Uveitis.
This is a fairly common pathology of the eye, explained by the fact that the choroid consists of a large number of vessels that form a dense network with a very slow blood flow. Due to the slow blood flow, many toxic and infectious agents (bacteria, viruses) settle in the choroid, causing acute and chronic inflammation (uveitis). If the entire choroid becomes inflamed, panuveitis develops.
Often, due to the fact that the anterior part (iris and ciliary body) and the posterior part (choroid) have separate blood supply, inflammation develops only in the anterior part - iridocyclitis (anterior uveitis) or only in the posterior part - choroiditis (posterior uveitis) of the choroid. Sometimes one iris becomes inflamed (iritis) or the ciliary body (cyclitis).
Causes. Inflammation of the choroid can occur with common infectious diseases (influenza, tuberculosis, syphilis, toxoplasmosis, etc.), with so-called focal infections (foci of inflammatory processes in carious teeth, paranasal sinuses, tonsils and other organs), rheumatism, polyarthritis, allergic diseases etc. Examination and treatment of patients with uveitis is carried out in an ophthalmological hospital.
Vascular diseases of the retina (macular edema, thrombosis, vascular damage, etc.)
The main cause of incurable blindness is usually vascular diseases of the eyes.
Obstruction of a vessel or insufficient blood flow for normal blood circulation leads to heart attacks, microinfarctions, or simply chronic oxygen deficiency in the vessels of the organ of vision. Oxygen starvation is especially dangerous for the most important layer of the eye - the photosensitive layer of the retina. The complex structure of the retina dictates especially high requirements for blood supply in its structures. If the central retinal artery is completely obstructed, vision can disappear in a few seconds!
A characteristic feature of all vascular diseases of the retina is a local circulatory disorder, leading to arterial obstruction and vein thrombosis.
Among the vascular diseases of the retina, the following are the most common:
1
Structure of the eye and eyeball
2
Diagnosis and treatment of vascular diseases of the retina
3
Treatment of retinal vascular diseases
Retinal swelling
Retinal edema is associated with vascular damage and accumulation of moisture and protein structures in the retina. This is not an independent disease, but a symptom of some pathology. For example, macular edema of the retina can occur as a result of diabetes mellitus, vascular and inflammatory diseases.
Diabetic retinopathy
Diabetic retinopathy is a rather insidious disease that develops against the background of elevated blood sugar levels and has no symptoms in the initial stages. If traumatic retinopathy occurs as a result of eye injury and is manifested by swelling and hemorrhage, then diabetic retinopathy develops quietly and unnoticeably.
However, if treatment is not started early, retinal detachment can occur, leading to blindness. This type of disease is characterized by neovascularization - pathological growth of blood vessels.
More detailed information about this vascular disease of the retina can be found here.
Retinal angiopathy
Angiopathy is a lesion of retinal vessels of different diameters. With angiopathy, the vessels become narrow and tortuous.
Among the reasons for the development of this pathology are the following diseases: diabetes mellitus, eye injury, vasculitis, cervical osteochondrosis, high blood pressure.
You can read about the symptoms of this disease and what methods are most effective for treating it here.
Retinal vein thrombosis
Symptoms of thrombosis of the central branch of the retina are simple: the appearance of blind spots in the visual field or a noticeable but painless deterioration of vision in one eye. Most often, this pathology affects elderly people.
The provoking factors of this retinal vascular disease are:
When unfavorable conditions arise, the walls of the arteries thicken and become dense, which leads to compression of the adjacent vein. In the vein, blood flow slows down, forming a blood clot (thrombus).
Blood stagnation increases vascular permeability, the liquid part of the blood fills the vascular space, which leads to retinal edema and hemorrhages.
Retinal vein thrombosis can appear on the central vein and in its branches, developing in ischemic and non-ischemic types .
With non-ischemic damage, slight changes appear in the fundus of the eye, and a slight drop in visual acuity is observed.
The ischemic type is characterized by the occurrence of multiple hemorrhages and cotton wool-shaped (blind) lesions in the retina. In this case, a significant deterioration in vision occurs.
Due to the risk of various complications with such disorders, it is necessary to come for an examination by an ophthalmologist every 2 weeks.
1
Diagnosis and treatment of retinal vascular diseases
2
Diagnosis and treatment of retinal vascular diseases
3
Diagnosis and treatment of retinal vascular diseases
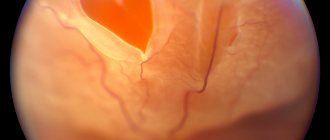
Occlusion of the central retinal vein and its branches
Occlusion of the veins and central retinal artery, due to the speed of changes occurring, is sometimes called a “vascular catastrophe”, which results in a rapid decline in vision.
Occlusion of the central retinal vein is a deterioration in the blood circulation of the central retinal vein and its branches.
With this vascular disease of the retina, the patency of the central vein is completely disrupted, and pinpoint hemorrhages occur in all squares of the retina.
Tortuosity and dilatation of veins, cotton wool lesions, papilledema, and the appearance of neovascularization of the retina, iris, and disc are observed. Within ten days, vision (in one eye) will continue to decline, but this will not lead to complete blindness.
Central retinal artery occlusion
When the central retinal artery is occluded, a symptom such as sudden loss of vision is observed.
A person can only distinguish between light and darkness and can barely see his fingers in front of his eyes. Before the onset of the disease, the patient develops short-term episodes of complete blindness. This disease occurs 2 times more often in men than in women. Occlusion of the central retinal artery can occur in both 25-year-olds and people over 85 years of age.
When the peripheral branches of the retinal arteries become inflamed, the patient experiences partial loss of vision.
Causes of the disease
The cause of the development of this vascular disease of the retina may be:
- atherosclerosis (every third disease of the choroid occurs for this reason);
- hypertension (every fourth disease);
- rheumatism;
- temporal arteritis;
- neurocirculatory dystonia, arrhythmia.
If treatment for this disease is not started promptly, complete loss of vision is possible.
1
Diagnosis and treatment of retinal vascular diseases
2
Diagnosis and treatment of retinal vascular diseases
3
Diagnosis and treatment of retinal vascular diseases
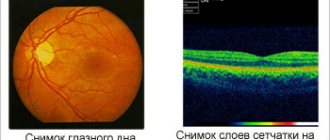
Diagnosis of vascular diseases of the retina
When diagnosing vascular diseases of the retina, the patient’s medical history and complaints are taken into account, laboratory techniques and physical examination methods are used.
The ophthalmologist collects data on the presence of family diseases, previous “vascular accidents” (thrombosis of the veins of the extremities, stroke and myocardial infarction, etc.), medications taken by the patient.
Physical examination includes the following techniques:
Treatment of vascular diseases of the retina
Treatment of retinal edema and other vascular diseases of the retina is aimed at reducing edema, improving blood flow in the affected vein, optimizing retinal trophism, and resolving retinal hemorrhages.
Therapy for retinal vascular diseases includes:
- thrombolytic drugs;
- vasodilators;
- endothelial protectors;
- antiplatelet agents.
Source: //www.mediccity.ru/directions/633
Iritis (inflammation of the iris).
Iritis (inflammation of the iris) usually begins with aching pain in the eye, which can spread to the temple, the entire half of the head on the side of the affected eye. It is difficult for the patient to look at the light (photophobia, lacrimation, blepharospasm), and the vision of the affected eye deteriorates. The eye turns red (a pink-violet halo appears around the limbus - pericorneal injection). Unlike conjunctivitis, the conjunctival cavity is clean, there is no discharge; unlike keratitis, the cornea remains shiny and transparent. The iris changes its color.
If you compare the iris of a healthy and diseased eye, you will see that in the diseased eye the iris is cloudy, there is no characteristic pattern of depressions - iris crypts, dilated vessels are visible in it. Due to swelling of the iris tissue, the pupil narrows, which is also especially noticeable when comparing the diseased and healthy eyes.
The pupil of a diseased eye is much smaller and does not react as quickly to light as that of a healthy eye. This distinguishes iritis from an acute attack of glaucoma . In an acute attack of glaucoma, the pupil in the affected eye is wider than in the healthy eye and does not narrow when the eye is illuminated. In addition, iritis differs from glaucoma in that upon palpation the eye seems softer than a healthy one, and in an acute attack of glaucoma it appears much harder.
A particularly peculiar symptom of iritis are the so-called adhesions (synechia). These are the adhesions of the iris to the anterior surface of the lens (posterior iris commissures) or the cornea (anterior iris commissures). They are most clearly detected when drugs that can cause dilation of the pupil (mydriatics) are instilled into the eye: 1% platyphylline solution, 1% homatropine hydrobromide solution, 0.25% scopolamine hydrobromide solution or 1% atropine sulfate solution.
If instillation of these solutions into the conjunctival sac of a healthy eye leads to a uniform dilation of the pupil, maintaining a regular round shape, then in the presence of adhesions of the iris, the pupil dilates unevenly and its shape becomes irregular. (hypopyon) may appear in it
Etiology and pathogenesis of vascular diseases of the optic nerve
The main causes of damage to the vessels of the optic nerve and the entire brain are atherosclerosis, hypertension and arterial hypotension, vascular dystonia, nonspecific aortoarteritis, temporal arteritis, nodular periarthritis, diabetes mellitus. Among the factors contributing to the development of circulatory disorders, discopathy of the cervical spine, and primarily osteochondrosis, is of great importance. In this case, both a purely mechanical factor is important - compression of vessels by osteophytes, their displacement in the spinal canal - and a neuroreflex mechanism associated with irritation of the cervical sympathetic plexuses. The main etiological factor is atherosclerosis. Atherosclerotic lesions of vessel walls vary: from small changes (such as lipoidosis) to plaques with atheromatous decay. Atherosclerotic changes develop first in individual sections of the arteries, localizing most often in the area of mouths, branches, and bends of blood vessels, gradually affecting more and more new areas. As a result of thrombus formation, the lumen of the vessel supplying the optic nerve gradually closes, atrophic foci appear, which are subsequently replaced by scar tissue, and atrophy of the nervous tissue occurs. This is how stenosis of the vessels supplying the optic nerve develops. According to many experts, stenotic processes in the orbital and posterior ciliary arteries are of greatest importance.
Iridocyclitis.
Iridocyclitis is an inflammation of the iris and ciliary body, characterized by the same clinical symptoms as iritis, but even more pronounced. There are pain in the eye and headaches, decreased vision, photophobia, lacrimation, changes in the color and structure of the iris, and the moisture in the anterior chamber becomes cloudy. Deposits of cellular elements may appear on the posterior surface of the cornea - precipitates - of different colors and sizes.
Due to the fact that the exudate enters the vitreous body, it becomes cloudy and during ophthalmoscopy the reflex from the fundus of the eye becomes dull; floating semi-fixed or fixed opacities in the form of threads, strands, flakes are detected in the vitreous body. Another symptom characteristic of cyclitis is pain in the area of the ciliary body, which is detected by palpating the eyeball through closed eyelids (the same way as is done to determine intraocular pressure.
Due to a disruption in the formation of aqueous humor in the ciliary body, intraocular pressure decreases, and the eye is soft and hypotonic on palpation. If the iris along the entire pupillary edge is fused to the lens (pupil fusion) or the entire pupil is filled with exudate (pupil occlusion), then due to a violation of the outflow of aqueous humor, intraocular pressure may increase and the eye will be hard on palpation.
Eye stroke (occlusion) - symptoms, treatment, causes, consequences
In modern medicine there is no diagnosis of “ocular stroke” - this is a definition of occlusive pathologies of the retina, blockage or rupture of the vessels supplying the eyeball, transient cerebral circulatory disorders (transient ischemic attacks) or acute circulatory disorders (cerebral strokes), which lead to various pathological conditions with damage to the organ of vision and are manifested by specific symptoms.
At the same time, they develop:
1) pathology of retinal vessels:
– artery occlusion and retinal detachment;
– separation of retinal veins;
– central occlusion of the artery;
2) stroke of the optic nerve, developing with damage to the optic lobes, the center of gaze in the precentral gyrus, oculomotor centers, or with foci of necrosis or intracerebral hemorrhages in the area of the optic chiasm.
Causes and risk factors
The relevance of considering this issue is that, according to statistics, about 30% of patients with stroke do not notice or do not attach importance to the manifestations of the disease.
Vascular pathology of the retina or disorders of the blood supply in the area of the visual center, optic chiasm due to transient disturbances in the nutrition of neurons or small foci of stroke - the disease can proceed unnoticed and not cause concern in patients.
In most cases, people do not even realize that they are in serious danger and consider all signs of visual impairment to be age-related, because most often the disease occurs in people over 50-60 years of age.
In addition, neurologists note a more severe course of ocular strokes in elderly patients.
But there are certain risk factors that contribute to the occurrence and progression of vascular pathology of the retina and optic nerve
in people of young and mature age:
- constant and prolonged overstrain of the visual organs as a result of working with papers or at a computer monitor;
- excessive fatigue, mental or physical fatigue;
- stress, nervous and psychological disorders;
- violation of diet (excessive consumption of fried, spicy, fatty foods, pickled and salty foods);
- complicated heredity (predisposition to vision pathologies, acute disorders of cerebral circulation, vascular spasms);
- long-term use of medications that contribute to the progression of vision pathology and vascular disorders (corticosteroids, oral contraceptives);
- bad habits (smoking, excessive alcohol consumption, drug addiction).
Causes of eye stroke
Ischemic cerebral disorders occur due to vascular occlusion - blockage of blood clots, emboli, particles of atheromatous plaques or as a result of prolonged spasm of the vessels of the eyeball and/or vessels of the brain and neck, causing disorders of the blood supply to areas of the brain in the area of the optic lobes, nerve fibers of the optic chiasm, oculomotor centers, the center of gaze in the precentral gyrus.
Vascular changes in the organ of vision are also caused by ruptures of retinal vessels or hemorrhagic strokes (bleeds into the brain).
The main causes of visual strokes include:
1) diseases with vascular lesions, which are accompanied by increased fragility, bleeding or thrombus formation:
- severe diseases of the heart and cerebral vessels: cerebral atherosclerosis, arterial hypertension, arrhythmias, endocarditis, heart attack and heart defects;
- vascular diseases: vasculitis, hemorrhagic diathesis, infectious-inflammatory or toxic diseases that are accompanied by changes in the vascular wall, congenital vascular diseases of the eye or cerebral arteries and veins (stenoses, kinks, arteriovenous malformations, aneurysms, stenoses);
2) diseases that contribute to degenerative changes in the vascular wall:
- infectious-toxic diseases of the brain (arachnoiditis, encephalitis, meningitis);
- tumors (atheromas, hemangiomas), brain metastases;
- pathological deposits in the vascular wall (amyloidosis, calcification);
- severe endocrine pathologies (hypothyroidism, diabetes mellitus, adrenal pathology);
- blood diseases.
The most common causes of ocular stroke are:
– damage to the vascular wall due to atherosclerosis, vasculitis, infectious-toxic changes in combination with arterial hypertension or frequent and prolonged spastic (vasomotor) paroxysms (with occlusive strokes or transient cerebrovascular accidents);
– a combination of hypertension or injury to the eye and/or brain with congenital vascular anomalies (the presence of aneurysms or malformations) with a hemorrhagic nature of the stroke (intracerebral or intraocular hemorrhages).
Symptoms and signs
The first warning signs of an ocular stroke are:
- temporary and/or progressive vision loss;
- gradual loss of peripheral vision;
- the appearance of white spots, glare, and other interference that blocks vision (“curtain effect”);
- sudden loss of areas of the visual field;
- color vision disorder.
It is important to remember that if any of these symptoms appear, you must immediately consult an ophthalmologist - timely diagnosis of pathological circulatory disorders of the eye and proper treatment prevent irreversible loss of vision and make it possible to fully or partially restore vision in case of an eye stroke.
Symptoms of eye stroke due to occlusion (blockage) of the central retinal artery
:
–
complete or partial loss of peripheral vision, which gradually develops into partial or complete loss of central vision (with retinal detachment);
– the appearance of blind spots, distorted outlines or distorted perception of the picture.
This pathology is considered one of the most dangerous and develops against the background of significant spasm or narrowing (atherosclerotic) of the carotid arteries, pathology of the vertebral arteries, severe heart disease, and the malignant course of hypertension.
In most cases, the disease is not accompanied by pain and patients do not pay attention to the manifestations of the disease, but prolonged occlusion of the central artery causes irreversible changes in the retina, up to complete blindness.
Occlusion and separation of the central retinal vein
This disease occurs when the venous outflow from the vessels of the retina is disrupted - blockage of the central retinal vein. Most often, this pathology develops in cases of blood clotting disorders, in patients with diabetes mellitus, atherosclerosis or other vascular changes.
The following are noted:
– deterioration of vision, initially peripheral with gradual loss of central vision;
– blurred images of objects;
– the appearance of floating reflections, clouding;
– loss of visual fields.
Most often, unilateral damage to the organ of vision is observed.
Signs of the disease appear in proportion to the degree of obstruction, they appear unexpectedly and gradually progress - from several hours to several days.
Centralized arterial occlusion occurs suddenly and is characterized by
unilateral loss of all visual functions (complete loss of vision).
For optic nerve strokes
which develop during the formation of a cerebral infarction or intracerebral hemorrhage in the area of the center of gaze in the precentral gyrus, the location of the oculomotor centers, optic chiasms, and optic lobes of the brain depends on:
- on the size and anatomical location of the stroke focus (cerebral hemispheres, brainstem, cerebellum, parieto-occipital lobe);
- degree of damage to the vascular system;
- type of stroke (hemorrhagic or cerebral infarction);
- side of the lesion.
Symptoms may occur:
– sudden blindness or a sharp decrease in vision in one eye with disturbances in movement (hemiparesis) and sensitivity in the arm and leg on the opposite side (cross syndrome);
– loss of visual fields (hemianopsia), often with preservation of color perception and visual acuity;
– acute pain, constriction of the pupil, limited eye mobility (ophthalmoplegia), nystagmus (swinging movements of the eyes), double vision, blindness in half of the eye on the side opposite to the lesion;
– various oculomotor disorders, strabismus.
The formation of visual images occurs in the visual lobes of the brain, so when they are damaged, loss of the corresponding parts of the visual fields develops.
The main harbinger of a stroke is the symptom of atrial scotoma (darkness) in the form of visual disturbances: periodic flickering of light - fog, glare, flickering, covering surrounding objects and rapidly increasing.
They are often accompanied by impaired skin sensitivity and paresthesia in various parts of the body. The duration of the attack can last from several minutes to several hours, then vision is completely restored.
This symptom often manifests itself against the background of hypertension, atherosclerosis, severe headache and nausea.
Treatment of eye stroke
Therapy for circulatory disorders of the eyeball, optic nerve, and retinal lesions is based on the diagnosis of pathology, identification of a blocked vessel (thrombosis or spasm) and/or determination of the type of microstroke.
When the first signs of an ocular stroke appear, you must consult an ophthalmologist to conduct a visual examination of the eye and fundus, if necessary, conduct an electronic scanning of blood vessels (fluorescence agiography), and consult a neurologist. Depending on the diagnostic results, methods of adequate therapy are determined - how to treat an eye stroke.
Treatment tactics and consequences of ocular stroke depend on the degree of obstruction, duration of the disease and timely administration of therapy.
In most cases, with early diagnosis and adequate treatment, there is a complete or partial restoration of all lost functions; there may be residual effects in the form of problems with distorted perception of objects, blind spots, partial loss of visual fields or distorted outlines.
The most dangerous thing is to ignore the appearance of alarming symptoms - this can lead to serious consequences if normal blood flow is not restored within the first hours after occlusion.
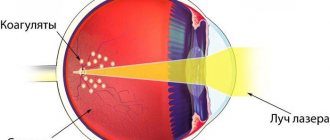
Modern laser surgery is considered the most effective method of treating the consequences of an ocular stroke, with timely access to specialists, successful relief of a “transient ischemic attack” and the absence of cerebral infarction or brain stroke - patients have every chance of complete restoration of vision.
Source: //zen.yandex.ru/media/id/5d903bd123bf4800ae3a9d31/5df327362beb4900b06ff6d5