What is an eye hemorrhage
Hemorrhage in the eye is a fairly common phenomenon, the cause of which is a violation of the vascular wall of the eyes.
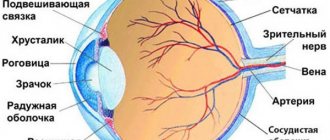
This is an accumulation of blood that has poured out of the blood vessels, filling the cavity of the eyeball, as well as the surrounding tissues. This phenomenon most often occurs in pathological conditions: diseases or injuries. Hemorrhage can be observed in the anterior chamber of the eye, in the vitreous body of the eyeball, as well as in the retina on its posterior wall and directly in the orbit.
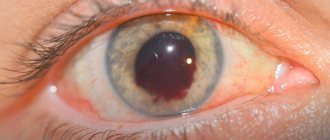
A retinal hemorrhage looks like a bright red spot on the surface of the eyeball. The person usually does not experience any pain. He may sometimes feel a pain, as if a foreign body has entered, and also complain that visual acuity is decreasing.
There are no harmless hemorrhages. Only specialists from microsurgery and ophthalmology can diagnose and cure the disease.
Causes
Blood can only flow from the vessels, so the immediate cause of hemorrhage in the retina is always damage to the choroid that feeds it - a rupture or pathological permeability of the vascular walls (in the latter case, the volume of the accumulating effusion is much less). In turn, the main causes of vascular damage are:
- injuries (including those received during ophthalmic surgery) are statistically the most common factor, the share of which is 75-85%;
- vascular pathology (angiopathy) and the resulting degenerative processes in the retina (retinopathy) as an independent, primary disease;
- secondary angio- and retinopathy that developed as a result of other, more general diseases (diabetes mellitus, arterial hypertension, blood diseases, infections, atherosclerosis, etc.).
The direct consequences of retinal hemorrhage may be infiltrates, swelling, inflammation, etc., but the most likely and dangerous threat (especially when fluid leaks between the retina and the choroid) is retinal detachment, partial or total - which means a sharp deterioration in vision or irreversible blindness.
Separately, as a special form, retinal hemorrhage in newborns is considered, which has a clear cause-and-effect, clinical and prognostic specificity in contrast to “adult” hemorrhages.
Thus, with a worldwide trend toward an increase in the frequency and severity of retinopathy in newborns (especially premature infants), the frequency of postpartum retinal hemorrhages in infants reaches 20-30%. Important statistical patterns were revealed: firstly, such hemorrhages are extremely rare during cesarean section births, and secondly, their probability is much higher (about one and a half times) if a woman gives birth for the first time.
Subsequently, it was confirmed that the main cause of retinal hemorrhage in newborns is the birth itself, or more precisely, the nature of the birth process and methods of delivery. Difficult, complicated, protracted labor associated with compression of the fetal head, as well as mechanical obstetric and gynecological techniques (forceps, vacuum) sharply increase the likelihood of retinal hemorrhage, which is usually noted at 1-2 weeks of life. There were alarming concerns about a possible connection between retinal and brain hemorrhages, but subsequent in-depth studies using tomography fortunately did not find such a connection.
Treatment
Most patients are treated on an outpatient basis, hospitalized only:
- seriously ill patients;
- patients with complications;
- little children;
- people with sickle cell anemia.
The nature of therapy is determined by the cause of hyphema formation, its degree and the presence of complications. As a rule, they initially try to cope with the problem with conservative measures, and if they are ineffective or complications develop, they resort to surgical intervention. But even with a slight hemorrhage in the eye, it is necessary to contact an ophthalmologist in order to protect yourself from the development of undesirable consequences and to speed up the onset of recovery as much as possible.
Attention! You cannot decide on your own to cover the injured eye with a bandage or apply any compress, as this may cause the condition to worsen.
General recommendations
All patients should:
- try to adhere to bed rest;
- sleep with the head of the head raised;
- avoid physical activity;
- do not take painkillers, since almost all of them affect blood clotting;
- on the recommendation of a specialist, cover the injured eye with a soft bandage for two weeks.
To speed up recovery, it is recommended to sleep on a high pillow or otherwise raise the head of the bed so that an angle of 45-60 degrees is formed between the head and the surface of the bed
Drug therapy
If the patient is taking anticoagulants or antiplatelet agents, that is, medications that thin the blood, they are discontinued during the treatment of hyphema. To eliminate traces of hemorrhage, the following is prescribed:
- drops with corticosteroids (Prednisolone, Dexamethasone) - to eliminate the inflammatory process and pain;
- hemostatic agents (Gemaza, Purolaza, aminocaproic acid);
- vascular strengthening drugs (Actovegin, Emoxipin);
- absorbable medications (Mannitol, Glycerol);
- mild pain relievers (Tylenol);
- atropine and drops with β-blockers (Thymol, Acetazolamide) - to normalize intraocular pressure.
If severe pain appears in the affected eye, especially in combination with attacks of nausea and vomiting, you should immediately consult a doctor, as this may be signs of increased intraocular pressure, which requires an immediate response and adjustments to the prescription.
Drops with corticosteroids - the basis of conservative treatment of hyphema - gallery
Sofradex
Pharmadex
Maxitrol
Maxidex
Surgery
Surgery is a last resort. Its implementation is indicated when:
- staining the cornea with blood;
- formation of clots;
- complete filling of the anterior chamber with blood;
- no improvement within 5–10 days of drug treatment;
- increased intraocular pressure and the ineffectiveness of medications to lower it.
Treatment of vitreous hemorrhage
Sudden vision loss requires emergency eye care. However, treatment for vitreous hemorrhage will vary depending on the underlying cause of the bleeding. The primary goals in the treatment of hemorrhage are: diagnostic search and elimination of the source of bleeding; Finding and repairing retinal damage before it leads to permanent vision loss; restoration of normal vision.
1 . Observation . If the source of bleeding is unknown and there is massive hemorrhage in the vitreous body of the eye, the patient is prescribed restrictions on physical activity and bed rest with the head of the bed elevated. A prerequisite for the treatment of vitreous hemorrhage is dynamic observation once every 3-4 days and ultrasound monitoring once every 7 days. Fresh minor hemorrhage into the vitreous body in some cases does not require treatment and resolves on its own within a few days to 1-2 weeks. However, retinal detachment due to hemorrhage should be ruled out urgently.
2 . Conservative methods of treatment of hemorrhages in the vitreous body. Local and systemic therapy for the actual vitreous hemorrhage is not required, since none of the drugs that outpatient ophthalmologists love to prescribe has proven clinical effectiveness. However, treatment of the underlying disease that caused the hemorrhage, for example diabetes mellitus, must be carried out and, if necessary, corrected. However, Aspirin and other forms of anticoagulants that the patient was taking before the hemorrhage do not worsen the condition and can be continued after the episode of vitreous hemorrhage.
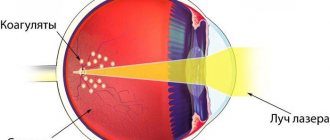
3 . Laser coagulation of the retina . Laser photocoagulation of the retina is the standard treatment for the treatment of vitreous hemorrhage from abnormal new vessels. This treatment should be carried out as soon as it becomes possible to visualize the retina, since panretinal laser photocoagulation not only promotes regression of neovascularization, but also helps reduce the risk of rebleeding.
| Hemorrhage into the vitreous body. Treatment | |
4 . Antivasoproliferative therapy . Intravitreal administration of angiogenesis inhibitors can reduce areas of retinal ischemia due to regression of newly formed vessels. In rare cases, the use of antivasoproliferative drugs is used in isolation. Typically, angiogenesis inhibitors are used in the combination treatment of vitreous hemorrhage, in addition to other treatments such as laser photocoagulation and vitrectomy.
| Antivasoproliferative therapy in the treatment of hemorrhage |
Localization of hemorrhage and its symptoms
Usually, apart from severe local redness of the orbit, there are no other symptoms. Rarely, when a large vessel is damaged, pain appears. With extensive hemorrhage, a feeling of pressure appears. The area of the outpouring itself is bright red in color and has clear boundaries. With extensive effusions, the blood spreads to the entire tunica albuginea.
There are several types of damage to small blood vessels, each with specific symptoms. Depending on the location of the damaged vessel, the following are distinguished:
- Hyphema is an accumulation of blood in the anterior chamber of the membrane between the cornea and iris. Typically results from blunt trauma. Accompanied by severe pain and blurred vision.
It looks like a homogeneous red formation with smooth contours. Blood can spread throughout the entire cavity of the anterior chamber if the person is in a horizontal position, or settle if the person is in a vertical position.
With this type of intraocular hemorrhage, vision is not distorted, except in cases where the hyphema completely covers the pupil. Blood clots with hemorrhage into the anterior chamber resolve quickly, literally within a few days.
- Hemophthalmos is a hemorrhage that occurs inside the vitreous body. Usually appears as a result of damage to the vascular membranes. It looks like a brown formation located immediately behind the lens. This is a severe damage to the eyeball.
There are two types of hemophthalmos: complete - leading to loss of vision; partial – capable of causing significant loss of visual acuity as a result of complications. The main symptoms of hemorrhage in the vitreous area are flashes of light before the eyes, dark moving spots that bother a person, as well as pronounced fog in front of the eye.
- Subconjunctival hemorrhage. The vessels of the mucous membrane are damaged. They are spontaneous, developing without an obvious reason. Outwardly it looks like a purple spot on the eyeball that does not disappear for several days. This is the only symptom of the disease. Deterioration of vision, pain are not observed.
They usually occur as a result of contusion of the apple orbit. Sometimes pathology occurs due to blood diseases and vasculitis. The symptom is pronounced bulging eyes with a sharp forward displacement of the eyeball, which severely limits ocular motor function. There is also hemorrhage under the skin of the eyelids and conjunctiva, and decreased visual acuity.
- Retinal hemorrhage. Develops as a result of bleeding from the vessels of the retina. The retinal tissue is very sensitive and thin. Therefore, even minor damage to blood vessels can lead to significant vision loss and the development of retinopathy.
Externally, the pathology is almost invisible, regardless of the extent to which the retinal tissue is involved. A person usually complains about the lack of sharpness of objects, objects in front of the eyes, a grid that shifts when moving in orbits, as well as the appearance of floating spots. Extensive blood clots in the retina can lead to complete loss of vision.
Symptoms of bleeding
It would seem that blood in the eye is manifested by the appearance of a red spot on the sclera, what is difficult in diagnosis? But for a doctor, the localization of bleeding can indicate the severity of the disease, the reasons that caused it, and methods of preliminary treatment.
Thus, hemorrhage in the anterior chamber of the eye is called hyphema. This is a red spot with clearly outlined edges. If the blood does not cover the pupil, but flows into the lower part of the eye, then vision retains its sharpness. This pathology does not require special treatment; the blood resolves on its own within a few days.
But if a person is elderly and in poor health, then he may develop glaucoma or cataracts, in which case treatment is necessary. Then the patient is prohibited from taking anticoagulants and non-steroidal anti-inflammatory drugs.
Fundus of the eye with hemorrhage
If there is blood in the vitreous body of the eye, then this is hemophthalmos. It looks like a large brown formation, and vision is impaired. In this pathology, blood enters the eye from the vessels of the membrane. If competent and urgent surgery is not performed to remove blood from the eye, the person may go blind forever.
When hemorrhage occurs in the retina, it is not visually manifested in any way, but the patient begins to see very poorly: objects are shrouded in fog, light spots and spots appear before the eyes. If such a patient is not provided with timely assistance, vision may be lost forever.
With severe contusion or vasculitis, bleeding into the orbit is possible. At the same time, the eye swells and visually increases in size. This is the most common sign of a basal skull fracture: both eyes swell, lose their mobility and lean forward. In this case, the blood accumulates around the eye in certain rings, reminiscent of glasses.
If this happens, it means that the injury was inflicted 24 hours ago, which is exactly how long it takes for blood to accumulate in and around the eye sockets until it becomes visible. Treatment in this case must begin immediately, otherwise the patient may lose vision.
Diagnostic methods
Even if there are no visible signs of eye damage after injury, the patient is recommended to undergo a preventive examination.
To determine the causes of hemorrhages in the anterior chamber and the nature of the damage, a number of studies are carried out:
- Visual examination and collection of medical history data allow us to draw a conclusion about possible etiological factors and determine the direction of further diagnosis;
- Visometry and tonometry are traditional methods that allow you to assess the functionality of the eyes and determine one of the main indicators of their health (IOP);
- Biomicroscopy is a method of examining internal structures using a slit lamp. Allows you to assess the extent and nature of damage;
- Computed tomography – examination is carried out in the most severe cases;
- Ultrasound of the eyeball - allows you to identify damage in areas that are inaccessible for examination by other methods;
- Blood test to determine the degree of clotting.
When identifying causes of non-traumatic origin, the diseases that served as the impetus for the development of hyphema are diagnosed.
Hyphema
Bleeding in the anterior chamber of the eye involves the gap between the cornea and iris. In normal condition, this area is filled with a transparent liquid, without foreign impurities.
The main source of hemorrhage is damage to the integrity of the blood vessel. Experts identify three possible causes of the disease.
Traumatization is one of the frequently recorded primary sources of hyphema formation. Prerequisites are further subdivided:
- Penetrating type - under the influence of sharp or blunt objects. Damage provokes a direct connection between the internal structures of the eyeball and the surrounding space;
- Non-penetrating – the internal structures of the eyeball are destroyed, which causes bleeding in the anterior chamber of the eye. Traumatization is the result of the influence of blunt objects, and there is no violation of the integrity of the outer shells;
- In the operating room - any type of surgical interventions on the organs of vision are considered injuries that can provoke the formation of hyphema.
Neovascularization is an eye disease accompanied by the formation of defective blood lines inside the organ. Fresh capillaries are characterized by structural defects and increased fragility, which leads to frequent hemorrhages with minimal or no external influences. The main prerequisites for the abnormal condition are presented:
- Diabetic angiopathy – as a consequence of diabetes mellitus;
- Overlapping of the lumens of the venous pathways in the retina;
- Retinal detachment;
- Neoplasms located inside the organs of vision;
- Inflammatory reactions occurring in the internal structures of the eyes.
Certain diseases of the body can also provoke hemorrhage in the scleral area. The problem may be caused by:
- Stable poisoning of alcoholic or drug origin;
- Problems with normal blood clotting;
- Malignant processes;
- System-wide lesions of connective tissues.
Causes of hemorrhages in the eye: from injuries to diseases
The most common cause of bleeding is injury to the visual organs. The cause of damage can be a blow to the eye, a blow to the head, torso injuries, or injuries to the sternum. Even minor bruises can lead to severe tissue changes.
But this does not always happen with injuries; often this phenomenon is provoked by diseases of internal organs and systems.
This condition can manifest itself due to destruction of the vascular wall, circulatory disorders: with damage to the vascular walls by atherosclerotic plaques, with microaneurysms, narrowing of the vascular walls; with the onset of pathological fragility of blood vessels or as a result of an increase in their permeability.
Excessive physical activity sometimes leads to intraocular hemorrhage.
The cause can even be a cough or a strong cry.
Atherosclerosis and increased blood pressure can cause narrowing of the lumen of the arteries and retinal angiopathy, causing fragility of blood vessels.
Diabetes mellitus is one of the causes of hemorrhage in the eye. It is capable of causing changes in retinal vessels. The vessel wall becomes weaker, microaneurysms appear on its surface, leading to intraocular bleeding.
The cause of the manifestation of pathology may be mechanical compression of the ocular vessels under the influence of a growing tumor inside the eye, as well as various inflammatory processes occurring in the iris, myopia.
Blood in the eye often occurs during increased cardio loads, as well as during labor in laboring women.
Correct and timely determination of the cause of the phenomenon makes it possible to preserve human health. When the first obvious symptoms appear, you should immediately contact a specialist.
Reasons why a blood vessel burst in the eye
The conjunctiva of the eyeballs contains many small capillaries that are quite fragile. When pressure increases from inside or outside the eyes, they can rupture. In such a hemorrhage, blood accumulates between the outer membranes, forming a bright red hematoma (hypophagma) . The reasons for its appearance differ in adults and children.
In a newborn
The provoking factor may be birth trauma, suffocation due to entanglement of the umbilical cord, as well as congenital diseases:
- deficiency of coagulation factors (absence or insufficient concentration in the blood);
- quantitative or qualitative changes in platelets;
- disruption of vascular formation;
- hypovitaminosis of vitamins P and C.
We recommend reading the article about retinal angiopathy. From it you will learn about pathology and its varieties, causes and dangers, signs and symptoms of angiopathy, methods of diagnosis and treatment. And here is more information about vascular injury.
The child has
In childhood, hyposphagma is often caused by infection, especially influenza, enteroviruses, Coxsackie virus, and whooping cough . It can occur with severe vomiting, coughing, straining and constipation. In adolescents, factors that cause injury to the blood vessels of the eye include prolonged visual stress when working with a computer, diving or scuba diving.
In an adult
The causes of burst blood vessels in the eyes of an adult cannot always be determined. Such hemorrhages are spontaneous, and elderly patients with age-related capillary fragility are especially prone to them .
Factors that provoke hyposphagma include:
- high intraocular pressure;
- hypertonic disease;
- increased thyroid function;
- eye injury, foreign body, intense friction with itching;
- anemia;
- decreased blood clotting activity, including during anticoagulant therapy and aspirin use;
- traumatic brain injury, contusion of the eyeball;
- excessive physical exertion, heavy lifting, sports;
- childbirth;
- diabetes;
- administration of medications under the eye, operations (including laser therapy), diagnostic procedures in ophthalmology;
- conjunctivitis, keratitis.
Watch the video why blood vessels burst in the eyes:
Diagnostics
If specific symptoms are detected, you should contact an ophthalmologist as soon as possible. The specialist will examine the eye using a slit lamp and an ophthalmoscope. To diagnose hyphema, it is extremely important for the doctor to know about the events preceding the hemorrhage (trauma, surgery, etc.)
The slit lamp can detect even minimal damage to the eye
In addition, the doctor will definitely measure intraocular pressure and check visual acuity, and also prescribe a blood clotting test.
Treatment is the work of the doctor, not the victim
Various causes of hemorrhage, its location and severity, adverse consequences, the worst of which is loss of vision, indicate that urgent consultation with a specialist is necessary.
It is rapid diagnosis and timely prescription of therapy that are the first aid for the disease. The basis for eliminating the consequences of pathology is rest and performing procedures. It is recommended to isolate the eye from environmental influences using an aseptic bandage.
The main diagnostic method is ophthalmoscopy - examination of the fundus. If hemorrhage occurs in the orbit, additional diagnostic measures are carried out - MRI, CT, x-ray of the skull, which makes it possible to judge possible complications.
The disease is treated using medications, surgery and vitamins. So, ophthalmologists prescribe the following measures:
- administration of vitamins intramuscularly;
- oral intake of vitamins: calcium chloride solution and ascorutin;
- intravenous administration of lidazo and glucose, which help to resolve infiltrates and blood effusions in the visual organs;
- introduction of protease enzymes.
Surgical intervention: vitrectomy surgery, laser correction is performed for damage to the vitreous body or retina. Used for extensive bleeding. It involves removing thickened blood from the eye cavity. Cloudy areas of the vitreous body and areas of the posterior hyaloid membrane are also removed.
To ensure rapid resorption of blood, special medications are prescribed to the patient.
- Hyphema. No specific treatment is required. The doctor prescribes drops of potassium iodide 3% externally 3 times daily for a week. The persistence of hyphema for more than 10 days, especially in elderly patients, is an indication for surgical removal of blood clots, since it indicates the development of future serious complications: glaucoma, uveitis, cataracts.
If an illness occurs, it is recommended to avoid taking anti-inflammatory non-steroidal drugs NSAIDs in any form, anticoagulants, as they interfere with blood clotting.
For the treatment of hyphema, albucid, taufon, and emoxipin are prescribed. Vitamin therapy is important. The use of vitamin P and ascorbic acid is beneficial. To strengthen the vascular wall, the drug ascorutin, which includes both of these vitamins, can be prescribed. It is recommended to consume vitamin C, which increases the elasticity of vascular walls.
- Hemophthalmos. When hemophthalmos occurs, you should immediately seek help from medical institutions, since this is a serious disease. Only urgent medical attention will help the patient preserve his vision. If there is bleeding into the retinal tissue, the patient is advised to rest completely.
For treatment, the doctor prescribes drugs to the patient that strengthen blood vessels and hemostatic agents. If the retinal effusion is extensive, the patient requires urgent hospitalization.
If, after the blood leaves the vessels, the hematoma appears in the form of glasses, which indicates that the eyelids are filled with blood, the patient needs to be hospitalized. Such a hematoma indicates damage to the base of the skull. To prevent the development of such effusions, experts recommend taking vitamin C, which softens the walls of blood vessels and makes them elastic.
Treatment of hemorrhage
Pathology is considered a dangerous process that can cause a number of serious consequences, so timely therapy is required. Treatment of hemorrhage depends on the degree of development of the disease. Severe form requires immediate surgical intervention. Even after surgery, it is not always possible to restore full vision. If the blood mass has led to tissue degeneration, removal is required to prevent the process from spreading.
In such cases, vitrectomy is prescribed - this is an operation to remove the leading components of the eye. During the procedure, the damaged vitreous body or parts thereof are removed. Then cleaning is carried out; blood clots must be pulled out from the inner cavity of the eye to protect against internal inflammatory process. After the operation, the patient remains under observation for another 2-3 weeks.
It is useful for the patient to stay with his eyes closed.
Moderate and mild degrees of the disease do not require surgical intervention. In this case, drug therapy is prescribed to allow the signs of hemorrhage to resolve on their own. During therapy, it is very important to reduce eye strain as much as possible; for this you should wear glasses, do not read, and do not work near monitors. It is best to keep your eyes closed for a long time. The therapeutic regimen includes the following components:
- thrombolytics with a hemostatic effect;
- drugs to strengthen blood vessels;
- corticosteroids in the form of drops;
- antioxidants;
- vitamin complexes.
Ways to combat retinal hemorrhage
If there is excessive bleeding, surgery (vitrectomy) may be performed. During surgery, the affected areas of the vitreous body and blood clots are removed. In most cases, vision recovery occurs in the first 2-4 weeks after surgery. If there are irreversible changes in the structure of the retina, vision may still remain insufficiently clear.
In case of minor hemorrhage, not caused by chronic diseases, it is recommended to provide rest to the eyes. You can sit for a while with your eyes closed. This will normalize blood circulation.
For hemorrhage in the retina of the eye, medications that have a hemostatic and vascular strengthening effect can be used. Such drugs include “Emoxipin”. This medication is recommended to be used under the supervision of a physician.
In some cases, the use of products containing vitamins K and E is indicated. These products have a beneficial effect on the walls of blood vessels and help improve blood clotting.
If there is retinal hemorrhage, the following medications may also be used:
- Corticosteroids;
- Medicines with anti-inflammatory properties;
- Medicines belonging to the group of diuretics;
- Vitamin and mineral preparations rich in antioxidants.
In some situations, in the presence of retinal hemorrhage, calcium therapy is performed. The procedure promotes blood resorption, helps relieve tissue swelling, and reduces inflammation.
Treatment with folk remedies
Together with traditional medicine, traditional medicine is used to treat pathology, helping to speed up the healing process. Traditional medicine only helps relieve symptoms; however, they will not be effective in severe cases of hemorrhage. For these purposes, recipes are used to help relieve symptoms and alleviate the condition.
Thus, chamomile decoction, boiled and crushed cabbage leaves and aloe juice are used for compresses. To relieve symptoms, lotions are also made from saffron, radish peel, fresh cheese and lentil oil. The duration of the procedure is 5 minutes.
Remember! Traditional medicine is powerless in severe cases of the disease. Frequent hemorrhages with extensive damage to the tissues of the eyeball, especially if it is associated with a head injury, are a serious reason to contact a specialist: a therapist, an ophthalmologist.
Hemophthalmos
Spontaneous hemorrhage into the vitreous body reduces its standard transparency index. Its responsibility is to conduct a light pulse from the cornea to the retina. The source of the problem is the following indicators:
- Damage to the retina, capillary lines in diabetes mellitus;
- Thrombosis of small capillaries of the retina;
- Atherosclerotic damage to the veins and arteries of the organs of vision;
- Pathologies of veins and arteries of congenital etiology - microscopic aneurysms;
- Lesions of the body of the eyeball with ruptures of individual membranes;
- Trauma with preservation of the integrity of the outer covers of the eyes;
- Increased level of intracranial pressure – with neoplasms, traumatic brain injuries, hemorrhages in parts of the brain;
- A gradual increase in intrathoracic pressure - with coughing, heavy physical exertion, sneezing, gag reflex, during childbirth;
- Blood diseases - anemic abnormalities, hemophilia, malignant processes in the bloodstream, the use of medications to reduce the rate of clotting;
- Tumor-like processes in the internal tissues of the eyeball;
- Autoimmune diseases;
- Retinal detachment;
- Congenital pathologies.
A severe degree of myopia can contribute to the formation of hemophthalmos.
Complications after hemorrhage
Regardless of which area of the eyeball the bleeding occurs, the pathology has a visual defect. Many patients delay visiting a doctor. Due to untimely treatment, the disease progresses rapidly, so the following complications appear:
- glaucoma;
- retinal detachment;
- disturbance of image perception;
- loss of vision (partially or completely);
- traumatic cataract;
- formation of a cataract.
These consequences are due to the toxic effects of elements formed as a result of the destruction of blood cells. To eliminate complications, radical measures are often resorted to.
Prevention is as simple as two
There are no specific measures to prevent the development of bleeding into the eye. Preventive measures are different, they all boil down to strengthening the immune system in general, since the condition of blood vessels and various diseases, such as hypertension or diabetes, are the consequences of an unhealthy lifestyle.
A healthy lifestyle and taking vitamins are excellent disease prevention.
Treatment of the underlying disease can prevent the development of complications in the form of bleeding.
Types and classification of eye hemorrhages
The classification of the disease depends on the location of blood clots in the organs of vision. In addition, the pathological phenomenon is divided based on the intensity of development:
| Severity | Main characteristics |
| Lightweight | There are no painful sensations. The structure of the organ does not change and is restored over time. |
| Average | Minor eye damage. Needs drug therapy. |
| Heavy | Serious and sometimes irreversible impairments, including loss of vision. Treatment is carried out through surgery. |