Thinning of the retina occurs as a result of trophic disorders associated with severe somatic diseases, injuries or hereditary predisposition. In this case, the patient complains of lacrimation, photophobia, distortion of the shape and color of objects, as well as the inability to distinguish small objects and read.
Visual impairment can be observed in the periphery or in the center of the visual field and is caused by areas with a thin retina and a lack of light-sensitive cells.
Risk group
The process that results in thinning of the mesh area is largely associated with age-related changes occurring in the human body. However, this does not mean that the disease is diagnosed only in elderly people. Very often, symptoms of the disease are observed in children. According to research data, women are more susceptible to the disease. A high degree of myopia, chronic types of diseases of the vascular system and diabetes mellitus are just a small list of diseases that result in the development of pathology.
Retinal thinning is an irreversible degenerative disease. The causes of thinning of the retina may be hereditary. The disease affects people who have a white skin tone and light-colored iris. Constant stress, visual strain, bad habits and an unbalanced diet increase the risk of developing the disease.
Symptoms
Clinical manifestations of the disease depend on the type of dystrophy. Thinning of the retina in central dystrophy is accompanied by symptoms:
- Objects are partially out of sight, straight lines are distorted.
- Visual acuity is reduced.
- Color perception is distorted.
- Night blindness occurs.
If we are talking about the peripheral form of the disease, symptoms do not appear until the retina ruptures. In such cases, vision deteriorates sharply, flashes appear before the eyes, “spots”, “lightning”.
Factors provoking the development of pathology
The main cause of retinal dystrophy is natural wear and tear of the organs of vision and age-related changes in the body. But this phenomenon is not at all necessary in old age; not all older people develop dystrophy of the visual organs. The risk group includes:
- those suffering from diabetes mellitus, kidney and adrenal dysfunction;
- hypertensive patients;
- patients diagnosed with high and moderate myopia - in this case, the retina overstretches, becomes thinner in certain areas and ultimately ruptures;
- people prone to vascular diseases;
- victims of severe intoxication.
It has already been proven that dystrophic changes in the retina are caused by genetic predisposition and can be inherited. For this reason, children of parents who have been diagnosed with such a pathology should especially carefully monitor the condition of their visual organs.
This is interesting: according to research, atrophic changes in the retina are more common in females with fair skin and blue irises. Moreover, the symptoms of dystrophy often begin to express themselves clearly during pregnancy in women.
Thinning of the retina - what is it, how does it manifest itself?
Thinning of the retina is a complication of myopia. But this is not the only disease that ultimately provokes dystrophy. In the process of myopia, anatomical and physiological changes in the eye occur. At the same time, the eye increases in length and its membranes stretch and become thinner inside at the periphery. All this reduces blood circulation in the eye and disrupts the trophism of the periocular tissues. The retina does not receive the required amount of nutrients and oxygen, as a result of which peripheral dystrophies of the retina itself occur.
Retinal thinning is not the most dangerous thing that can happen. Breaks in this area are truly an irreversible pathology that leads to the most severe ophthalmological disease - retinal detachment. Unfortunately, it is impossible to identify and cure this in the first stages. There are no symptoms in the initial period, and the patient feels well. Vision does not immediately deteriorate. When a detachment occurs, vision is lost suddenly and, often, irrevocably.
Retinal dystrophy is diagnosed not only in people suffering from myopia. There is a risk group of people who need to take care of the prevention of pathology.
Causes
Experts divide the causes of retinal thinning into two categories: local and general. So, the following reasons fall into the general category:
- chronic hypertension;
- uncontrolled diabetes mellitus;
- eye infections;
- complications as a result of the flu;
- diseases of the renal system.
The local category includes mechanical damage to the visual organs, myopia and inflammatory diseases.
A very important nuance is that the disease is hereditary. If there is a person in the family with this diagnosis, then the rest of the family members are recommended to visit the ophthalmologist’s office as often as possible for timely diagnosis.
Causes
Retinal thinning can develop for many reasons. Since the mechanism of occurrence of the disease is associated with various factors, experts identify several groups of phenomena that provoke it:
- Vascular changes
. Even a well-formed and adequately loaded retina undergoes thinning due to a lack of nutrients and oxygen. They reach it through the choroid of the fundus of the eye. If the local circulatory network does not function well enough, over time the rate of death of retina cells exceeds the rate of their renewal. The result of the process is thinning of the retina. - Metabolic changes
. The framework of the retina is collagen, which is also the connecting element between the choroid of the eyeball and the retina. When metabolic processes are disrupted or collagen synthesis pathologies in the body, the base of the retina becomes thinner. - Systemic diseases
- hypertension, atherosclerosis and diabetes mellitus. These ailments lead to a gradual weakening and destruction of the vascular walls, impaired patency, as a result of which the retina does not receive enough nutrients and becomes thinner. - Ophthalmic infections
. Not the most common cause of retinal thinning, as it might seem at first glance. Disturbances in retinal nutrition due to infectious and post-infectious changes are possible only when the pathological process moves to the intraocular membranes. Most often this happens with tuberculosis or herpes infection, as well as with the penetration of pathogenic flora (streptococci, staphylococci, Pseudomonas aeruginosa) through open wounds on the cornea. - Complications of viral infections
(influenza), which affect the vascular system of the eyes. - Kidney disease
, when the body increases the level of compounds that negatively affect the condition of the smallest vessels, including in the inner lining of the eye. - Mechanical damage to the inner membranes of the eye
due to injury or surgery.
Ophthalmologists also identify a congenital form of thinning of the retina. In this case, the fetus initially develops a retina of insufficient thickness. Visual impairment in this case is observed from the very birth of the child, and as the child grows, vision is completely lost.
Important! The only way to recognize a vision problem in a timely manner is to have your vision checked regularly. If a person is at risk, it is recommended that he visit an ophthalmologist twice a year, and for others - annually.
Subtypes of the disease
The disease is divided into two subtypes: acquired and hereditary. In the hereditary form of the disease, experts distinguish two main types:
- Pigmented - as a result of a malfunction of certain receptors, twilight vision is impaired.
- Dotted white – the disease manifests itself in childhood and has a slow development.
This disease is the most common cause of visual impairment in old age. The acquired type of disease is often associated with the aging of the body, since the development of the disease is observed only in people who have reached old age. In most cases, the disease is accompanied by the appearance of cataracts. The acquired type of disease is divided into:
- Peripheral thinning of the retina is a pathology that results in impaired quality of vision. In most cases, the occurrence of the disease is associated with trauma or inflammation of the organs of vision.
- Central retinal thinning is a process that results in the loss of central vision.
The central type of the disease has two pronounced forms:
- Wet - with this form of pathology, the functioning of the vascular system of the eyeball is disrupted, as a result of which the fluid circulating in the vessels begins to accumulate under the retina.
- Dry - with this form of the disease, in the gap between the vascular system and the retina, there is an accumulation of products formed as a result of the breakdown of nutrients.
Types of pathology
Retinal dystrophy can be central or peripheral. In order to begin treatment, it is important to determine the type of pathology.
- Central - vision decreases and it is difficult for a person to read, write, or drive a car.
- Peripheral - there are no symptoms, the disease is difficult to diagnose. Peripheral vision is affected. Then “floaters before the eyes” and “sparks in the eyes” appear.
If we are talking about hereditary pathology, pigmentation or a dotted white form of the disease may be observed at birth. Destruction of the retina in this case is diagnosed in childhood.
Main symptoms
If a person has a thinned retina, then he experiences the following clinical signs:
Redness of the organs of vision and dryness of the mucous membrane may be symptoms of the development of pathology.
- presence of black spots before the eyes;
- photophobia;
- lacrimation;
- headache;
- pressing sensations in the eye sockets;
- disturbance of general well-being;
- difficulty working with small objects and reading;
- inability to distinguish colors;
- sharp deterioration of vision in the dark;
- distortion of the shape of objects;
- redness and dryness of the eye mucosa.
Symptoms
Different types of the disease have their own distinct symptoms. Thus, with the peripheral form of retinal thinning, the initial stage of the disease occurs without certain pain or visual defects. The first symptoms may appear only at the stage of retina rupture. Very often, patients at this stage complain of bright flashes of light and the appearance of black spots in front of their eyes.
The wet form of the disease leads to visual distortion of the shapes of observed objects. The visual field can be significantly narrowed, which leads to the fact that some areas simply fall out of the visual field.
The risk group includes people suffering from myopia, as well as those who have vascular diseases, diabetes, hypertension
The following signs should be considered common symptoms of the disease:
- decreased visual acuity;
- difficulty navigating in a poorly lit room;
- impaired “twilight” vision;
- problems with color perception;
- the appearance of veil and cloudiness.
Signs by which thinning can be recognized
Please note that the initial stage of the peripheral form of the disease occurs without pain and visual defects. Primary symptoms may appear only at the stage of retinal rupture. Patients who are at this stage begin to complain of bright flashes of light or black spots appearing before their eyes.
The wet form of thinning can lead to distorted visibility of objects. Due to the strong narrowing of the visible field, some areas become invisible to humans at all. There are common symptoms of the disease. These include the following signs:
- the appearance of a veil before the eyes;
- impairment of the so-called “twilight” vision;
- decrease and drop in perceptual acuity.
Also, symptoms of the disease include poor perception of the color palette and difficulty in orienting the area in poor lighting.
What zones does the retina divide into?
The retina of the eye is divided into two main areas:
- The central zone (other names: macula, macula) is the main part of the retina, on which the quality of human vision depends by 90%. Its function is to provide subject and color perception of the surrounding world. A larger number of cones are concentrated here, which are responsible for the perception of color diversity. This is why any pathological changes cause major vision problems.
- Peripheral zone. Rods are located here - receptors that provide peripheral, spatial and twilight vision. If pathology occurs in this area, then the field of vision narrows significantly, and some areas disappear.
Treatment
The prescribed treatment is directly influenced by the degree of development of the pathology and its type. Unfortunately, in advanced cases of the disease, it is not possible to restore the original quality of vision. To treat the disease in its onset stages, medications with vasodilating properties are used. In addition, vitamin complexes and drugs that strengthen the body’s vascular system are prescribed. Very often, specialists allow the possibility of using physical treatment methods. Such techniques include:
- therapy using microwaves and ultrasound;
- laser therapy;
- influence using electrical impulses.
Today, laser therapy is one of the best measures for the prevention of diseases of the visual organs. This method is used when patients cannot undergo surgery.
The tendency to thin the retina is inherited
Thinning of the retina: causes and treatment, symptoms and prevention
The retina of the eye has a complex structure and performs important functions. Its main function is to provide central and peripheral vision. Also, thanks to the proper functioning of the retina, a person is able to: distinguish colors and shades, navigate in space, see at a distance (close, medium and far). Any pathological disorders lead to deterioration of vision.
Thinning (dystrophy) of the retina is a pathological condition (degenerative) that occurs under the influence of various ophthalmological diseases and leads to complete loss of vision. Vision deterioration sometimes occurs abruptly; there are often no obvious symptoms at the initial stage. The disease leads to the death of eyeball tissue and this process is irreversible.
Who most often experiences this defect?
This disease can develop in people of different age categories, but older people are more likely to suffer from it. This is due to the natural aging of the body. In some cases, heredity plays a decisive role. Children with a predisposition to certain ophthalmological diseases are regularly examined by an ophthalmologist.
People who are also at risk:
- overweight women and men (obese);
- people diagnosed with myopia, hypertension and diabetes;
- women and men who have bad habits and lead an unhealthy lifestyle;
- people working in unfavorable (harmful) conditions;
- people with light eyes and skin.
According to statistics, dystrophy occurs more often in women than in men. This is due to the fact that representatives of the fairer sex undergo hormonal changes in the body during pregnancy and lactation and weakened immunity.
Classification of pathology
There are several classifications of this disease. By type, pathology is classified into:
- age-related (develops under the influence of natural aging of the body);
- peripheral (more often occurs in people with myopia, is asymptomatic and can lead to retinal detachment);
- pigmentary (caused by genetic mutations, leading to impaired twilight vision and complete loss of vision);
- central (the ability to see details close up is lost: it is difficult to read, write, do handicrafts and drive a vehicle).
The disease is also divided into 2 types:
- Primary (congenital). This type of dystrophy is inherited and manifests itself in childhood.
- Secondary (acquired). It develops against the background of exposure to negative factors and natural aging of the body.
Treatment for thinning retina
Treatment of retinal dystrophy is carried out using various methods: drug treatment, physiotherapy, surgery. Often people turn to alternative medicine.
The main purposes of using drugs for thinning of the retina:
- prevent thrombosis;
- prevent the development of hypoxia;
- reduce the growth of blood vessels (abnormal);
- reduce vascular permeability.
For these purposes, drugs such as antiplatelet agents, angioprotectors, polypeptides, vitamin complexes (vitamins A, B and E are effective), vasodilators, etc. can be prescribed.
Treatment of such a complex and dangerous disease should be carried out exclusively by a specialist. Self-medication and ignoring the disease can lead to serious consequences.
At the initial stage of the disease, in addition to drug therapy, a therapeutic effect can also be obtained from the following types of physiotherapy:
- retinal stimulation (electrical and photo);
- magnetic therapy;
- electrophoresis;
- irradiation of blood with laser (intravenously).
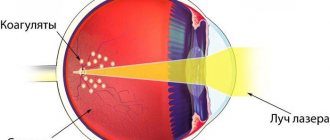
The most effective method today is laser coagulation of the retina. The operation is performed on an outpatient basis under local anesthesia. Has a number of significant advantages:
- short duration of the procedure;
- short recovery period;
- efficiency;
- relative safety.
In some cases, other types of surgical intervention (including vitrectomy) are prescribed.
Treatment of retinal dystrophy with traditional methods at the initial stage is also possible, but as an auxiliary therapy and only with the prescription (permission) of a specialist.
Various decoctions are used for this:
- from goat milk and water;
- from pine needles, rose hips and onion peels;
- from celandine and water (purified).
It is also believed that hirudotherapy (treatment with leeches) has a certain effect. Their bite helps relieve inflammation, eliminate pain, increase immunity, cleanse toxins, and lower blood sugar and cholesterol levels.
Video from our doctor on the topic
In conclusion, it is worth recalling that retinal restoration is possible and there are several medical methods for this. The prescription of a particular treatment method occurs for certain indications. These include: the degree of retinal destruction, its causes, and the patient’s physical characteristics. It is also necessary to remember that at the first signs of deterioration in visual functions, especially after an eye injury, it is necessary to contact an ophthalmologist as quickly as possible. Only in this case can we talk about timely treatment, which should bring good results.
By contacting the Moscow Eye Clinic, each patient can be sure that some of the best Russian specialists will be responsible for the results of treatment. The high reputation of the clinic and thousands of grateful patients will certainly add to your confidence in the right choice. The most modern equipment for the diagnosis and treatment of eye diseases and an individual approach to the problems of each patient are a guarantee of high treatment results at the Moscow Eye Clinic. We provide diagnostics and treatment for children over 4 years of age and adults.
{loadposition doc-vitamin}
You can find out the cost of a particular procedure or make an appointment at the Moscow Eye Clinic by calling 8 (800) 777-38-81 (daily from 9:00 to 21:00, free for mobile phones and regions of the Russian Federation) or using the form online entries.
Yakovleva Yulia Valerievna
Treatment of wet retinal thinning
In the treatment of this type of pathology, a large complex of medications is used. An ophthalmologist prescribes medications with antispasmodic effects, angioprotectors, antiplatelet agents and courses of vitamin therapy. This course of drugs is aimed at stopping the progression of the disease. Treatment of thinning of the retina with medications must be carried out at intervals of up to six months. The regularity of taking such courses directly determines whether it will be possible to stop the development of the disease. When the disease is severe or diagnosed at a late stage, specialists prescribe the following physiotherapy:
- exposure to areas of the retina using a magnet;
- stimulation of individual areas of the retina with electrical impulses;
- laser coagulation;
- photostimulation of the retina;
- irradiation of blood using a laser;
- surgical intervention.
These methods, as well as drug treatment, must be used at least twice a year. Only a competent specialist can determine the necessary treatment tactics, based on the collection of anamnesis data.
In the wet form of the disease, first of all it is necessary to carry out a laser therapy procedure to stop the formation of defective vessels. During such a micro-operation, a laser beam affects the affected areas and clogging of certain parts of the vascular system occurs. As a result of this effect, the liquid does not reach the affected areas of the vessels. This reduces the enormous risk of retinal detachment.
The laser coagulation procedure is a bloodless technique that does not cause pain. It can be carried out both in a hospital setting and on an outpatient basis. The duration of such an operation is about half an hour.
After the operation, the patient is prescribed a course of medications aimed at inhibiting the growth of the vascular system. This treatment is prescribed to stop pathological neoplasms that can cause the disease to develop in new areas.
Depending on the location of the lesion, dystrophy can be central or peripheral
Treatment of pathology
To eliminate the cause of the disease, medications are prescribed that help relieve inflammation and improve the condition of the retina.
Therapy for degenerative changes in the macula is aimed at eliminating the main cause that caused the development of the pathology. Features of pathogenetic therapy depend on the form of the disease. Drug treatment consists of prescribing angioprotectors, vasodilators, antioxidants and corticosteroids, which help reduce the severity of inflammation and improve the condition of the vascular wall of the macular arteries. For retinal edema, diuretics and biogenic stimulants are used. “Tauron” and “Emoxipin” will help strengthen trophic processes in the tissues of the eye.
Vitamin and mineral complexes with lutein and zeaxanthin will be useful. You can use photodynamic therapy and injections of substances that inhibit retinal dystrophy, which are made directly into the eyeball. If therapeutic methods are ineffective, surgical interventions with reconstruction of the vascular bed are used. If there is a threat of retinal detachment, laser coagulation of the choroid plexuses and adhesion of the macula to the underlying tissues must be done.
When the cause of dystrophy is hereditary, it is impossible to cure it.
Other symptoms of retinal detachment due to myopia
In this article
Myopia is not only changes in the fundus of the eye, it is also the thinning of the retinal pigment epithelium and the accompanying degenerative changes. Among the first changes are redistribution of pigment and blanching of the optic nerve head. Atrophy then occurs either around the disc or on one side of it.
Further changes appear on the temporal side of the disc in the shape of a crescent. The size of these changes corresponds to the area of thinning of the retina. Moreover, the progression of myopia is accompanied by further stretching of the fundus, a decrease in blood supply to the choroid and an increase in chorioretinal degeneration.
There are many types of diseases, as well as the causes of their occurrence. One of them is myopia.
Retinal detachment can occur in anyone, and patients with high myopia are at particular risk. With high myopia, a large eyeball provokes stretching of the retina and disruption of its nutrition. The latter causes a deterioration in metabolic processes in tissues and blood circulation, which causes hypoxia and retinal dystrophy.
There is peripheral and central chorioretinal dystrophy. In the most serious case, a “dry” or “wet” lesion of the macular region of the retina occurs. This significantly impairs vision and even leads to blindness. If the adverse changes in the retina are severe, the patient is diagnosed with myopic disease.
Myopic disease occurs quite rarely. As a rule, high myopia remains a harmless pathological change in refraction.
Timely preventive measures significantly reduce the risk of retinal detachment due to myopia or any other disease.
As mentioned above, the main preventive measure is laser coagulation. This is a fairly simple and not painful procedure, but if the eyes are very sensitive, pain may still occur. In this case, factors such as:
- volume of coagulation and zones of its implementation;
- model of laser equipment;
- features of the anatomy of the palpebral fissure;
- correct choice of contact lens;
- surgeon experience.
If the patient knows that the pain threshold is low or that he is uncomfortable during the procedure, it is better to warn the doctor about this in advance. The pain can be reduced with the help of special medications and then the procedure will take place without any difficulties.
Another symptom of retinal detachment is “morning improvement” - a sign in which a person, after a long period of inactivity, becomes able to see well: the veil fades or decreases. By lunchtime the patient's condition worsens, and by evening everything reaches its peak.
If the retinal tear is in the upper parts of the eye, then due to the descending fluid, retinal detachment occurs very quickly in myopia. If the gap is at the bottom, then the detachment slowly rises and occurs less rapidly, but the scars will be more pronounced, since there will be much more time for their occurrence.
To prevent retinal detachment due to myopia and other diseases of the visual organs, you need to regularly visit an ophthalmologist and carefully follow all his recommendations.
Retinal diseases
0
The retina of the eye plays one of the most important roles in visual perception of the environment. This component is the inner sensory layer of the eye, which performs the function of receiving light and color signals and then delivering them through the optic nerve to the brain.
The retina is one of the most complex structures of the visual organ. It is responsible for projecting images and transmitting them in the form of electrical impulses through the optic nerve to the brain. Therefore, any diseases of the retina lead primarily to deterioration of vision. To preserve visual ability and avoid radical measures to restore it, it is important to promptly identify diseases and treat them at an early stage. But today there are about ten pathologies of the retina: how to distinguish them from each other?
Currently, medicine already knows many different pathologies of the retina. The most dangerous and common of all these ailments is retinal detachment. The level of development of modern medicine, fortunately, makes it possible to successfully combat this disease.
Types of diseases
There are 3 groups of diseases that can affect the retina of the eye:
- Dystrophic. These pathologies can be congenital or acquired and are associated with structural changes in the photosensitive membrane.
- Vascular. Most often, such retinal diseases develop against the background of existing pathologies that affect the circulatory system. For example, iridocyclitis.
- Inflammatory. When there is an infectious lesion of the visual apparatus, the retina is sometimes involved in the inflammatory process.
Here is a list of the most common diseases that affect the retina of the eyes:
Angiopathy
One of the common diseases of the retina is angiopathy. This is a pathology that affects the vascular network of the membrane and develops when:
- Diabetes.
- Hypertension.
- Hypotension.
- Injury to the cervical spine, brain or chest.
This disease applies to all age groups of people, but people over 30 years of age are at risk.
Hemorrhage
Minor hemorrhages in the sclera occur in many people. This is harmless to your eyesight and does not require seeing a doctor. But when blood accumulations form in the retina, there is a reason to seek medical help. Retinal hemorrhage usually occurs against the background of injuries that differ in severity:
- Easy. There is no external damage to the eye, vision will be restored.
- Average. There is damage to the retina of the eye, and visual ability is reduced.
- Heavy. The structure of the visual organ is irreversibly damaged; restoration of vision, even partially, is most likely not possible.
Hemorrhage into the sclera
Treatment for hemorrhage in the eye consists of stopping the bleeding and eliminating the cause that caused it. A radical measure is vitrectomy. This operation is to remove clouded parts of the vitreous and blood accumulations from the retina.
Retinal tear
A retinal tear is associated with a violation of the integrity of the photosensitive membrane. As a result, this can lead to its complete detachment. The following types of rupture are distinguished:
- Holey. It occurs against the background of thinning of areas of the retina in the periphery against the background of peripheral dystrophy. Typically, the causes of such a rupture are dystrophy in the form of a cochlear mark on the retina or lattice.
- Valve. The rupture occurs against the background of fusion of the membrane with the vitreous mass.
- Macular. Observed in the central vision area. Occurs against the background of fusion of the macular zone of the retina with the vitreous body.
- Serrated. Sometimes the retina tears along the dentate line. This occurs against the background of severe concussions and injuries.
Retina rupture without the beginning of detachment of the membrane is treated by laser coagulation. Sometimes they resort to vitrectomy.
Macular edema
Swelling of the retina in the central area is called macular edema - part of the retina of the eye, about 0.5 cm in diameter. Macular edema develops against the background of:
- Thrombosis of the central vein of the retina.
- Chronic vascular inflammation.
- Retinal cancer.
- Diabetic retinopathy.
- Partial retinal detachment.
- Toxic damage to the visual apparatus.
- Ritinitis.
With macular edema, restoration of vision can take from 2 months to one and a half years.
Retinal detachment
This retinal pathology is caused by retinal tears. The detached part of the photosensitive shell ceases to receive nutrition, which leads to disruption of the photoreceptors. Fluid accumulates in the resulting pockets, causing blurred vision and continued retinal detachment.
According to the classification, retinal detachment is:
- Rhegmatogenous (rupture and detachment due to thinning of the retina).
- Traction (against the background of retina tension from the vitreous body during the formation of new vessels or fibrous tissue).
- Exudative (occurs against the background of infectious diseases of the visual analyzer, neoplasms in the choroid or retina).
- Traumatic (the retina can peel off immediately after injury or after several months or even years after an eye injury).
Restoring visual ability is more effective if you seek medical help immediately after symptoms of retinal detachment appear.
Retinal dystrophy
Retinal dystrophy is a degenerative irreversible process occurring in the retina. The disease progresses slowly, but leads to deterioration of vision, but vision loss is rare. Elderly people, in whom dystrophy is one of the common causes of visual impairment, are more susceptible to pathology.
The following types of dystrophy are distinguished:
- Central (the middle part of the retina is affected, central vision is impaired)
- Peripheral (changes affect only the peripheral parts of the membrane, only lateral vision is affected).
The progress of retinal dystrophy can be stopped, but vision cannot be restored after it has been impaired due to degenerative processes.
Diagnostic methods
To identify retinal diseases in a patient, it is necessary to go through the following procedures:
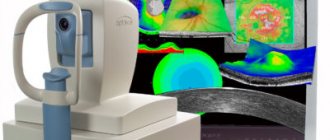
- Tonometry – measurement of IOP (intraocular pressure).
- Visometry is a study of the level of visual acuity, which allows one to determine the condition of the affected area and vital central areas.
- Electrophysiological examination of the eye (EPI) - assessment of the viability of retinal and optic nerve cells.
- Computer perimetry is an examination of visual fields to determine the condition of the peripheral areas of the retina.
- Ophthalmoscopy is an examination of the fundus of the eye, which allows one to determine the lesions of the retina, the location and number of breaks. In addition, in the presence of detached areas of the retina.
- Ophthalmoscopy makes it possible to assess their condition, the strength of their connection with the vitreous body, and also identify areas that require increased attention during treatment.
- Optical coherence tomography.
- Amsler test for checking the central visual area.
- Computed tomography of the eye.
- Ultrasound.
- MRI.
The procedures are prescribed by a specialist, so the patient does not have to undergo this entire complex.
Prevention
Preventive measures for retinal diseases differ slightly depending on the type of disease, but in general they are very similar. The most important principles of successful preventive activities are a healthy lifestyle, proper and fully balanced nutrition and the obligatory abandonment of bad habits.
What is eyeball nystagmus?
Tetracycline ointment: instructions for use for the eyes are described in this article.
Xalak eye drops with instructions https://eyesdocs.ru/medicinaoperacii/lekarstva/ksalakom-ot-chego-prednaznacheny-dannye-glaznye-kapli-i-kakova-instrukciya-po-ix-korrektnomu-primeneniyu.html
Video
conclusions
It is very important to know and understand that timely consultation with a doctor (at the first symptoms) and, as a result, receiving qualified medical care will help to avoid the development of serious complications. After all, retinal diseases can often cause irreversible harm to health and a person can lose his sight forever.
Also read about what diseases are caused by putrid discharge from the eyes and diplopia.
A working method to restore vision! You will throw your glasses in the trash in just 3 days...
Restoring vision. Real life story.
Laser coagulation
The laser treatment technique is used for almost all diseases associated with the visual organs. A huge amount of energy concentrated in a laser beam effectively affects areas affected by the disease. The concentration of laser beams in a specific area ensures that healthy areas of the retina are not affected during the operation. There are several specific laser treatment techniques and their use depends directly on the form of the disease.
One of these effects is laser stimulation of damaged areas. As a result of such intervention, in areas with thinning retina, abundant metabolic processes are activated. Exposure to laser beams has a beneficial effect and slows down the progression of the disease for many years to come.
Another example of laser surgery is the process of vascular coagulation. The essence of this effect lies in the need to separate vessels with a damaged structure from healthy ones. The laser beam affects the affected areas, where coagulants (adhesions) are formed as a result of protein breakdown. Such adhesions will protect pathological vessels from fluid penetration into them. As a result of the operation, an isolated network of the vascular system is created, through which nutrients do not circulate. This approach makes it possible to completely stop the progression of the disease, but this intervention does not protect against pathology occurring in other areas of the retina.
Surgical methods
Surgery may be required for severe retinal thinning. When the disease is in an advanced stage, treatment with medications and laser therapy does not bring a positive result. There are several types of surgical interventions, which can be divided into two conditional subgroups:
- Revascularization surgery is an intervention, as a result of which the surgeon removes abnormal neoplasms, and the vascular system, which has a normal structure, is opened;
- Vaso-reconstructive surgery - during such an operation, the surgeon installs special implants in order to normalize the microvascular bed of the eyeball.
Any surgical intervention should be carried out in a hospital, by specialists with extensive experience in such operations.
Typically, retinal thinning is caused by changes in the vascular system of the eyeball.
Diagnosis and treatment
Diagnosis is not always simple due to the age of the patients and the presence of concomitant eye diseases - cataracts, glaucoma. Ophthalmoscopy, fundus examination, and ultrasound examination are used.
Age-related changes in the retina are irreversible. Treatment is aimed at slowing down the processes of retinal degeneration and compensating for the affected functions of the eye.
With timely and early initiation of treatment, it is possible to achieve stabilization of the process and reduce changes in vision. In advanced cases, the function of the central parts of the retina completely disappears and the patient is left with only peripheral vision.
Drugs that improve blood supply to the eye, physiotherapeutic and laser procedures, and electrical stimulation are used. For local detachment and ruptures, laser cauterization of part of the retina of the eye is used.
The Medicine 24/7 Clinic provides complex therapy for age-related retinal diseases using innovative techniques tested in clinical studies, which allows, in uncomplicated cases, to return even forgotten sensations to the eyes. Sign up for a consultation
Diagnostics
You can suspect that the retina is discharged and the number of light-sensitive cells on it has decreased if the patient has a clinical picture characteristic of this disease. To confirm the diagnosis, an ophthalmoscopic examination of the fundus is performed. To better identify structural abnormalities of the macula, the pupil can be pre-dilated. An ultrasound examination of the eyeball and its optical tomography are also performed. To identify abnormalities in the structure of blood vessels, angiography is performed, where an abnormal arrangement of blood vessels is detected, which means the wet form of macular degeneration. You can measure intraocular pressure and study the visual fields. It is also necessary to undergo a general and biochemical blood test.
Existing methods of treating the disease
In the ophthalmologist's office, the patient can learn the causes and treatment of this disease. The type and degree of its development depends on the specific treatment option for retinal thinning. In advanced cases, it will not be possible to restore good vision. If the disease has just arisen, then medications and vitamins are prescribed, with the help of which you can strengthen the blood vessels. Also, physical treatment methods such as:
- Application of microwaves and ultrasound. Intravital measurements in the eyeball and its anatomical and optical elements are diagnosed. Ultrasound is prescribed as a complement to generally accepted clinical methods for diagnostic measures in ophthalmology. Sometimes an ultrasound is preceded by an x-ray of the eye.
- Use of laser, magnet. This method is considered relatively new in ophthalmology. Thanks to this method, you can get rid of the problem of poor vision once and for all and restore your vision to 100%.
- Effect of electrical impulse. Galvanization is effective; the method is used to increase or decrease the functions of eye tissues. The pain-relieving method is especially suitable after a person has suffered injuries related to the organs of the visual system.
As for preventive measures, these include special exercises for the eyes, a healthy diet, as well as an annual examination at the clinic. At the initial stage of the disease, it is necessary to drink a vitamin complex. Vitamins A, E and B can normalize vision, improve blood flow and fill the body with useful substances.
Medicines that are recommended for the treatment of thinning of the retina are prescribed exclusively by a doctor: No-spa, Retinalamin, Ascorutin, Methionine, Pentoxifylline, Lucentis. During pregnancy, many medications are prohibited, so you should not self-medicate.
Comprehensive treatment, which includes taking vitamins, medications, exercises, etc. It is recommended to use at least 2 times a year. Therefore, if the disease is severe or you were diagnosed too late, you may even be prescribed surgical intervention - be prepared for such an outcome.
Important! The peripheral type of the disease is treated first with laser and then with physical procedures and medications. You need to stop smoking and wear UV protective eyepieces.
You may be interested in: Which drops are best to choose to strengthen the retina?
A course of vitamins for thinning of the retina
When a patient is diagnosed with the initial stage of thinning of the retina, an ophthalmologist may prescribe a course of vitamins. Vitamins of groups “A”, “B” and “E” have the ability to normalize visual processes, improve blood circulation and nutrients in the body. This vitamin group improves the nutritional processes of eye tissues, and with a long course, stops the progression of the disease.
Vitamins from these groups should be taken in three specific forms:
- The first form is special vitamin complexes that come in tablet or injection form.
- The second form is vitamin supplements.
- The third form is food products containing the listed groups of vitamins.
These foods include leafy vegetables, cereals, fresh berries and fruits. These products are vital for people at risk to take. A properly balanced diet is the key to health and longevity of the whole body. Facebook
What is the retina
My example will probably be somewhat culinary, but I think this is a very suitable analogy. Let's say you decide to make jelly. To do this, you will need a deep round bowl - a mold, cling film, it is usually used to make it easier to remove the jelly from the mold and, accordingly, the jelly itself in a liquid state. This example is purely schematic, but the following can be understood from it. The eyeball resembles a cup in our example, that is, the inner part of the sclera, which figuratively “holds” our eye, the cling film is the same retina - just as thin, but very fragile, and the jelly is the vitreous body, which really resembles jelly or jelly and, in turn, makes our eye elastic.
So, if the film is slightly torn in some place, then the uncured jelly will begin to leak under the film. In cooking this is an aesthetic defect, but in ophthalmology it is catastrophic. Why? Gradually, through the existing gap, liquid will leak under the rest of the film, that is, the retina, peeling it off from the choroid ( retinal vessels ). Gradually this whole process leads to blindness.