Classification
A unified classification of ischemic eye diseases has not currently been developed. In this case, there is a direct connection between the mechanism of development of ischemia and damage to various parts of the blood flow. In connection with this circumstance, we can say that ischemic eye diseases are of a polyetiological nature, have a variety of clinical manifestations, and also do not have a single pathogenesis.
The development of ischemia in the posterior segment of the eye is greatly influenced by the anatomical features of blood flow in the area of the optic nerve head and retina.
Conventionally, ocular ischemia can be divided into acute and chronic.
Symptoms and diagnosis
It is known that the retina covers most of the inner wall of the eye, consists of a number of zones with different functional purposes (for example, the foveal fovea in the macular “yellow spot”; the optic disc; the jagged edge devoid of photosensitive cells on the periphery) and has a multilayer structure. They include, in particular, the pigment epithelium, the ganglion layer, the outer and inner nuclear layers, etc. These layers and zones differ in the number and structure of photoreceptors, the concentration of light-sensitive pigments, and thickness - for example, the most sensitive to light and providing central vision, the foveal fossa is the thinnest zone and consists exclusively of cone cells.
It is obvious that with such a complex organization and narrow specialization of each structural element, full vision is possible only with complete coordination and normal functioning of all elements, and any disturbances in nutrition, oxygenation (oxygen supply) or, moreover, the integrity of the retina automatically become a serious ophthalmological problem that requires in immediate intensive treatment. Since the retina is the main and only receiver of the image focused by the eye optics (which must be transmitted to the optic nerve and then transmitted to the visual centers of the cerebral cortex), retinoschisis as a splitting of the receiving-transmitting tissue inevitably affects the quality of the final visual image built by the brain. Accordingly, the first and main complaint with retinoschisis is a significant deterioration in vision.
The localization of the dissection is of significant importance: dystrophic-degenerative retinoschisis, as indicated above, is more often manifested by disturbances or loss of peripheral visual fields (with probable subsequent spread to the central areas), while hereditary retinoschisis often affects the central visual field in the early stages.
With the increase in destructive changes, not only visual acuity often decreases, but also general light sensitivity: patients are increasingly less able to navigate in twilight or darkness. The progression of untreated retinoschisis leads to the most severe consequences for the eye, including retinal detachment and irreversible blindness - the risk of such an outcome accompanies almost any retinal pathology. A less common, but also quite likely complication of retinoschisis is hemophthalmos - extensive hemorrhage into the vitreous body.
To diagnose retinoschisis and differentiate it from other retinopathy, in addition to standard fundus ophthalmoscopy, visometry (precise measurement of visual acuity), perimetry (examination of visual fields), slit-lamp biomicroscopy, optical coherence tomography, electroretinography, etc. is used. A thorough study of anamnestic data is necessary. – in particular, the presence of background somatic or endocrine pathology (primarily diabetes mellitus, cardiovascular diseases, atherosclerosis), unilateral or symmetrical nature of the lesion, age of manifestation of the disease, dynamics of progression, etc. are taken into account. If hereditary retinoschisis is suspected, a medical genetic consultation is required.
Our ophthalmology center has all the capabilities to provide high-quality and inexpensive care to patients diagnosed with retinoschisis. Retina specialists (laser and vitreoretinal surgeons) carry out diagnostics and effective treatment using modern equipment. We approach each patient individually, which allows us to achieve the best possible treatment results.
Causes of acute ischemia
In acute ischemia of the posterior segment of the eye, problems occur with blood flow in the central retinal artery or central retinal vein. In addition, there is anterior or posterior ischemic neuropathy and acute toxic neuropathy. Acute ischemia can occur against the background of long-term chronic hypoxia of the eyeball (angioretinopathy of diabetic or hypertensive nature, degenerative processes in the retina, stenosis of the carotid or orbital artery, temporal arteritis).
Ocular ischemia is most often associated with vasospasm, head or eye trauma. Sometimes ischemic neuropathy and impaired blood flow in the central vessels of the retina are associated with hypotension that occurs while taking certain medications as a result of surgery. Risk factors for coronary eye disease are anemia, imbalance in the blood coagulation and anticoagulation systems, and microembolization.
Retinal ischemia: clinical picture of pathology and therapeutic methods
The level of visual acuity primarily depends on the functionality of the vascular system not only of the eye and retina. Various vascular pathologies can provoke the development of ischemic eye diseases, among which retinal ischemia is especially prominent. This pathology leads to sudden loss of vision and requires timely treatment.
Retinal ischemia: acute course
The following factors provoke the development of acute retinal ischemia:
- Disruption of blood flow in the central retinal vein.
- Pathological blood flow in the central retinal artery.
- Ischemic process in the eyeball.
It also appears against the background of diabetic or hypertensive angioretinopathy, degenerative lesions of the retina, stenosis of the carotid or orbital artery. It often develops as a result of a chronic form of pathology or after severe traumatic brain injury.
Clinical symptoms of acute retinal ischemia are manifested by the following symptoms:
- Sharp deterioration in vision.
- Sudden partial loss of vision.
- Limitation of the visual field.
- Complete blindness.
These signs can appear in one or two eyes at the same time.
Chronic course of retinal ischemia
It is important to contact in the first hours after an acute vascular accident in the retinal area, so that doctors can quickly and without complications eliminate the pathology
Ischemic processes disrupt normal blood flow in the retina, which leads to its insufficient supply of nutrients. The chronic form of the pathology develops against the background of various pathologies. Among them, the following stand out:
- Systemic diseases.
- Injury to the head and eyeball.
- Retinal sclerosis.
- Arterial stenosis.
- Hypotension.
- Anemia.
- Diabetes.
- Chorioretinal degenerations.
Often the cause of chronic retinal ischemia is endocrine diseases.
This form of pathology has characteristic symptoms:
- Gradually clarity of vision.
- Partial blindness develops.
- The retina acquires a grayish tint and becomes cloudy.
- A red spot appears in the center of the retina.
In the initial stage of the pathology, the optic disc has a pink tint. With the development of pathology, it becomes paler and completely atrophies.
How to make a diagnosis?
Medications are very effective, but most of them are serious and require only medical prescription
Only an ophthalmologist can diagnose retinal ischemia. To do this, the doctor conducts a physical examination and prescribes a special examination.
To promptly identify the presence of this disease and determine its stage of development, the following is carried out:
- Ophthalmoscopy.
- Examination with a fundus lens.
- Optical coherence tomography.
- MRI.
Typically, the diagnosis of retinal ischemia does not require special preparation and the examination can be carried out on the day of visiting a doctor. The method is selected in each case individually.
What pathologies does it differentiate with?
To accurately diagnose retinal ischemia, a comprehensive examination is often used. Its results allow us to differentiate this pathology from diseases such as:
- Blockade of the central retinal artery.
- Disruption of blood flow in the retinal vein and its branches.
- Ischemia of the anterior segment of the optic nerve.
- Damage to the retrobulbar part of the optic nerve.
- Toxic damage to the optic nerve under the influence of chemical compounds.
Timely diagnosis of retinal ischemia allows you to quickly select adequate treatment. This significantly reduces the risk of developing irreversible changes in the tissues of the eyeball, which lead to total blindness.
Therapeutic methods
In some cases, the cause of retinal ischemia can only be eliminated through surgery.
Modern medicine makes it possible to treat retinal ischemia using conservative and surgical methods. The conservative course includes the prescription of antispasmodics, anticoagulants, vitamins and drugs with anti-sclerotizing properties.
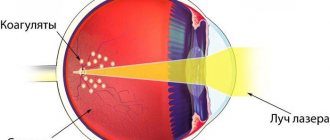
Surgery is performed using laser and microinvasive methods. In complex forms of pathology, it is the only way to restore vision. It is also recommended if conservative methods are ineffective.
As an auxiliary therapy, therapeutic courses can be prescribed to treat concomitant diseases that provoke the development of retinal ischemia. Usually this is a complex that includes taking medications and undergoing physiotherapeutic procedures. In some cases, surgery is recommended to eliminate such pathologies.
Treatment of retinal ischemia requires careful monitoring. Therefore, it is better to take the therapeutic course in a hospital. In such conditions, it is possible to carefully monitor the dynamics of recovery and, if necessary, correct treatment.
Drug therapy
In acute retinal ischemia, treatment must be started immediately. For this, ophthalmologists recommend taking the following medications:
- Nitroglycerin tablets: one tablet under the tongue. This drug has an antianginal effect. Its average price is 37 rubles.
- Atropine in the form of a 0.1% solution. It is used for retrobulbar administration. Single dose 0.5 ml. The average cost of the drug is 70 rubles.
- Aminophylline solution 2.4%. Used for infusion administration. Single dosage of the drug is 10 ml. It is an affordable medicine in the mid-price category. Its cost does not exceed 120 rubles.
- Papaverine in solution form. Used for intramuscular injections and intravenous administration. Single dosage 1-2 ml. The price of the drug is within 570 rubles.
- To reduce cholesterol levels and improve tissue nutrition, systematic intake of vitamin complexes is prescribed. They should include retinol, ascorbic acid, vitamins B6 and B12. The average cost of such drugs varies from 150 rubles to 370 rubles.
- Fibrinolysin. The solution is used for retrobulbar administration of 5-10 units. The price of the drug is within 270 rubles.
The selection of the drug, its dosage and regimen of use are prescribed only by an ophthalmologist after a thorough examination and examination. Self-medication of this pathology is categorically unacceptable.
Operations in the treatment of retinal ischemia
Preventive examinations with an ophthalmologist will help identify predisposition to the development of circulatory disorders in the retina
This technique is aimed at improving blood supply and nutrition to the retina. All operations are divided into three main groups:
- Revascularization of the retrobulbar part of the eye with the involvement of ocular muscles, episcleral tissue, implants in the episcleral space. Depending on the type, the cost of the operation is 14,000-48,000 rubles.
- Surgical interventions on large and small vessels that participate in the blood supply to the eyeball. The price of such surgical treatment is within 60,000 rubles.
- Decompression surgery on the optic nerve. The cost of such operations is 27,000-39,000 rubles.
The method of surgical resolution is the most effective method of treating retinal ischemia. The method and type of operation are selected individually in each case.
To carry out any surgical intervention and during the recovery period, specialized conditions and medical supervision are required. This treatment is carried out only in a hospital setting.
The consequence of retinal ischemia of any form is a decrease in the level of visual acuity, partial or total blindness. The prognosis for recovery is not very favorable. Full restoration of vision is possible only at a relatively young age. Therefore, it is important to monitor the condition of your eyes and contact an ophthalmologist at the slightest decrease in your vision level.
In the video, ophthalmologists talk about the symptoms, diagnosis and treatment of retinal artery thrombosis, and give advice on
Select it and press Ctrl+Enter to let us know.
Source: https://glaza.online/zabol/setch/ishemiya-glaza.html
Symptoms and treatment
In acute blood flow disorders, complete or partial loss of vision almost always occurs, which is caused by acute hypoxia of the retina and optic nerve. In some cases, during treatment the process stabilizes and vision improves. However, most often repeated courses of therapy are required.
Quite often, ischemic optovascular syndrome is the first manifestation of ischemic events in the coronary and cerebral vessels. In this regard, it is necessary to treat not only ocular ischemia, but also the underlying disease that caused the disruption of blood flow.
Central retinal artery occlusion
Occlusion of the central retinal artery or its branches may be associated with spasm, vascular thrombosis, or embolism. Arterial spasm is associated with vegetative-vascular disorders, and in elderly patients - with organic damage to the vascular wall against the background of atherosclerosis, hypertension, etc. If we trace the frequency of systemic diseases that led to occlusion of the retinal arteries, it turns out that 25% had hypertension, 7% had rheumatic heart disease, 3% had temporal arteritis, and 35% had atherosclerosis of the blood vessels and heart. About 25% of occlusions in the retinal vessels turned out to be idiopathic, that is, the cause could not be determined.
Occlusion of the retinal arteries in most cases is unilateral, with men predominating among the patients. The average age of patients is 55-60 years (from 20 to 85 years).
Clinical signs and symptoms of acute retinal occlusion
Patients with retinal occlusion complain of a sudden, persistent decrease in vision. Sometimes (when only the branches of the central artery are affected) only sectoral loss of vision occurs. In 10-15% of cases, short-term loss of vision is observed, which precedes the final ischemic events in the retinal vessels.
In approximately 10% of patients, complete blindness occurs; in half of the patients, vision is reduced to counting fingers in front of the face; in 20% of cases, visual acuity is 0.1-0.2. If occlusion occurs in only one of the branches of the central artery, then vision can be preserved, but there is loss of visual fields.
Central artery embolism develops predominantly in young patients with acute infections, sepsis, endocrine disorders, trauma and rheumatism.
Diagnostics
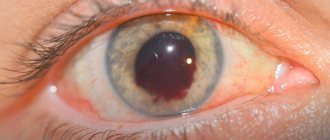
To identify manifestations of acute ischemia, it is necessary to perform ophthalmoscopy, in which the appearance of gray-white diffuse opacification of the retina is noted, as well as narrowing of the central retinal artery and its branches. The area of the fovea contains a zone of bright red hyperemia, which looks like a cherry pit against the background of a pale retina. This diagnostic sign is associated with transillumination of the choroid in the area of thinning of the retinal substance. In the initial stages of the disease, the optic disc is pink in color, but later it also turns pale due to atrophic processes.
There are cases when characteristic ophthalmoscopic signs cannot be identified. In this case, retinal edema can be located only paramacularly or in the form of separate areas. The diameter of the artery decreases slightly, since the degree of occlusion is small. If there is an anatomical feature in the form of an additional cilioretinal artery, then the cherry pit symptom may be absent during ophthalmoscopy. By maintaining blood flow in the central zone, visual acuity is usually preserved.
The prognosis for patients with central artery embolism is poor. If there was an artery spasm in young patients, then vision can be restored almost completely, but in older patients the percentage of restoration of visual function is much lower.
Diagnosis and treatment of ischemic optic neuropathy
Ischemic neuropathy is a vascular pathology of the optic nerve, characterized by a sudden disruption of the arterial blood supply. The disease leads to a sharp decrease in vision and blindness in people over 50 years of age, mainly in males.
Today, the incidence of vascular pathology has increased among young people. Ischemic facial neuropathy is a shocking condition for many patients due to its sudden onset.
There are two forms:
The first ocular ischemic syndrome is caused by ischemia, or disruption of blood circulation, in the arteries supplying the anterior portion of the optic nerve.
Ocular ischemic syndrome
The optic nerve contains approximately 1.2 million nerve fibers, and all visual images that a person sees come through it. If the access of oxygen and nutrients to the nervous tissue is stopped, loss of visual acuity and field of vision occurs.
Classification of the anterior form depending on circulatory disorders:
- Arterial. The most dangerous, develops against the background of inflammatory diseases of large arteries.
- Non-arterial. The most common form usually has the best prognosis. Occurs against the background of systemic diseases.
- Venous circulation.
Etiology
The reasons that characterize the appearance of anterior ischemic neuroopticopathy:
- hypertension;
- giant cell temporal arteritis;
- antiphospholipid syndrome;
- periarteritis nodosa;
- radiation necrosis;
- atherosclerosis;
- diabetes;
- systemic lupus erythematosus;
- anemia (sickle cell, hemolytic);
- hypotensive shock.
Systemic lupus erythematosus
Posterior ischemic neuropathy occurs under the influence of prolonged neuro-emotional stress, psychological trauma, and sudden jumps in blood pressure.
Epidemiology
Non-arterial ischemic optic neuropathy is 6 times more common. The age of patients ranges from 30 to 85 years.
Pathogenesis
The main factor in the appearance is stenosis or occlusion of the arterial vessels supplying the nerve, and the resulting imbalance between intravascular and intraocular pressure.
This is due to the peculiarities of its anatomy: the area has the smallest diameter (1.5 - 1.6 mm), nutrition is provided only by return branches from the retina and small arterioles from the choroid and posterior ciliary arteries.
The clinical course and diagnosis depend on the form.
AION (anterior ischemic optic neuropathy) associated with arteritis
This form is a consequence of giant cell arteritis (GCA). Anterior ischemic optic neuropathy presents with sudden, significant monocular vision loss that may be accompanied by periocular tenderness. Sometimes predecessors appear:
- fog before the eyes;
- appearance of light flashes.
Cloudiness before the eyes
In most cases, ischemic thrombosis appears several weeks after the onset of GCA. When clarifying the medical history, patients indicate:
- previous headache;
- soreness of the head muscles;
- masticatory muscles;
- polymyalgia rheumatica.
Signs
- Pain and decreased pulsation of one or both temporal arteries.
- A very light-colored (“chalky”) optic disc edema indicates GCA.
- After 1-2 months, the swelling gradually subsides, but pronounced atrophy of the optic nerve remains.
- FA reveals significant choroidal hypoperfusion.
- ESR, C-reactive protein, and platelet levels are elevated.
Important! It is advisable to perform a temporal artery biopsy within 7 days of starting treatment. Histological confirmation of GCA may serve as a basis for long-term use of steroids.
Treatment of anterior ischemic pathology cannot be delayed until the results of the biopsy are obtained.
But, with inadequate use of hormones, more harm can be done to the body. Due to complications associated with their use, it is necessary to replace them with second-line drugs, for example Azathioprine.
The drug Azathioprine
Forecast
Adverse. Vision loss is often irreversible; a well-chosen course of steroids can contribute to its partial restoration.
PION not associated with arteritis
Neuropathy results from partial or complete infarction of the optic nerve head. It often occurs without accompanying symptoms in patients aged 55 to 70 years.
Predisposing factors:
- arterial hypertension;
- SD;
- hypercholesterolemia;
- collagen vascular diseases;
- antiphospholipid syndrome (APS);
- hyperhomocysteinemia;
- vascular collapse;
- condition after cataract removal;
- sleep apnea syndrome;
- use of sildenafil (Viagra).
Neuropathy of the anterior part of the optic nerve as a result of impaired venous circulation
In rare cases, venous circulation in the optic nerve is impaired.
The pathogenesis and clinical picture are somewhat reminiscent of thrombosis of the trunk of the central retinal vein. In this case, vision decreases gradually over several days, reaching tenths, hundredths of a unit or counting fingers on the face.
Central paracentral scotomas are identified in the field of view. A couple of days after decreased vision in the fundus, the optic disc is somewhat swollen, hyperemic, the veins are moderately dilated, the arteries are not changed, and are of normal caliber. In contrast to arterial ischemia, when venous circulation is impaired, vision decreases gradually, visual functions suffer less, so the prognosis is better.
With fluorescein angiography, in some cases it is detected in the late phases of staining the walls of dilated retinal veins with a contrast agent, which is associated with a partial disruption of the outflow of venous blood.
This disorder in the anterior part of the optic nerve is sometimes called vascular papillitis. As a separate type, ocular ischemia is rare; mixed arteriovenous pathology is more common.
Arteriovenous malformation
Treatment
Ocular thrombosis is an emergency condition that requires emergency hospitalization in the ophthalmology department of the hospital.
The goal of treatment is to prevent damage to the second eye and achieve remission.
Pharmacological treatment required for the treatment of ischemic stroke of the optic nerve:
- Vasodilators (papaverine, bencyclane, aminophylline, xanthinol nicotinate, nicoshpan).
- Vasoactive drugs (vasobral, nicotinoyl gamma-aminobutyric acid).
- Anticoagulants (heparin, nadroparin calcium)
- Antiplatelet agents (aspirin, dipyridamole, pentoxifylline).
- Hemocorrectors (dextran).
- Osmotic agents (triampur compositum, furosemide).
- Local antihypertensive drugs (timolol, dorzolamide - reduce IOP).
- Metabolism correctors. Antioxidants (ascorbic acid, vitamin E, rutoside, retinalamin, cortexin, taurine, strix, aevit.
- Anti-sclerotic drugs (statins to lower cholesterol - lovastine, simvastine, fluvastine).
- Fibrates (to reduce the level of triglycerides in the blood - bezafibrate, fenofibrate).
The drug Fenofibrate canon
Anterior ischemic neuropathy is a polyetiological disease, being an ocular symptom of various systemic diseases.
Traditional treatment is an additional method, but nothing more. Eyes after such a pathology require thorough treatment.
A case study based on a scientific institute
Anterior ischemic neuropathy associated with APS (antiphospholipid syndrome) is an unusual form of pathology characterized by recurrent arterial or venous thrombosis, recurrent miscarriage and thrombocytopenia in the presence of antibodies to phospholipids - a lupus anticoagulant.
Patient K., 61 years old, applied to the Research Institute of Eye Diseases with complaints of decreased vision in her left eye and a “floating” dark spot in front of it.
History of 4 spontaneous miscarriages followed by infertility. Episodes of arthritis of large and small joints, laboratory signs of kidney damage, and an increase in blood pressure to 160/100 mm Hg were recorded. Art.
During examination, antinuclear factor, antibodies to DNA, and elevated ESR were detected in the blood, on the basis of which a diagnosis of systemic lupus erythematosus (SLE) was made.
Upon presentation, visual acuity of the left eye was 0.9, uncorrected, followed by a decrease to 0.1 within 1 week. In the field of view - absolute and relative scotomas, mainly in the lower half. In the fundus there is ischemic edema, blurring of the boundaries of the optic disc, streak-like hemorrhage on the disc.
Fundus examination
To confirm the diagnosis, electrophysiological methods were used, which revealed a decrease in the conductivity of the axial bundle of the optic nerve of the left eye to 26 Hz.
Optical sections of the disc area obtained during retinal CT revealed signs of thinning of the neuroglial belt, which indicates swelling of the optic disc area.
For the purpose of differential diagnosis between optic neuritis as a manifestation of lupus vasculitis and ischemic neuropathy, a study of ocular hemodynamics using color Doppler mapping was carried out.
A pronounced decrease in systolic blood flow velocity was detected, an increase in the resistance index was noted in the central retinal artery, posterior short ciliary arteries, and the ophthalmic artery of the left eye, which confirmed the ischemic nature of optic neuropathy.
The patient was prescribed a direct anticoagulant - heperin clexane, the duration of treatment of which was 2 months, with a further transition to an indirect anticoagulant - warfarin. In addition, antiplatelet agents (thrombo-ASA), vasoactive (Cavinton), metabolic drugs and antioxidants (Mexidol, Emoxypine) were prescribed.
Various forms of the drug Mexidol
During treatment, positive dynamics were observed in the visual field of the left eye, which was manifested by a decrease in the number of scotomas. Visual acuity remained stable at 0.1. When returning after 4 months, partial atrophy of the optic nerve was detected.
This observation is presented in order to draw attention to a rare form of MN pathology and the difficulties of differential diagnosis.
Compression-ischemic neuropathy refers to polyetiological diseases, being an ocular symptom of various systemic processes. Therefore, in the prevention of pathology, the clinic of the underlying disease should be taken into account.
“Loss of vision in one eye - what to do?”
This video explains why loss of vision in one eye can occur. What could be the predecessors and what to do in such a situation.
Source: https://stopvarikoze.ru/ishemiya/diagnostika-i-lechenie-perednej-ishemicheskoj-nejropatii-zritelnogo-nerva.html
Clinical guidelines
In case of acute disruption of blood flow through the central retinal artery as a result of spasm, it is necessary to immediately begin treatment, which includes:
- Nitroglycerin (1 tablet under the tongue);
- Amyl nitrite (2-3 drops on a cotton ball should be inhaled);
- Atropine (0.1% solution is administered retrobulbarly, 0.5 ml);
- Xanthinol nicotinate (15% solution is administered retrobulbarly at 0.3-0.5 ml);
- Eufillin (2.4% solution, 10 ml, administered intravenously);
- Papaverine (1-2 ml is administered intramuscularly or intravenously).
If central artery thrombosis occurs, anticoagulant therapy should be performed:
- Fibrinolysin and heparin (5-10 units) are administered retrobulbarly;
- Heparin (5-10 units) is administered subcutaneously 4-6 times a day;
- Finilin (0.03 mg) is administered 4 times a day during the first few days of the disease, after which the frequency of administration is reduced to 1 time a day.
When using anticoagulants, it is necessary to monitor the parameters of the blood coagulation system, including prothrombin time.
In addition, for the treatment of patients with arterial occlusion, vitamins B 6 and 12, C, A, miscleron, and methionine should be prescribed.
Ischemic diseases of the retina and optic nerve
Diseases of the vascular system of the visual organs in people of various ages are one of the leading causes of low vision, blindness and disability. In recent years, the number of ischemic eye diseases has increased. The reason for this is the spread of atherosclerosis, coronary heart disease, hypertension and diabetes mellitus.
Classification, etiology and pathogenesis of ischemic eye diseases
Currently, there is no unified classification of ischemic eye lesions. There is a close relationship between damage to various parts of the circulatory system and the pathogenetic mechanisms of ischemia. This is the reason that ischemic diseases of the organs of vision do not have a single pathogenesis; they are characterized by polyetiology and diversity of clinical picture
The clinical picture of damage to the posterior segment of the eye is determined by the characteristics of the blood supply to the retina and optic nerve. Ischemic processes in the eyeball can be acute and chronic.
An acute ischemic process in the posterior segment of the eye is characterized by circulatory disorders in the central artery or central vein of the retina, as well as anterior or posterior ischemic neuropathy or acute toxic neuropathy.
Acute ischemia can develop as a result of existing chronic ocular ischemia, which occurs due to diabetic or hypertensive angioretinopathy, degenerative changes in the retina, stenosis of the carotid and orbital arteries, as well as temporal arteritis.
Ocular ischemia also develops against the background of eye and head injuries, as well as general angiospastic diseases. It can be triggered by hypotension that occurs when taking a number of medications.
Ischemia of the organ of vision can develop after surgical interventions that were performed against the background of anemia, accompanied by the formation of microemboli and disorders of the blood coagulation and anticoagulation systems.
Acute circulatory disorders in the optic nerve and retina quite often cause partial loss of vision or blindness. In this case, the prognosis is more than serious, but not hopeless. After treatment, sometimes there is improvement or stabilization of the pathological process.
In most cases, repeated courses of treatment may be necessary. It should be noted that ischemic optovascular syndrome can be a precursor of ischemic cerebral or coronary attacks.
If it occurs, it is necessary to conduct a full examination and treatment of concomitant diseases.
Blockage of the central retinal artery
The cause of occlusion of the central retinal artery and its branches is spasm, embolism or thrombosis of the vessel. When arteries spasm, vegetative-vascular disorders occur. In older people, it manifests itself as organic changes in the vascular wall caused by hypertension, atherosclerosis and other diseases.
Occlusion of the central retinal artery mainly develops on one side. The disease occurs in people of different ages - from 20 to 85 years. Most often it affects men.
Clinical signs of the disease
Patients complain of a sudden and persistent decrease in vision or sectoral loss of visual fields. In 10-15% of cases, short-term blindness develops before the development of a complete picture of occlusion.
In 10% of patients, complete blindness develops, in 50% visual acuity decreases to the ability to count fingers on the face, and in 20% of cases - to 0.1 - 0.2.
If only one branch of the central retinal artery is affected, then visual acuity may remain at the original level, but defects appear in the visual field.
In typical cases, fundus ophthalmoscopy visualizes gray-white diffuse opacification of the retina, as well as narrowing of all branches of the central retinal artery. In the area of the central fovea, against the background of general blanching of the retina, an area of bright red hyperemia is determined.
This is a symptom of "cherry pit". It occurs due to thinning of the retina in this place and a bright red translucent appearance of the choroid.
At the beginning of the pathological process, the optic disc remains pink in color, and then, due to the development of atrophy, gradually turns pale.
Sometimes there may be no characteristic ophthalmoscopic picture. In this case, the area of retinal edema can be located only in the form of separate areas or paramacularly.
The arteries may be slightly narrowed. If there is an additional cilioretinal artery, then the cherry pit symptom may not be present.
In this case, due to the preservation of central vision, sufficient acuity is ensured.
Forecast
For embolism of the central retinal artery, the prognosis is pessimistic. In the case of spasm, vision in young people may return almost completely, but in older people the prognosis is less favorable.
Emergency care and treatment of acute thrombosis of the central retinal artery
In case of acute thrombosis of the central retinal artery, it is necessary to take and apply local vasodilator drugs. You should put one nitroglycerin tablet under your tongue and inhale the vapor of 2-3 drops of amyl nitrite located on a cotton swab.
Aminophylline solution 2.4% - 10 ml is administered intravenously; retrobulbar - or 0.1% solution of atropine sulfate 0.5 ml, or 15% solution of xanthinol nicotinate 0.3 - 0.5 ml.
You should also perform an intramuscular injection of 1 or 2 ml of xanthinol nicotinate 15% solution or 1-2 ml of papaverine hydrochloride 2% solution.
Anticoagulant therapy is carried out under the control of blood clotting parameters. For this purpose, fibrinolysin with heparin is administered retrobulbarly, and heparin is administered subcutaneously 4 to 6 times a day. Subsequently, they switch to indirect-acting anticoagulants, which include phenylin. Anti-sclerotic drugs and vitamins A, C, B6 and B12 are also prescribed as auxiliary therapy.
The best eye clinics in Moscow where ischemic diseases of the retina and optic nerve are treated
- Moscow Eye Clinic
- Clinic of Dr. Shilova T.Yu.
- MNTK named after S.N. Fedorov
All eye clinics in Moscow >>>
Ischemic diseases of the retina and optic nerve
Source: //prokonyuktivit.ru/ishemicheskie-zabolevaniia-setchatki-glaza-i-zritelnogo-nerva.html