of equipment used and the population of patients examined.
Currently, ultrasound is the optimal diagnostic method in the practice of a neonatologist, given its harmlessness, high informativeness, non-invasiveness, accessibility and ease of implementation [3]. It should be noted that previously used radiographic methods for studying the adrenal glands are now used very limitedly due to the need for special preparation of the child, the harmful effects of radiation and low information content. Thus, echography is the method of choice already at the first stage of application among imaging instrumental diagnostic methods (CT, MRI) [4, 5]. The purpose of the work was to determine the anatomical and echographic parameters of the adrenal glands, including visualization of organ blood flow in healthy newborns and children with a complicated course of the early neonatal period.
The adrenal glands are located retroperitoneally; in newborns, their topography is asymmetrical - the right one is lower than the left, which is sometimes displaced from the upper pole of the kidney to its hilum along the lateral or medial surface [2]. The right adrenal gland often has the shape of a triangle, while the left one resembles a crescent. Externally, the adrenal gland is surrounded by a fibrous capsule of dense fibrous connective tissue, from which connective tissue septa extend into the thickness of the gland. The adrenal stroma consists of loose fibrous connective tissue that supports epithelial cells and contains a huge number of blood capillaries with fenestrated endothelium, the parenchyma is a collection of epithelial cells that have different structures at different distances from the adrenal capsule.
The blood supply to the adrenal cortex comes from three sources: the superior adrenal artery (a branch of the inferior phrenic artery), the middle adrenal artery, which arises directly from the abdominal aorta, and the inferior adrenal artery (a branch of the renal artery). The outflow of venous blood occurs through the central adrenal vein. The central vein of the right adrenal gland (about 1 cm long) drains into the inferior vena cava, and the vein of the left adrenal gland, which is slightly longer than the right (2–4 cm), drains into the renal vein. Numerous small veins emerge predominantly from the left adrenal gland, which flow into tributaries of the portal vein.
The human adrenal glands have a unique structure, consisting of two glands united together, which consist of a cortical and medulla layer. During embryogenesis, the suprarenal anlage (a derivative of the neuroectoderm), which forms the medulla, and the interrenal anlage (a derivative of the mesoderm), from which the adrenal cortex develops, come together. The cortical layer is laid down at 4–5 weeks of intrauterine development in the form of a thickening of the coelomic epithelium; at 6–7 weeks it loses connection with the lining of the coelom and forms a primordium in the form of a compact accumulation of cells - the interrenal organ.
From the end of the 7th week, two zones are formed in the cortex - the outer (definitive cortex) and the inner (fetal cortex). From the 6th to the 20th week, the mass of the adrenal gland increases 170 times, mainly due to the growth of the fetal cortex, which makes up about 87% of the mass of the organ. Subsequently, the growth of the adrenal gland occurs due to the constant cortex: from the 22nd to the 34th week, its thickness increases by 160%, while the thickness of the fetal cortex does not change. During the first months of postnatal development, death and resorption of cells of the fetal cortex occur, due to which by the end of the second week the mass of the adrenal gland decreases by more than 2 times, and by the end of the first year of life the thickness of the fetal cortex is only 16–20% of the initial level [6 ].
The medulla develops from para-aortic sympathoblasts, which differentiate into chromaffinoblasts. Starting from 6–7 weeks, these cells actively grow deep into the developing adrenal cortex towards the center of the organ, where they form clusters of various sizes (“brain balls”). Cells of the “brain balls”, under the influence of increased levels of glucocorticoids produced in the cortex, differentiate into chromaffin cells. From 8 weeks, their secretory granules contain only norepinephrine (H cells); from 16 weeks, some noradrenocytes transform into adrenocytes (A-cells), and subsequently the number of the latter increases. During the first years of postnatal life, the processes of cytological differentiation of glandular cells are completed. Despite the fact that the glands are united, their histological and functional development is different [6].
The high functional significance of the adrenal glands is determined by the production of a number of hormonal substances that have a wide variety of biological properties and a wide range of effects on metabolic processes, regulate vital functions and play a significant role in the implementation of protective and adaptive reactions of the body. The production of the hormone cortisol, which is the most important adaptive steroid, is regulated by the pituitary gland with the help of adrenocorticotropic hormone (ACTH), but the activity of the pituitary gland also depends on the amount of cortisol in the blood - by a negative feedback mechanism, an increase in the concentration of cortisol in the blood reduces the production of ACTH by the anterior pituitary gland, which, in in turn, leads to a decrease in the synthesis of cortisol by the adrenal glands. The central nervous system plays an important role in regulating the formation and secretion of ACTH.
A number of neurotransmitters are involved in this type of regulation, including norepinephrine, acetylcholine and serotonin. Most likely, it is the neurotransmitters that mediate the stress response from ACTH, which stimulates the production of glucocorticoids necessary for adaptation to stress under various influences on the body. With prolonged and particularly life-threatening stress, disruptions may occur in the feedback mechanism that interrupts the secretion of corticosteroids (CS), when the interaction between the nervous and chemical mechanisms is disrupted. It was found that in this case, CS bind to a special blood protein – transcortin (TR). The “CS + TR” connection is delayed by the blood-brain barrier, so the brain stops receiving information about excess CS in the blood and ACTH secretion is not interrupted.
When the negative feedback that limits the growth of CS levels does not work, the stage of exhaustion begins. Excessive accumulation of adrenal hormones in the fluids of the body leads to a disorder of its functions, which gradually spreads to the nervous and endocrine systems, affecting the heart, blood vessels, lungs, and digestive organs. It is assumed that the nature of the pathological syndrome is associated with which parts of the adrenergic system are incompetent and cannot withstand strong stress and what form of disturbance occurs in this case: excitation, exhaustion, the formation of intermediate metabolic products [6, 7, 8]. Thus, the hypothalamic-pituitary-adrenal system is involved in the implementation of mechanisms of adaptation of newborn children to extrauterine life, which determines the importance and necessity of studying the adrenal glands in children in the perinatal period.
Material and research methods
A comprehensive ultrasound examination of the adrenal glands in newborns was carried out on the basis of the perinatal center of City Clinical Hospital No. 7. An expert-class ultrasound machine M-Turbo (SonoSite, USA) with a linear broadband sensor with a frequency of 10–16 MHz was used. The adrenal glands were determined by placing the sensor between the anterior and middle axillary lines. During longitudinal scanning, the height and width of the organ were assessed, and during transverse scanning, its thickness was assessed [2].
The study included 167 newborns (71 girls and 96 boys). The first group (comparison group) consisted of 79 newborns with an uncomplicated course of the early neonatal period. Among the children in this group, 60 newborns were full-term, 19 were premature with a gestational age of 33–37 weeks. The body weight at birth of premature children in the comparison group ranged from 1870 to 3790 g (body length 42–52 cm), and that of full-term children – from 2150 to 4220 g (body length 45–54 cm). All children included in the comparison group were conditionally healthy at the time of the study or had minor deviations in their health status: mild disturbances of hemocerebrospinal fluid dynamics without structural changes, conjugation jaundice of the 1st degree - or were in the department for the purpose of nursing.
The second (main) group consisted of 88 newborns, including 16 full-term children and 72 premature children. The number of preterm infants included 12 infants born at 25–28 weeks of gestation, 26 preterm infants with a gestational age of 29–32 weeks, and 34 infants born at 33–37 weeks of gestation. The birth weight of premature infants 25–28 weeks of gestation ranged from 790 to 990 g (body length 33–34 cm); children 29–32 weeks of gestation – from 1060 to 2190 g (body length 35–42 cm); premature babies with a gestational age of 33–37 weeks – from 1610 to 3290 g (body length 42–51 cm). The body weight at birth of full-term children of the second group ranged from 2540 to 4460 g with a body length of 46 to 57 cm. Children of the second group at the time of the study were characterized by the presence of pathological conditions of the respiratory system (congenital pneumonia), severe ischemic brain lesions of varying severity, including those with structural changes in the central nervous system, that is, they were distinguished by a severe, complicated course of the early neonatal period. Among the children in this group, 51 newborns were on mechanical ventilation (the duration of mechanical ventilation ranged from several days to a month), 10 children received oxygen therapy using other methods (tent, nasal catheter). 22 (25%) newborns of the main group had a low Apgar score (less than 5 points). Among the newborns in the comparison group, only 1 child (1.3%) had a low Apgar score. Ultrasound examination of the adrenal glands was carried out at the ages of one, two, three weeks and one month of life in children in order to determine the age-related dynamics of the size of this endocrine gland.
All children examined underwent ultrasound scanning of the adrenal glands in B-mode. During the study, the location of the adrenal glands, their shape, characteristics of the contours of the organ, echogenicity, echostructure, differentiation of layers were assessed, and the linear dimensions used to calculate the volume of the organ were determined: the width of the base of the adrenal gland, its height and thickness (Fig. 1, 2). In addition to the overview ultrasound examination, color and power Doppler mapping was used, and pulsed-wave Doppler measurements of blood flow in the adrenal arteries were performed. The middle adrenal artery (the largest branch of the abdominal aorta) was most often visualized; however, the blood flow parameters in it, according to the literature, do not reliably differ from those in other adrenal arteries [9]. Using the data obtained from survey echography, the total volume of the adrenal glands was calculated by adding the volumes of the right and left glands, calculated according to the formula: V = 0.520 × A × B × C, where A, B, C are the linear dimensions of the adrenal glands (cm), 0.520 – conversion factor calculated experimentally.
During the study, the body surface area was calculated for each child, taking into account weight and height indicators, and the ratio of the total volume of the newborn's adrenal glands to the body surface area was calculated. Statistical processing of the results was carried out using standard methods. Quantitative parameters are presented as arithmetic mean values adjusted for the standard error of the mean (M ± m). Differences in hypotheses were considered significant at the significance level p
Research results and discussion
As a result of the ultrasound examination, the following data were obtained: in healthy full-term and premature children of the first group, the adrenal glands were visualized in a typical place as structures with clear, even contours, predominantly triangular (right) and semilunar (left) in shape, with clear differentiation into hyperechoic cerebral and hypoechoic cortical layers (Fig. 3). In children of the second group, during two-dimensional scanning, the adrenal glands had a normal location; in shape, echostructure and differentiation of layers they were similar to the adrenal glands of newborns of the first group. However, the border between the hyperechoic medulla and the hypoechoic cortex was not always smooth, although it remained clear in all newborns of the second group. It should be noted that in the echostructure of the hyperechoic adrenal medulla in children of the second group, a large number of single hypoechoic inclusions were noted, and in the hypoechoic cortex hyperechoic inclusions were detected (Fig. 4, 5). Particularly pronounced structural changes in the form of uneven contours and heterogeneity of the organ structure due to inclusions were noted in a study of 10 very premature children of the second group, which constitutes 83% of the total number of examined children with a gestational age of 25–28 weeks. Among other categories of premature babies included in the main group, these echographic changes were also detected in most cases, although they were less pronounced: in 18 newborns 29–32 weeks of gestation, which is 69%; in 19 children 33–37 weeks of gestation (56%). Full-term children of the second group were characterized by similar features of the ultrasound picture, however, among this category of patients they were observed much less frequently (in 5 (31%) children).
During an echographic study in B-mode, the linear dimensions of the adrenal glands were measured: height, width and thickness. When analyzing the data obtained, it was found that the values of the width of the base and height of the adrenal glands fluctuate in a wide range in all examined children. The width of the base of the adrenal glands of children in the comparison group ranged from 5 to 14 mm, the height of the adrenal glands was from 9 to 18 mm, regardless of side. In contrast to the highly variable values of the width and height of the adrenal gland, the value of its thickness in the cross section varied strictly within certain limits. According to the data obtained as a result of the study, the range of scatter of this parameter ranges from 2.0 to 6 mm for children at different stages of early childhood, both conditionally healthy and children with pneumonia and severe hypoxic brain damage. In this regard, the measurement of the thickness of the adrenal gland during its transverse scanning is of key importance for the echographic characterization of this endocrine gland. During the study, it was noted that the maximum thickness in the first group is typical for the first days of a child’s life, and then it decreases (Table 1). The values of adrenal thickness in children in the first and second weeks of life were significantly different on both the right and left sides. There were no statistically confirmed differences in adrenal thickness between other age groups. The thickness parameter values ranged from 2.0 to 6 mm among healthy full-term infants and from 2.0 to 5 mm among healthy preterm infants.
The width of the base and height of the adrenal glands in children of the second group have the same wide range of values as in the first group of patients: in full-term newborns, the width ranged from 7.5 to 17 mm, the height of the adrenal gland - from 9.5 to 21 mm. In premature newborns of the second group, the width ranged from 5 to 13 mm, height - from 5 to 15.5 mm. However, the most significant parameter - the thickness of the adrenal gland during its transverse scanning - in the second group was characterized by relative constancy of values: in full-term - from 2.0 to 6.0 mm, in premature - from 2 to 4.5 mm. During the study, it was noted that the dynamics of the adrenal gland thickness in children of the main group are similar to those examined in the comparison group: the maximum is typical for the first week of a child’s life, with a further decrease by the third week and a slight increase by the month (Table 2). The values of the thickness of the adrenal glands in children in the first and second weeks of life were significantly different (p Using correlation and regression analyzes it was established that there is a strong direct positive correlation between the value of the thickness of the adrenal gland and the value of its volume. The identified pattern allows us to use the thickness parameter as the main characteristic of the adrenal gland when assessing its volume. Based on the measurement of linear values of the adrenal glands, the volumes of the right and left glands were calculated, then the total volume of the adrenal glands was calculated by adding the data obtained. When analyzing and comparing the calculation results, it was found that the change in the total volume of the adrenal glands in children has a certain age-related pattern. Healthy Newborns in the first week of life were characterized by the largest total volume of the adrenal glands compared to other age categories of children in group 1. As a result of calculating the ratio of the total volume to the surface area of the child's body among healthy newborns, the maximum value was also obtained for children in the first week of life. From the eighth day to three weeks of age, there was a decrease in the total volume of the adrenal glands in the group of healthy children, and then a gradual increase in this parameter was noted by the month of life (Table 3). The age dynamics of this indicator in children of the main group are presented in Table 4.
Taking into account the differences in the weight and height parameters of the examined children, in order to obtain an adequate assessment of the volumetric parameters of the adrenal glands, the ratio of the total volume of the adrenal glands to the body surface area of each examined child was calculated (Tables 5, 6). When analyzing the results obtained, it was found that children of the second group are characterized by larger values of the ratio of the total volume of the adrenal glands to the body surface area than in the first group in all age categories. This indicates that per unit body surface area in children with pronounced pathological changes in the body there is a greater value of the total volume of the adrenal glands than in healthy children. When assessing the reliability, statistically significant differences were confirmed between full-term children of the first and second groups at the age of one, three weeks and a month of life. For premature infants 33–37 weeks of gestation with pathological changes and conditionally healthy premature newborns of the same gestational age, no statistically significant differences were found. Probably, the increase in the ratio of the total volume of the adrenal glands to the body surface area in premature children of the main group, born at 25–32 weeks of gestation, is associated with the provision of adaptive neuroendocrine reactions of the adrenal system and the inclusion of compensatory mechanisms in the presence of pathological changes in the body.
A Doppler study in pulse-wave mode was carried out on 64 children of the first group (including 9 premature and 55 full-term newborns) and 66 children of the second group (including 50 premature and 16 full-term newborns). There were no significant differences in blood flow parameters among children of different ages, therefore the data presented in Table 7 are not divided by age. As a result of a biochemical study to determine total cortisol, it was noted that healthy full-term and premature newborns of the comparison group and children of 33–37 weeks of gestation, as well as full-term children of the main group, are characterized by normal levels of this hormone in the blood, that is, its content corresponds to generally accepted reference values in this age group (from 190 to 1300 nmol/l). In premature children from 25 to 32 weeks of gestation with pathological changes in the body, there was a statistically significant decrease in the concentration of cortisol in the blood compared to full-term children of the main group (Table 8). This may indicate a violation of the functional state of the adrenal cortex during the period of a detailed clinical picture of the disease in premature infants of gestational age 25–32 weeks.
It should be noted that, along with low cortisol levels, in the majority of premature newborns from 25 to 32 weeks of gestation with pathological changes in the body, more often than in other categories of subjects, echographic changes in the structure of the adrenal glands are observed in the form of the presence of uneven contours of the gland, as well as blurred borders between layers, heterogeneity of the internal structure with the appearance of hypoechoic inclusions in the medulla and hyperechoic strands and inclusions in the cortex. The data obtained indicate that echographic changes in the structure of the adrenal glands detected in premature newborns with a gestational age of 25 to 32 weeks allow us to predict a possible decrease in cortisol levels in this category of children. The identified feature of this part of the examined individuals indicates the need to determine the concentration of cortisol in the blood in the presence of changes in the structure of their adrenal glands according to echography data.
Thus, the ultrasound research method in pediatric practice is a priority for a comprehensive assessment of the condition of the adrenal glands, since it allows one to evaluate their structural and hemodynamic characteristics. Newborns with various pathological conditions are characterized by a higher ratio of the total volume of the adrenal glands to the body surface area compared to healthy children in the comparison group. In the majority of premature infants from 25 to 32 weeks of gestation with pathological changes in the body, there was a significant significant decrease in the concentration of cortisol in the blood, which indicates functional insufficiency of the adrenal cortex at the height of the pathological process in premature infants of this gestational age. The results obtained during the study suggest that the presence of pathological changes causes activation of the body's adaptive processes, including the reaction of the adrenal system, which is necessary to maintain optimal homeostasis in the body and compensate for existing disorders.
Symptoms and diagnosis
Detection of birth injuries in children is possible at the stage of examination by a neonatologist. In case of severe injuries, the general condition of the child changes, which is a cause for concern. Various methods are used to confirm the diagnosis:
- Monitoring of body functions - heart rate, respiration, biochemical blood parameters, diuresis, gas exchange efficiency.
- Neurological examination.
- Instrumental research methods - ECG, ultrasound, ENMG, radiography, etc.
In some cases, birth injuries are identified in a delayed period. Parents pay attention to problems with the child’s movements, the presence of severe deformations, body asymmetry, frequent profuse regurgitation, general symptoms such as tearfulness, sleep disturbances, refusal to eat, problems with weight gain or mental and physical development.
Signs
Symptoms of birth trauma largely depend on the type of injury and severity. For soft tissue injuries, the main signs are: swelling, pain and hematomas at the site of injury. In the case of fractures, visible skeletal deformation and dysfunction of the injured limb may occur.
Neck and head injuries have the most severe manifestations. In the case of hemorrhage and ischemia, symptoms appear immediately after childbirth in the form of impaired consciousness, breathing, blood circulation and neurological deficit corresponding to the site of injury (paralysis of a certain muscle group, impaired swallowing, changes in muscle tone and reflexes). With subluxations and fractures, compression of the nerve fibers occurs, which cannot always be determined in the early postpartum period.
After discharge from the hospital, symptoms begin to appear in the form of lethargy and atonicity of the muscles, lack of sensitivity when touching the child, or, conversely, increased tone of the muscles of the neck or limbs. At a later date, muscle dystrophy occurs due to motor disorders, constant pain, inability to hold the head, stand and walk.
Injuries to the spine and skull often lead to retardation in mental and physical development, cerebral palsy and neuropathies.
Treatment at Doctor Simkin's Clinic
In our clinic, therapy is aimed at eliminating the causes and unwanted symptoms of birth trauma. The main role in the mechanism of development of such consequences is played by anatomical and physiological disorders in the functioning of the body.
Treatment of birth trauma involves a complex effect on the child’s body. The goal of the course of therapy is not only to get rid of symptoms, but also to find the root cause of pathological changes. Only in this case is it possible to achieve the goals set and restore the child’s lost health.
What does a doctor do
The first stage of work is to examine the child and identify deviations from the norm. They can be caused by both anatomical changes and failures in the coordinated functioning of organ systems. The doctor identifies the most significant areas of osteopathic damage. After the examination, the second stage begins - the use of osteopathic techniques to eliminate the identified problems. An osteopathic doctor influences damaged structures through gentle external influence with his hands.
A child’s body is not yet a formed system. Its work can be compared to a complex mechanism. The cause of a violation of any function is not always associated with a specific part in the violation zone; it is often caused by damage in another area or a failure in the interaction between parts of the whole. The human body also works on this principle.
By influencing certain areas of the body with the help of hands, the doctor corrects pathological changes not only at the site of impact, but also in remote areas of the body. Eliminating tension in muscles and connective tissue leads to improved blood supply to tissues and nerve function. At the same time, existing problems are eliminated and the body’s functioning is “tuned” to a natural physiological way.
When to seek help from an osteopath
It is recommended to visit a doctor after discharge from the hospital, even if the birth proceeded without visible complications. The sooner the child is examined by an osteopath and any changes in the functioning of the body are identified, the easier they are to correct.
This statement is especially true with regard to damage to the skeletal system. Injuries to the head and neck during childbirth are common and easier to correct in infancy, when the child’s bones, ligaments and soft tissues are more pliable and sensitive to external influences, and also before the chain of disorders caused by birth trauma has not gone too far. It is better to carry out a course of osteopathic procedures before the child begins to actively move (6-7 months) in order to avoid the progression of existing pathologies.
Hemorrhages in the adrenal glands
Bilateral hemorrhage into the adrenal glands is the cause of acute adrenal insufficiency. In medical practice, this pathological condition is called Waterhouse-Friderichsen syndrome. Hemorrhage, or hemorrhagic infarction of the adrenal glands, often occurs against the background of a progressive infectious disease in the stage of decompensation.
Acute disruption of the blood supply to the adrenal glands leads to a complete or partial cessation of the formation of gluco- and mineralocorticoid hormones, which regulate water-salt, carbohydrate, immune metabolism and, in general, the homeostasis of the whole organism. Severe dehydration, collapse, neuropsychic and gastrointestinal disorders occur. If assistance is not provided at this stage, acute adrenal insufficiency develops into a coma, which ends in death.
The adrenal glands synthesize a large number of hormones that regulate important parameters of human life.
Causes of hemorrhages in the adrenal glands
In adults, the development of the syndrome is due to the following reasons:
- severe fulminant sepsis;
- extensive burns;
- thrombosis of adrenal vessels;
- systemic connective tissue diseases;
- pathology of pregnancy.
The listed diseases and pathological conditions, if left untreated and with a progressive course, ultimately lead to the formation of disseminated intravascular coagulation syndrome. In the vessels and capillaries of vital organs, the process of thrombus formation begins, blocking blood flow.
Intensive consumption of coagulation factors for the formation of blood clots quickly leads to their deficiency. At the next stage, the blood loses its ability to clot, and some of the formed elements and plasma leave the vascular wall.
This forms a hemorrhagic infarction in the adrenal tissue, which can subsequently become necrotic.
The most common cause of adrenal infarction in both adults and children is generalized meningococcal infection.
Table. Characteristics of the causes and mechanisms of development of hemorrhage in the adrenal glands
| Causes | Pathogenesis of development | Examples of diseases |
| Sepsis | Bacterial toxins, when released into the bloodstream, damage the vascular wall and activate blood clotting factors. | Meningococcal, streptococcal, staphylococcal infections, diphtheria, destructive purulent pneumonia, osteomyelitis, peritonitis and other diseases complicated by the generalization of the infectious process. |
| Burns | Shock from deep burns is accompanied by loss of plasma, decreased blood pressure and thickening of the blood. Toxins from necrotic tissues, entering the bloodstream, trigger the formation of blood clots. | Deep or widespread superficial thermal or chemical burns. |
| Systemic connective tissue diseases | The autoimmune process leads to the formation of circulating immune complexes, which are fixed on the vessel wall and can disrupt blood clotting processes. | Systemic lupus erythematosus, vasculitis, periarteritis nodosa |
| Pathology of pregnancy | In severe forms of gestosis, widespread vascular spasm and immune inflammation of the cells of the vessel wall occur. The result is activation of tissue thromboplastin (clotting factor). | Preeclampsia, eclampsia, amniotic fluid embolism, total placental abruption. |
Any septic or progressive autoimmune disease, any type of shock if medical care is not provided can lead to the formation of intravascular coagulation syndrome, the manifestation of which will be various bleeding and hemorrhages, including in the adrenal glands.
Causes of hemorrhages in the adrenal glands in newborns
In newborns, adrenal gland damage is most often associated with trauma received during childbirth. This can occur during a prolonged period of expulsion of the fetus, clamping of the umbilical cord loops, or the application of obstetric forceps. Incorrect provision of obstetric care at birth (especially with breech presentation) can also cause hemorrhages in the adrenal glands in newborns.
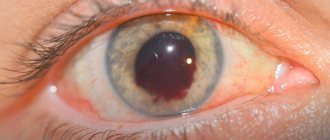
Meningococcal infection is the most common cause of adrenal hemorrhage
Symptoms
Congenital adrenal hyperplasia
The manifestation of symptoms depends on the degree of damage to the adrenal cortex. With total bilateral hemorrhage, the first place will be symptoms of acute adrenal insufficiency, which can develop within a few hours.
Due to a sharp decrease in the synthesis of adrenal hormones, sodium and chloride ions are not absorbed in the intestines and are intensively excreted in the urine during uncontrollable vomiting and diarrhea. Next comes dehydration and shock. Typical symptoms are fever, shortness of breath, cyanosis, and petechial skin rashes.
Depending on the severity of the manifestations, the following variants of adrenal insufficiency are distinguished:
- cardiovascular – tachycardia, hypotension;
- gastrointestinal – sharp abdominal pain, vomiting mixed with blood;
- cerebral – convulsions, nervous disorders, stupor.
In newborns, minor adrenal hemorrhages after a traumatic birth may go undetected. Subsequently, small areas of infarction calcify, and the adrenal gland is completely rebuilt. With massive damage, typical symptoms of acute adrenal insufficiency develop.
Adrenal infarction is accompanied by a state of shock, and if help is not provided to the patient in a timely manner, the risk of death is very high
General principles of treatment
With the development of acute adrenal insufficiency, the complex of treatment measures includes:
- hormone replacement therapy with gluco- and mineralocorticoid drugs;
- fluid therapy to combat dehydration and shock;
- restoration of electrolyte imbalance;
- treatment of concomitant disease (infection, autoimmune disease, etc.).
Treatment of newborns is also based on the use of hormone replacement therapy.
The prognosis for hemorrhages in the adrenal glands is serious, but with adequate and timely treatment, impaired functions can be compensated and possible negative consequences can be minimized.
Source: https://2pochki.com/bolezni/krovoizliyaniya-nadpochechniki-detey-vzroslyh
Consequences with possible complications
The consequences of birth injuries are varied and range from minor to life-threatening. The prognosis largely depends on the type of damage and the degree of its impact on body functions. Soft tissue injuries have a favorable prognosis and resolve quickly, rarely leading to any damage.
The consequences of birth trauma to the neck and head vary widely, from a slight delay in physical development and impaired motor activity of the child due to damage to nerve fibers to cerebral palsy - cerebral palsy. In infants, the consequences of birth injuries are represented by general symptoms in the form of lethargy, decreased or increased muscle tone, decreased motor activity, too early due to hypertonicity or, conversely, late raising of the head. Serious complications of birth trauma include paresis and paralysis of the limbs, muscle dystrophy, and the inability to sit or move.
The main reason why birth trauma is dangerous due to damage to the central nervous system is the high probability of death due to disruption of the vital functions of the body. Even with timely diagnosis and treatment, residual neurological manifestations and mental retardation of the child are possible. Injuries to the neck and head followed by massive hemorrhage in the brain or spinal cord are often fatal in the early postpartum period.
Symptoms of injuries
A newborn, unlike an adult, has pliable bones, because some of them consist of almost half of cartilaginous tissue. What is it for? First of all, to be able to pass through the birth canal, so that the main support of the small body can withstand the loads during childbirth.
For example: the occipital bone is formed by 4 separate bones, which are connected by cartilage, and their complete fusion occurs only by the age of 7. This provides space for the baby's growing brain, as well as adaptation to changes in atmospheric pressure during childbirth, etc.
There is danger hidden in this adaptation mechanism. If something goes wrong, there is a high risk of birth injury. Every child is at risk. Symptoms depend on what kind of injury the baby received.
In case of soft tissue injury, abrasions, scratches, etc. are considered the most common. Diagnosis is carried out during a visual examination of the baby by a neonatologist. As a rule, they are not dangerous, rarely cause complications and require only local treatment. There are also more serious ones, which occur when the fetus is in an unnatural position and are accompanied by swelling and pain.
Other, more complex injuries include:
• Birth tumor – swelling with pinpoint hemorrhages in the parieto-occipital region of the head. Symptoms develop as they pass through the birth canal and disappear within 1–4 days. • Cephalohematoma – hemorrhage in the area of the skull bones. This is a dense, elastic hematoma, but painless.
In case of injury to the musculoskeletal system, the most common are injuries to the collarbone and limbs, and these problems are classified as obstetric birth trauma.
Fractures without displacement are not diagnosed immediately, but only after a while when characteristic symptoms appear: dense swelling, indicating the formation of a callus. And this is a signal for parents, a reason to visit a doctor and rule out injury.
Symptoms of displaced fractures will be: • lack of active movements; • intense, hysterical crying, which is explained by severe pain; • swelling in the area of the fracture.
With such an injury, there is a decrease in basic reflexes, depression of tone and the development of torticollis.
In case of injury to internal organs They arise as a result of a negative external impact on the fetus as a result of a pathological birth process. External signs in newborns appear only after 3 or more days; most often, hemorrhages are detected in the liver and adrenal glands. But as soon as the hematomas rupture, the following symptoms appear: • repeated vomiting; • muscle hypertonicity; • inhibition of some reflexes; • lowering blood pressure, etc.
In case of trauma to the nervous system The concept of birth injury of the spinal cord in newborns includes: hemorrhages, stretching, compression or even rupture at different levels, damage to roots, plexuses, spinal and cranial nerves. Such consequences are associated with various symptoms and are quite serious, but they directly depend on the diagnosis: • decreased muscle tone; • absence of one or more reflexes; • weak cry at birth; • unnatural act of breathing; • paresis or paralysis, etc.
For mild injuries of the central or peripheral nervous system, the prognosis is favorable, although many of them are accompanied by changes in normal muscle tone, inhibition of reflexes and basic motor reactions.
With intracranial birth trauma, for example, hemorrhages, extremely severe symptoms develop, but they depend on the location of the hematoma.
Common signs include: • sudden and sharp deterioration in the condition of children; • change in cry, sounds similar to meowing and moaning appear; • abnormal movements; • thermoregulation disorders; • suppression of reflexes, up to complete absence; • violation of the act of sucking and swallowing; • attacks of suffocation; • tremors and convulsions; • pathological regurgitation and vomiting; • anemia.
If cerebral edema or hematoma increases, death is possible.