Bacterial conjunctivitis is one of three types of damage to the ocular conjunctiva by pathogenic microflora. If in the case of the viral type the root cause is considered to be damage to the eye by viruses, in case of allergic conjunctivitis the cause should be sought from an allergist, while bacterial damage to the eye is caused by the ingress of microbes that multiply quickly and cause severe discomfort to adults and children. How to distinguish bacterial conjunctivitis from other types of disease? Is there a difference in treatment? What conditions are favorable for damage to the conjunctiva of the eye by various bacterial agents? Is it possible to avoid complications if there is purulent discharge from the eyes? Details in the article.
Physiology of the human eye
Nature has provided protective mechanisms for the body to eliminate negative consequences from contact with the environment. The eyes are no exception, given that they can be easily injured. In addition to the eyelids and eyelashes, the eyeball is constantly moistened by a liquid called lacrimal and has the function of protecting against the penetration of the smallest elements (grains of sand, microbes, viruses) onto the cornea. This is a special function of local immunity.
Tear fluid is formed in the lacrimal sacs and enters the surface of the eyeball through the canaliculi in a small or large volume, which depends on external circumstances.
This liquid itself is not ordinary water. It contains special substances - immunoglobulin and lactoferrin, which act as antiseptics and a protective barrier against microbes of different origins. But circumstances arise that reduce the protective properties of tear fluid. Microbes, viruses and allergens quietly penetrate the mucous membrane of the eyes and begin to actively multiply, leading to the formation of inflammation and pus.
With conjunctivitis, it is the conjunctiva of the eye that is affected, the lacrimal canal is blocked and the natural antiseptic cannot fulfill its function in full. Pathogenic microflora, which surrounds a person at every step, freely settles on the conjunctiva and leads to serious illness.
Viral conjunctivitis
More than half of all cases of inflammatory diseases of the conjunctiva belong to this type of conjunctivitis. To date, more than 500 different viruses have been identified that can cause certain types of conjunctivitis in children. The most common pathogens are:
- Adenoviruses, which can cause adenoviral conjunctivitis or more severe epidemic keratoconjunctivitis (pharyngoconjunctival fever). The disease is transmitted by airborne droplets and affects children between 5 and 10 years old. Manifestations of eye conjunctivitis in children most often occur against the background of pharyngitis, rhinitis, tracheitis, bronchitis, and sometimes otitis, with an increase in temperature to 38–39°. This is not only hyperemia and mucous discharge, but also the appearance of pinpoint hemorrhages and small follicles in the area of the lower transitional fold.
- Enterovirus-70 causes epidemic hemorrhagic conjunctivitis. The disease is manifested by swelling of the eyelids and chemosis, the appearance of mucopurulent discharge, swelling of the conjunctiva, noticeable hemorrhages, allowing the doctor to determine this type of conjunctivitis in a child. An additional symptom is the presence of small white or yellowish spots.
- Herpes simplex viruses lead to various types of herpetic conjunctivitis: catarrhal, follicular, vesicular-ulcerative. In this case, characteristic bubbles appear on the mucous membrane of the eyelids, which subsequently turn into erosions or ulcers.
Specifics of the bacterial form of conjunctivitis
This form of damage to the visual organ is the most complex and dangerous among the three forms of pathology, because there is a bacterial background that can quickly multiply and leave waste products on the mucous membrane. Bacterial conjunctivitis is always accompanied by the formation of pus in a small or large volume. A purulent mass fills the conjunctiva, comes out, and can stick together the eyelashes, making it difficult to open the eyes and see clearly.
Bacterial conjunctivitis in most cases affects both eyes at the same time, or very little time passes between inflammation in one and the other if treatment measures are not carried out in a timely manner.
The incubation period is 1–2 days from the moment any bacteria penetrates the conjunctiva. The ways of infection with bacterial conjunctivitis are very diverse, from dirty hands and the use of other people's objects, for example, decorative cosmetics, towels, to complications after any disease.
Bacterial conjunctivitis is a form of complications after inflammation in the throat, nose, and ears, if these diseases become chronic or are not treated properly. Staphylococcus, pneumococcus, Pseudomonas aeruginosa, Escherichia coli, chlamydia and other classes of bacteria that cause ENT diseases can enter the conjunctiva and, due to reduced immunity, manifest themselves as purulent secretions.
Eye infection with bacterial conjunctivitis is relevant for newborns if the mother has one of the groups of bacteria in the birth canal, for example, chlamydia, staphylococcus. When passing through these paths, without having a protective film, as in the uterine cavity, the child gets an infection of the eyes, which manifests itself in the first days after birth.
If purulent discharge is not treated according to the correct regimen or therapy is not carried out until complete recovery, conjunctivitis becomes chronic, which can negatively affect vision if pathogenic agents penetrate the cornea.
The essence of bacterial pathology
The term “conjunctivitis” refers to a certain type of inflammatory reaction that affects the mucous membrane of the organ of vision. The conjunctiva covers the anterior zone of the eyeball with a transition to the inner surface of the eyelids. The appearance of conjunctivitis is provoked by various types of pathogenic microorganisms that populate the mucous membrane of the eye from the very birth of a person.
The patient is able to detect signs of conjunctival damage on his own, but to clarify the correct diagnosis for prescribing treatment should be entrusted to a specialist. To prevent infection of the second eye and immediate environment, you must adhere to the following recommendations:
- use only your own hygiene items;
- avoid touching your eyes with your hands;
- minimize contact with healthy people.
The main reason for the development of bacterial conjunctivitis is associated with a weakening of local immunity, which leads to an imbalance between friendly and pathogenic microflora.
Causes of infection
In addition to a decrease in the body's defenses, a rapid increase in the pathogen population can be triggered by the following situations:
- frequent colds and viral diseases;
- foreign bodies getting on the surface of the conjunctiva;
- diseases of the ENT organs, infectious diseases of the skin;
- pathologies of the visual organs, structural defects or injuries;
- improper use of contact lenses;
- impaired outflow of tear fluid, dry eye syndrome.
Bacterial conjunctivitis is highly contagious, and infection can occur through household contact. Conjunctivitis is diagnosed even in newborns who become infected in utero from a sick mother. In adults, acute bacterial conjunctivitis is provoked by non-compliance with the rules for using contact lenses.
Signs
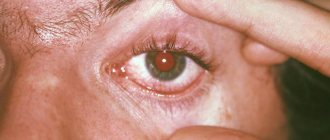
Symptoms of conjunctivitis develop rapidly. The inflammatory process first starts unilaterally, rapid progress leads to damage to both eyes. Just a few hours after direct infection, bacterial conjunctivitis signals a violent clinical picture:
- copious discharge of purulent exudate from the eyes with swelling of the eyelids and mucous membranes of the eye;
- sticking of the eyelids due to the appearance of crusts that prevent the opening of the organ;
- hyperemia of the conjunctiva with profuse hemorrhages;
- burning sensations, severe pain, sand in the eyes.
The acute form of the pathology can be accompanied by a sharp jump in body temperature, the appearance of headaches, the development of insomnia, and the formation of follicles on the mucous membrane of the eye. If at the initial stage of the disease the discharge from the eyes is watery, then after a day it becomes purulent, and the mucus looks like threads. The danger of this form of ophthalmia is the threat of developing keratitis of bacterial etiology.
Acute conjunctivitis should be treated immediately if even minor symptoms are detected. Therapy usually lasts 10-14 days, but self-medication is excluded.
Factors preceding bacterial conjunctivitis
The human body is naturally able to withstand any external circumstances and quickly recover if there is no reason that reduces internal vigilance and protection. Any pathological processes that lead to a failure in a single mechanism open a weak link for attack by pathogenic agents from the outside.
The eyes, unlike other organs, are the first to be exposed to this threat. Their protection, even with a good immune response, can be destroyed if the influence of the outside world is overly aggressive, for example, damage to the eyes from toxic gas, caustic smoke, or some object. With bacterial conjunctivitis, infection occurs for the following reasons:
- Frequent respiratory diseases (sinusitis, otitis media, tonsillitis, ARVI) are a source of bacteria that easily penetrate the eyes due to their close location to the source of inflammation. Without following the rules of hygiene, an adult or child transfers germs from the nose to the eyes or the infection penetrates through adjacent channels;
- Injury to the conjunctiva by an object or gas, which weakens the function of the protective film and allows bacteria to freely penetrate the damaged organ;
- Other eye diseases not associated with bacterial conjunctivitis provide fertile ground for bacteria. Dry eye syndrome, when there is not enough tear fluid to create a protective film. Blepharitis, cataracts, viral conjunctivitis and other pathological processes lead to weakened immunity in the organs of vision;
- Mother's illnesses that are not cured before pregnancy pose a threat to the newborn becoming infected during childbirth;
- Hypothermia also weakens the body’s defenses and creates conditions for bacterial conjunctivitis;
- Dermatitis on the face is a breeding ground for bacteria if the rules of hygiene and care for inflamed areas on the skin are not followed;
- Glasses and contacts can be a source of bacteria if proper use of eye instruments is not followed. Lenses must be removed and treated in a special solution, but glasses also require proper use. You should not use other people's items, because both lenses and glasses are individual products.
Any of the above reasons can lead to bacterial conjunctivitis, because pathogenic agents surround a person constantly and wait for the right moment to attack.
This eye disease is contagious, which creates a threat to your immediate environment if simple hygiene rules are neglected.
What causes conjunctivitis?
As an immunological protection for the eyes, it produces tear fluid, which contains immunoglobulin and lactoferrin (eliminate all pathogenic microbes that enter the eye). Despite this, it is possible that the immune function may be weakened due to which the barrier protection does not work and the person begins to suffer from conjunctivitis.
The main pathogens that cause conjunctivitis are streptococci, chlamydia, staphylococci, gonococci and others. Treatment becomes more complicated when bacterial conjunctivitis is supported by a fungal infection. The following factors predispose you to contracting conjunctivitis:
- Decreased protective functions of the immune system.
- Contact with the membrane of any foreign body, which leads to infection.
- Damage to the eye shell.
- Infectious diseases of the skin.
- ENT diseases.
- Some eye diseases.
- Consequences of wearing contact lenses for a long period of time.
Signs of bacterial conjunctivitis
But, basically, infection occurs through direct contact with conjunctival secretions. If we talk about infection of newborns, then in almost 30% of children conjunctival damage occurs. This is explained by the infected birth canal through which the child passes if the mother has chlamydial or gonococcal infection.
Transmission routes
The bacterial form of conjunctivitis, along with the viral form, has a high level of contagiousness, and therefore is very common in medical practice. Infection occurs through the use of household items, such as towels, bed linen and dishes. Therefore, it is very important, if there is a patient with bacterial conjunctivitis in the family, to provide him with separate items for personal hygiene.
Manifestations of bacterial conjunctivitis
Based on the fact that ordinary people rarely know about the existence of several types of conjunctivitis, it is difficult to understand from the expressed symptoms that it is bacterial that has developed. But if you observe the clinical picture on the first day of infection, you will notice the following signs indicating the penetration of bacteria into the eyes:
- The inflammatory process is rapid. No more than 48 hours pass from infection to the onset of symptoms;
- The patient feels a burning sensation, pain, and the presence of a foreign object. Typically, complaints describe sand in the eyes and itching;
- Swelling, redness, hemorrhages, discharge of purulent fluid. This secretion can accumulate in the corners of the eyes closer to the nose or completely fill the space of the conjunctiva, form dried crusts on the edges of the upper and lower eyelids, and glue eyelashes together. In a complex form of the disease, there is so much pus that the eyes open with difficulty and the conjunctiva between the eyelids may be pinched;
- Possible increase in body temperature, headache, general malaise, as with other forms of infection of the body by pathogenic bacteria or viruses;
- The bacterial form is confirmed by souring of the organs of vision after waking up, which indicates the activity of microbes. With viral and allergic conjunctivitis, such symptoms are absent, because the secretion does not have a sticky base.
You can independently understand that the eye is affected by bacteria and not a virus or that it is an allergic reaction if this is not the first time you have encountered the disease. But you shouldn’t take risks and start treatment without consulting an ophthalmologist, because the principles of treating bacterial, viral or allergic conjunctivitis differ from each other, and incorrect actions can lead to complications and a longer course of the disease.
What are the symptoms of chlamydial conjunctivitis?
This type of conjunctivitis resembles a bacterial infection in its course. But chlamydia is not a bacterium. It occupies an intermediate position between viruses and microbes. Chlamydial infection occurs in acute, subacute or chronic form. In the first case, its symptoms are pronounced. Itching and burning appear, pus is released from the conjunctival sac. Subacute conjunctivitis caused by chlamydia is characterized by more mild symptoms. Chronic inflammation is sluggish, with slight redness of the conjunctiva, mild lacrimation and almost complete absence of discharge. This disease is accompanied by blepharitis, an inflammatory lesion of the edges of the eyelids.
Chlamydia is transmitted to humans when visiting a bathhouse or swimming pool, as well as through sexual contact. Inflammation develops in one eye, but often it becomes bilateral. Difficulties may arise in treating this disease. Not all antibacterial drops are capable of destroying this type of parasite. I have to take antibiotics. We will talk about methods of treating various types of conjunctivitis later.
Fighting bacteria
Treatment of bacterial conjunctivitis, if correctly diagnosed by an ophthalmologist, takes 10–14 days, depending on the severity of the disease. The principles of therapy for adults and children are the same. The only exception is the choice of medications prescribed by the doctor according to the patient’s age.
To understand how to treat bacterial conjunctivitis in an adult or child, the doctor conducts an examination, examination using equipment and prescribes tests to confirm his assumptions. Laboratory studies of purulent secretion make it possible to determine the type of pathogenic agent in order to select the correct antibiotic in drops, given that different eye drops are highly effective against specific types of pathogens. In order not to select an antibiotic at random, it is better to identify the causative agent of conjunctivitis.
- Sometimes the selection of an antibiotic for the treatment of an eye disease is complicated by the patient’s allergic reaction to the active substance or additional ingredients of the drug. If the patient is not aware of a possible allergic reaction, the new medicine must be taken with caution to prevent the development of adverse symptoms;
- In addition to antibiotics in the form of eye drops, the doctor prescribes disinfection procedures using a furatsilin solution, which is prepared at home and used in both adults and young patients;
- To eliminate itching and swelling, antihistamines are prescribed in the form of tablets or drops for babies;
- At night, to eliminate the need for eye drops, antibiotic eye ointment is used at a certain interval. The action is long-lasting, which eliminates the possibility of protein synthesis of pathogenic agents;
- In more complex cases, it is possible to prescribe an eye wash procedure in a hospital setting to remove as much germs as possible.
Attention! Any eye patches with medicine or disinfectant solution are excluded so as not to create favorable conditions for the growth of bacteria and aggravation of the patient’s condition.
How to treat a bacterial infection
The leading role in therapeutic measures belongs to local antibiotics (drops, ointments) of a bactericidal nature. To block the contagiousness of the disease, precautions should be taken, not forgetting the principles of personal hygiene.
Treatment regimen:
- At night, an antimicrobial ointment is placed under the eyelids;
- in the morning, sour eyes are cleaned of purulent mucus with an antiseptic;
- During the day, antibiotic drops are instilled every 2-4 hours.
The most modern method of treating bacterial conjunctivitis is the use of fluoroquinolone antibiotics. The highest effectiveness can be achieved with therapy with solutions of Ciprofloxacin, as well as Ofloxacin.
The combination drug Sofradex, which combines antibiotics with an anti-inflammatory agent, has gained well-deserved popularity. Among ointments, Tetracycline ointment has the best antibacterial effect.
Drops for bacterial conjunctivitis
| Names of ophthalmic solution | Brief information about the drip form of medication with an antibiotic |
| Tobrex | The active substance tobramycin is characterized by a wide range of effects on the vital activity of many bacteria, including streptococci and staphylococci, diphtheria bacillus. The course of therapy lasts a week |
| Dancil | Drops based on ofloxacin (fluoroquinolone) demonstrate the strongest antimicrobial effect. Due to resistance to the composition of enzymes secreted by bacteria, antibiotic resistance does not develop |
| Levomycetin | The active substance of the drops is characterized by rapid absorption and blocks the synthesis of bacterial protein structures. Inexpensive drops should not be used for a long time, so as not to cause disruption of the hematopoietic function |
| Phloxal | A solution of a popular antibiotic from the fluoroquinolone group is effective 10 minutes after use. The therapeutic effect of drops, practically devoid of harmful effects, lasts up to 6 hours |
| Oftaquix | The active antibacterial substance levofloxacin can lead to the development of an allergic reaction. Drops have a list of side effects |
| Albucid | The drug from the sulfonamide line is characterized by a powerful bacteriostatic effect. The active substance helps suppress the growth and reproduction of bacteria, but without completely destroying them |
Eye drops for children
Any type of bacterial eye disease without a professional approach to treatment can lead to adverse consequences. For the treatment of bacterial conjunctivitis in children, the doctor selects medications approved for children and adjusts the dosage taking into account the child’s age and the severity of the eye infection.
How can you treat a child:
- Albucid eye drops 20% concentration;
- children over 2 years of age can have Levomycetin solution instilled into their eyes;
- Fucithalmic drops are used for a week, if there is no result, the drug is replaced with another;
- Children after one year of age are allowed Ciprofloxacin drops, starting with a loading dose every two hours;
- Vitabact drops are suitable for long-term treatment of symptoms of combined infection in newborns.
During treatment, one should not forget about the high contagiousness of bacterial conjunctivitis. If the organ of vision is affected in a small child, it is necessary to ensure that he does not rub his eyes with his hands, as this can worsen the course of the disease. An important point in the treatment of conjunctivitis in small and adult patients is washing the conjunctiva with antiseptics.
Sources used:
- Age-related macular degeneration / A.S. Alpatov. - M.: GEOTAR-Media, 2020.
- Ultrasound in ophthalmology / Diana Angelova. - M.: Palmarium Academic Publishing, 2012.
- Textbook of eye diseases / V.N. Arkhangelsky, M.K. Bryantseva, K.V. Dormidontova. - M.: State Publishing House of Medical Literature, 1983.
- National Eye Institute
Sequence of procedures in the treatment of bacterial conjunctivitis
The treatment regimen for the disease consists of several points, which are repeated daily until complete recovery:
- Disinfect each eye with furatsilin solution, preparing it in advance according to the instructions included in the package with the drug. You will need a sterile napkin, which you can buy at a pharmacy or make yourself from a bandage. A separate swab for each eye to prevent infection if only one is affected. The possibility of infection is very high if you neglect to use different tampons. The liquid should be warm and not burn the surface of the eyelid and the mucous membrane of the eye;
- After thoroughly cleaning both eyes, you need to instill drops prescribed by your doctor. Try not to let the tube dropper come into contact with the eye so that bacteria do not transfer to its surface and be transferred to the other eye. It is better to wipe the tip before performing manipulations on the second eye. The number of drops and approaches per day is determined by the attending physician;
- Before going to bed, the drops are replaced with eye ointment, which, after thoroughly disinfecting the hands and the inflamed area, is placed in a thin layer behind the lower eyelid and distributed over the surface. It is advisable to close your eyes and remain in this position until the morning so that the antibiotic has maximum effect on the disease.
You cannot stop treatment when the first improvements appear, because residual forms of the pathogenic agent may be present in the eyes and after some time the conjunctivitis will return and may develop into a chronic form, which is much more difficult and longer to combat. There is a risk of developing bacterial keratitis (damage to the cornea by microbes).
The ophthalmologist always schedules a follow-up appointment with the patient to make sure that the treatment is correct and there is no reason for relapse.
Treatment
How to treat conjunctivitis in adults? Bacterial conjunctivitis is usually treated by a qualified ophthalmologist. It is not recommended to treat bacterial conjunctivitis on your own, as if treated incorrectly, serious complications can subsequently arise.
To treat conjunctivitis, topical medications containing bactericidal antibiotics are used.
Typically, the following drugs are prescribed:
- Erythromycin ointment;
- Tetracycline ointment;
- Dexa gentamicin ointment;
- Gentamicin drops;
- Fluoroquinolones (Ofloxacin, Lomefloxacin, Ciprofloxacin).
Ophthalmologists often prescribe Moxifloxacin drops from the fluoroquinolone group if the cause of conjunctivitis is not gonococcal or chlamydial infection. This drug is used three times a day for 7-10 days. Also, a fairly popular drug is Trimethoprim/polymyxin B, which must be used 4 times a day. As a rule, if this drug does not help, this indicates that the patient has conjunctivitis of a viral or allergic nature or has bacterial resistance to this drug. In this case, bacterial culture is performed and sensitivity to antibiotics is tested.
Conjunctivitis caused by chlamydia is usually treated with tetracycline antibiotics. Also, chlamydia reacts to macrolides and fluoroquinolones. Chlamydia conjunctivitis should never be treated on its own. It can only be cured with properly selected medications, since chlamydia very often develops immunity to many antibiotics. The ophthalmologist prescribes treatment strictly individually for each patient.
It is imperative that the patient observe hygienic requirements for caring for the mucous membrane of the eyes.
Using cotton balls, the eyelids are regularly wiped. To disinfect the conjunctival sac and remove purulent discharge, jet rinsing with an antiseptic solution is performed. As a rule, furatsilin or boric acid is used for washing. An undine or pear is used as a tool for washing the eyes.
Read about conjunctivitis during pregnancy at the link.
Symptoms
Only after thorough washing of the eyelids and conjunctival sac are antibacterial eye drops instilled. The eyes are usually instilled with drops every 2-3 hours using a pipette. Antibacterial ointment is usually applied at night. The eye ointment is administered using a special eye stick.
In case of bacterial conjunctivitis, it is not recommended to apply a bandage to the sore eye, as this complicates the treatment of the inflammatory process and can contribute to infection of the cornea.
The full course of treatment for bacterial conjunctivitis is carried out within 10-12 days. During this period, all symptoms of the disease should completely disappear. It is advisable to carry out bacteriological control of the contents of the conjunctival sac again after this period.
Complications
As a rule, timely antibiotic therapy allows you to completely get rid of bacterial conjunctivitis. Without proper treatment, there is a risk of complications. Among them are:
- Bacterial keratitis. It is an infectious disease of the cornea of the eye.
- Clouding of the cornea of the eye.
- Decreased visual acuity.
- Ulcerative keratitis. Characterized by an inflammatory process in the cornea. Otherwise, this disease is called a corneal ulcer. Without treatment it leads to blindness.
- Orbital cellulitis. This is a serious, life-threatening disease that is characterized by inflammation of the eye tissue behind the orbital septum.
The article will tell you whether conjunctivitis is contagious in a child.
In addition, you need to know that if left untreated, the acute form of bacterial conjunctivitis can become chronic.
Prevention
Don’t forget, if you have allergies under your eyes, you should consult a doctor.
It is possible to avoid the occurrence of the disease by preventing conjunctivitis:
- It is necessary to strictly adhere to hygiene standards. Under no circumstances should you touch the eye area with dirty hands, as this is a direct route for infection and the occurrence of an inflammatory process.
- Those who use contact lenses must follow the rules of wearing lenses and hygiene. Before putting on and removing lenses, you should thoroughly wash your hands and regularly change lens storage containers.
- Avoid injury and damage to the eyes.
- Only personal hygiene products and bedding should be used.
- You should strengthen your immunity, especially in winter. To do this, you need to lead a healthy lifestyle, eat right, harden yourself, and take vitamin and mineral complexes.
What to do if your vision goes bad.
How to restore farsightedness at home: https://eyesdocs.ru/zabolevaniya/gipermetropiya/dalnozorkost-u-godovalyx-detej.html
Modern effective methods for treating clouding of the lens of the eye are given in this article.
Brief overview of drugs for the treatment of bacterial conjunctivitis
In most cases, a solution of furatsilin is prescribed as a disinfectant. It can be replaced with plain boiled water or a decoction of herbs, which must be carefully strained before use so that particles do not get into the eye and cause deterioration. Among traditional medicine recipes, baths with tea leaves are popular, in which tampons are moistened and the eyes are wiped from the temple to the nose.
Among antibiotic eye drops and ointments, the following drugs are widely used:
- Levomycetin;
- Albucid;
- Phloxal;
- Oftaquix;
- Tobrex;
- Sulfacyl Sodium (for children);
- Normax (for children);
- Tetracycline ointment;
- Erythromycin ointment.
The list of pharmaceuticals for the treatment of bacterial conjunctivitis is more diverse, but the choice should be made only together with your doctor and study the instructions for use in detail, especially the contraindications section, in order to avoid harm from the medicine.
What medications does a doctor prescribe for bacterial conjunctivitis?
Eye conjunctivitis - treatment with medications, complex therapy:
- Drinking plenty of fluids - in the first days of the disease, an increase in body temperature is possible, which is accompanied by dehydration, which contributes to the drying out of the mucous membranes and increases the soreness of the eyelids.
- The use of anesthetic eye drops is necessary so that the patient can painlessly apply medicinal ointments under the lower eyelid.
- Antibacterial agents: eye drops and ointments, antibiotics - with this eye treatment, the symptoms of the disease go away quite quickly.
- Rinsing the eyes several times a day with a solution of furatsilin - a disposable sponge is moistened in the solution and wiped the eyes from the outside to the inside.
How is conjunctivitis treated in adults? What conditions must be observed during therapy? Before instilling eye drops, you should always clean the eyelids of accumulated secretions - you can wash your eyes with herbal decoctions or by dissolving one furatsilin tablet in a cup of warm water. Since eye drops are stored in the refrigerator, before using them, the drops must be taken out in advance so that their temperature is close to room temperature. If you follow all the doctor’s instructions, the disease goes away quite quickly, within 5-7 days. During this time, inflammation decreases and pathogenic bacteria die.
Treatment for chronic conjunctivitis can last for weeks. It is difficult to treat because a weakened immune system cannot fight bacteria at full strength. In this case, you will need to take a culture of the discharge from the eyes to check the flora, determine sensitivity to antibiotics and be treated with drugs that can cope with bacteria. This is another significant proof that you should not rely only on decoctions and compresses when treating adults with folk remedies, because they are designed to relieve some of the symptoms, but will not be able to cure the disease.
Bacterial and viral conjunctivitis: what is the difference between the diseases?
Sometimes the bacterial form of the disease can be confused with a viral one, and then the treatment will be ineffective, which will lead to complications in the future. This happens because the symptoms of conjunctival lesions are very similar. Therefore, it is necessary to find out the exact root cause of the disease and only then begin treatment. To do this, you should visit an ophthalmologist and undergo all the necessary examinations.
Features
| Viral | Bacterial |
| Only one eye is affected | Initially, one eye is affected, then the infection spreads to the second |
| Among the first characteristic symptoms are redness of the eyeball and severe tearing. | Redness and tearing are practically not expressed. On the contrary, purulent discharge is clearly visible |
| Eyelashes stick together due to the secretion of mucus | Eyelashes stick together due to excessive discharge of pus |
| 80% of cases develop viral conjunctivitis, which, if not treated promptly, turns into a bacterial form | Infection occurs due to the contact of pathogenic bacteria on the membrane of the eye (chlamydia, staphylococcus) |