Description
Aphakia.
This is a pathological condition of the organ of vision, which is characterized by the absence of a lens in the eyeball. Clinically, the disease is manifested by decreased visual acuity, trembling of the iris, loss of the ability to accommodate and asthenopic complaints. Diagnosis of aphakia includes visometry, gonioscopy, biomicroscopy, ophthalmoscopy, refractometry and ultrasound examination of the eye. Conservative therapy consists of correcting aphakia using contact lenses and glasses. The tactics of surgical treatment boil down to implantation of an artificial lens (intraocular lens) into the aphakic eye.
What is pseudophakia of the eye, is it necessary and how to treat it. Aphakia code according to ICD 10
Pseudophakia eyes
Pseudophakia of the eye is a condition of the organ of vision in which an artificial lens was inserted due to indications. This type of correction is considered more acceptable than correction with glasses, since at the physiological level it eliminates the patient’s dependence on glasses without narrowing the field of vision, as happens with a removable vision accessory.
Pseudophakia does not produce peripheral scotoma, dark spots, or distortion of objects. The image is formed in the retinal area if an IOL is used, and in normal size. At the moment, many designs have been developed in which artificial lenses correct various deviations in vision, including glaucoma and cataracts.
Find out why retinal angiopathy occurs in a child and what can be done about such a disease in this material.
With some pathologies, if they are started and brought to the point of complete clouding of the natural, native lens, then blindness occurs. This condition can no longer be corrected by an IOL.
It will also be useful to learn about conducting and deciphering visometry.
Artifakia Code According to ICD
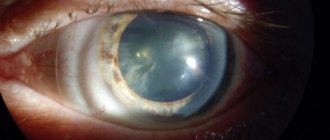
Cataract is a disease characterized by varying degrees of persistent opacities of the substance and/or capsule of the lens, which are accompanied by a progressive decrease in human visual acuity.
Causes of cataracts
Classification by etiology
Classification according to the degree of progression • Stationary (most often congenital, opacification does not change over time) • Progressive (almost always acquired, opacification of the lens increases over time).
Clinical picture
• General symptoms •• Painless progressive decrease in visual acuity •• Fog before the eyes, distortion of the shape of objects •• Ophthalmological examination reveals clouding of the lens of varying severity and localization.
Lens implantation: indications and features of the operation
In medical terminology, aphakia is the name given to an eye that lacks a lens. Intraocular correction of aphakia is a surgical operation to replace the natural lens with an artificial lens (implant).
Pseudophakia is the result of surgery to insert an implant. An eye with an implant is called pseudophakic.
Features and benefits of pseudophakia
Compared to other types of treatment, pseudophakia has clear preferences:
– the operation is safe (laser technology) and takes no more than 1 hour per eye;
– there is no cosmetic defect (the implant is completely transparent and similar to a natural lens);
– the visual field is completely preserved;
– there are no invisible areas in the field of view;
– there is no distortion of objects (typical for glasses);
– no need to wear glasses (or use contact lenses).
Additional facts
Aphakia, or absence of the lens, is an eye disease of congenital or acquired origin, which is accompanied by pathology of refraction, decreased visual acuity and inability to accommodate. Congenital aphakia is an orphan disease; the frequency of its development in the population has not been sufficiently studied. At the same time, the number of postoperative aphakia resulting from cataract extraction increases every year. The risk of developing an acquired form of the disease increases sharply after the age of 40. An increase in the number of acquired forms of the disease is predicted in economically prosperous countries. The development of both congenital and acquired forms of pathology is not affected by race and gender.
Causes
The clinical classification of aphakia includes congenital and acquired forms of the disease. In ophthalmology, there are two types of congenital aphakia: primary (caused by lens aplasia) and secondary (develops due to intrauterine resorption of the lens). Depending on the prevalence, the absence of a lens can be monocular (one-sided) or binocular (two-sided). A key role in the development of congenital aphakia is played by impaired development of the lens at the stage of embryogenesis. In the primary form of the congenital defect, the lens vesicle does not separate from the outer ectoderm. The PAX6 and BMP4 genes are normally responsible for this process. Depending on the degree of decrease in the expression of these genes at certain stages of embryonic development, the formation of anterior lenticonus, anterior capsular cataract and Peters anomaly combined with the absence of a lens is possible. It has been experimentally proven that a delay in the development of eyeball structures at the stage of corneal-lens contact leads to the primary form of congenital aphakia. The cause of the secondary form of the disease is idiopathic absorption of the lens, which occurs spontaneously. One of the theories of its development is considered to be a spontaneous mutation, which provokes a disruption in the formation of the basement membrane, from which the lens capsule should be formed during embryogenesis. In the etiology of acquired aphakia, the main role is played by surgical extraction of cataracts, dislocation and subluxation of the lens. Penetrating wounds and contusions of the eyeball can also be causes of this disease.
Treatment protocols
Clinical classification of PCRD 1. Lattice dystrophy - the most common cause of retinal detachment. A family-hereditary predisposition to this type of dystrophy is assumed to be more common in men. As a rule, it is found in both eyes. It is most often localized in the upper outer quadrant of the fundus, equatorially or anterior to the equator of the eye. When examining the fundus, lattice degeneration appears as a series of narrow white, fleecy stripes, forming figures resembling a lattice or a rope ladder. This is what obliterated retinal vessels look like. Between these altered vessels, pinkish-red areas of retinal thinning, cysts and retinal breaks appear. Characteristic changes in pigmentation in the form of darker or lighter spots, pigmentation along the vessels. The vitreous body is, as it were, fixed to the edges of the dystrophy, i.e. “tractions” are formed - cords that pull the retina and easily lead to ruptures. 2. Dystrophy of the “snail track” type . The retina shows whitish, slightly shiny, streak-like inclusions with many small thinning and perforated defects. Degenerative lesions merge and form ribbon-like zones, which in appearance resemble a snail's track. Most often located in the upper outer quadrant. As a result of such dystrophy, large, round shaped tears can form. 3. Frost-like dystrophy is a hereditary disease of the retinal periphery. Changes in the fundus are usually bilateral and symmetrical. On the periphery of the retina there are large yellowish-white inclusions in the form of “snow flakes”, which protrude above the surface of the retina and are usually located near thickened, partially obliterated vessels; there may be pigment spots. Frost degeneration progresses over a long period of time and does not result in ruptures as often as ethmoid degeneration and cochlear degeneration. 4. Cobblestone degeneration is usually located far in the periphery. Individual white lesions are visible, slightly elongated in shape, around which small lumps of pigment are sometimes identified. Most often found in the lower parts of the fundus, although they can be detected along the entire perimeter. 5. Cystoid (small cystic) retinal dystrophy is located at the extreme periphery of the fundus. Small cysts can merge to form larger ones. In case of falls or blunt injuries, cysts may rupture, which can lead to the formation of perforated ruptures. When examining the fundus, cysts appear as multiple round or oval bright red formations. 6. Retinoschisis - retinal separation - can be congenital or acquired. More often this is a hereditary pathology - a malformation of the retina. Congenital forms of retinoschisis include congenital retinal cysts, X-chromosomal juvenile retinoschisis, when patients, in addition to peripheral changes, often exhibit dystrophic processes in the central zone of the retina, leading to decreased vision. Acquired dystrophic retinoschisis most often occurs with myopia, as well as in old and senile age. 7. Mixed forms - a combination of different types of degenerations. Peripheral chorioretinal degenerations can lead to retinal breaks. Based on their type, retinal tears are divided into perforated, valvular, and dialysis-type. Perforated tears most often occur as a result of lattice and cystic dystrophies; the hole in the retina gapes. A rupture is called a valve rupture when a section of the retina covers the site of the rupture. Valvular tears are usually the result of vitreoretinal traction, which “pulls” the retina with it. When a tear forms, the area of vitreoretinal traction will be the apex of the valve. Dialysis is a linear tear of the retina along the dentate line - the site of attachment of the retina to the choroid. In most cases, dialysis is associated with blunt trauma to the eye. Tears in the fundus look like bright red, clearly defined foci of various shapes, through which the pattern of the choroid is visible. Retinal breaks are especially noticeable against the gray background of detachment.
Symptoms
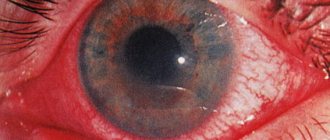
A specific symptom of aphakia is iridodonesis (trembling of the iris), which develops with eye movement. During examination, patients show a decrease in visual acuity and ability to accommodate. In terms of prognosis, the most unfavorable is the unilateral form of the disease, since the clinical picture is complicated by aniseikonia. The anomaly induced by organic pathology is accompanied by a difference in the size of the image on the retina, as a result of which binocular vision sharply deteriorates. The congenital form of the pathology is characterized by a progressive decrease in visual acuity with relative stability of other clinical manifestations. Lack of timely treatment can cause blindness. The postoperative form of aphakia is characterized by a staged course of the underlying disease, which was the reason for surgical intervention to remove the lens. The clinical picture of traumatic aphakia is characterized by a progressive increase in symptoms, the early manifestations of which are intense pain with an increase in local edema and a progressive decrease in visual acuity. Asthenopic complaints in patients with aphakia include the appearance of fog before the eyes, low ability to fixate, and double vision. Nonspecific manifestations of the disease are headache, general weakness, and increased irritability.
Diagnostics
To make a diagnosis of “aphakia,” it is advisable to carry out such research methods as visometry, gonioscopy, eye biomicroscopy, ophthalmoscopy, refractometry and ultrasound of the eye. Using visometry, it is possible to determine the degree of decrease in visual acuity. This research method is indicated for all patients before correction. Gonioscopy reveals a pronounced deepening of the anterior chamber of the eye. Carrying out ophthalmoscopy is necessary to identify concomitant pathologies and select further treatment tactics. In addition to scar changes in the retina and choroid, aphakia often reveals central chorioretinal dystrophy of the retina, partial atrophy of the optic nerve and peripheral chorioretinal lesions. The refractometry technique for the unilateral form of the disease allows us to detect a decrease in refraction by 9.0 - 12.0 diopters in the aphakic eye. Hypermetropia is determined in children after extraction of congenital cataracts and averages 10.0 – 13.0 diopters. The development of microphthalmos in congenital aphakia also contributes to farsightedness. The biomicroscopy method cannot visualize the optical section of the lens. In rare cases, capsule remains are detected. When examining Purkinje-Sanson figures, there is no reflection from the posterior and anterior surfaces of the lens.
Kinds
Since the disease is considered extremely common, doctors distinguish several classifications of the disease. The simplest classification is based on the origin of the disease, because there are two types:
- a disease caused by endogenous factors, that is, occurring against the background of other diseases;
- a problem that develops against the background of exogenous factors, that is, due to the negative influence of the external environment.
Iridocyclitis is also classified according to the degree of development of the disease and the reason for its occurrence.
Visual signs of the disease
Read how to use Indocollir eye drops correctly here.
Chronic variety
This form is characterized by peculiar symptoms
Which ones should you pay attention to:
- The state of health is gradually deteriorating.
- Swelling and inflammation may appear and disappear.
- The patient’s well-being changes depending on external factors (for example, when working at a computer for a long time, visual acuity may noticeably decrease).
- Eradicating the problem takes from one to three months.
Symptoms such as burning eyes, persistent discharge, pain and swelling develop gradually, but this does not mean that they should be ignored. If a person does not begin immediate treatment, his health will noticeably worsen.
Redness and lacrimation are the initial signs
A physiological feature or sign of disease is the cause of yellow eyes.
Acute and subacute form
The acute form of the disease develops according to a completely different scenario. Symptoms overtake a person immediately, and they develop so rapidly that within a week after infection it literally becomes painful for a person to open his eyes.
Often a visual examination of the patient is sufficient for diagnosis.
The average period of such iridocyclitis is 3-6 weeks. If a person ignores treatment for the acute stage of the disease, it can become chronic.
The patient is concerned about the following symptoms:
- change in iris color;
- redness and swelling of the eyes;
- severe pain in the eyes;
- constant release of tears and pus;
- possible bleeding from the eyes;
- noticeable decrease in visual acuity.
A drug for ophthalmological diagnosis and treatment of various problems – Atropine eye drops.
The acute form is characterized by rapid development
Fibrous-plastic
This form develops with penetrating eye injuries. Often, when this type of complication develops, a person develops adhesions on the back of the eye, which leads to its gradual fusion.
Symptoms do not develop abruptly, but if left untreated, there is a high probability of the disease progressing to the chronic stage.
Dangerous diseases that require timely treatment are optic nerve atrophy and congestive disc.
Fibrous appearance
Fighting herpes infection - instructions for using Zovirax eye ointment.
Depending on the cause of development
Another type of classification of iridocyclitis is based on the cause of the disease. Ophthalmologists identify a dozen problems that stimulate the gradual development of such a scourge, and each of them should be discussed separately.
- The disease often develops against the background of traumatic injury to the eye, due to serious contusion or injury.
- Iridocyclitis develops against the background of viral or bacterial diseases, such as measles, malaria, chlamydia, influenza, tuberculosis and others.
- Metabolic disorders or the development of diseases such as diabetes, gout.
- Rheumatoid conditions also stimulate the appearance of iridocyclitis.
- Infection with microbes or toxins when they come into direct contact with the iris stimulates inflammation.
- The problem may be directly related to an acute allergic reaction.
The method of treatment depends on the type of disease and the cause of its occurrence. Doctors urge you to always undergo diagnostics to find out why the problem arose.
An increase in intraocular pressure is characteristic of the initial and late stages of the disease
Drugs, the norm or a medical problem are the causes of constricted pupils.
Treatment
Aphakia is corrected using glasses, contact and intraocular lenses. The indication for spectacle vision correction is a bilateral form of the disease. For unilateral aphakia, glasses are recommended only if contact methods of correction are intolerant. The choice of glass for an emmetropic eye is difficult, because even glass of +10 diopters is not comparable to the refractive power of the lens, which is 19 diopters. This is due to the fact that the refractive index of the liquid that surrounds the lens is higher than that of the air surrounding the glass. The optical power of a glass lens depends on the patient's refraction. For hyperopia, it is necessary to choose glasses with stronger optics than for myopia. There is no need to prescribe vision correction methods to patients with high degrees of myopia before lens removal. Due to the lack of accommodation ability, the patient should be prescribed glasses for near vision that are 3.0 diopters stronger than for distance vision. Contact or intraocular vision correction is indicated for patients with monocular aphakia. Prescribing glasses to patients with this form of the disease will worsen aniseikonia. During surgery (intraocular correction), an artificial lens with individually selected optical power is implanted. The most preferred treatment option is the use of posterior chamber lenses, as they are localized at the location of the natural lens and provide high quality vision. Congenital aphakia can be corrected using this technique only after the child reaches two years of age.
Pseudophakia of the eye - what is it? Delivery of contact lenses and glasses in Moscow and Russia
An eye in which an intraocular lens (IOL) is installed is called pseudophakic. Often such operations are performed for cataracts. Often, IOL implantation is the only way to restore vision to a person in severe ophthalmopathologies. Let's find out how the procedure goes, whether there are contraindications to it and what complications there are.
Pseudophakia of the eye - what is it and how to treat it?
Actually, pseudophakia is not a disease, but the result of treatment for some ophthalmological disease, during which a special artificial lens is installed in the eye instead of the removed lens.
It is called an intraocular IOL. Also sometimes the process of implanting an IOL into the eyeball is called pseudophakia.
Such operations today are carried out using laser and ultrasound technologies; they are completely safe and rarely accompanied by complications.
In some cases, removing the lens and replacing it with an IOL becomes a real salvation for a patient who has lost visual function.
Indications for surgery
There are three main reasons that lead to the appointment of such a procedure:
- abnormal condition of the eye - absence of a transparent body or defects in it;
- the lens has already been removed during surgery;
- injury to the eyeball with damage or complete loss of the lens.
These are common reasons. In most cases, cataracts and aphakia lead to replacement of the corpus transparentum. Let's look at these pathologies in more detail.
Aphakia of the eye - what is it and how to treat it?
Aphakia is the absence of a lens. This pathological condition can be congenital, which is extremely rare, or acquired, caused by mechanical trauma to the eye or surgery.
Other varieties of this pathology are unilateral and bilateral. Aphakia of the left or right eye manifests itself in the same way. When only one eyeball is affected, binocular vision is impaired. Aphakia is also accompanied by:
- rapid decline in visual acuity;
- problems with focusing;
- impossibility of obtaining a uniform image.
During the examination, signs such as slight trembling of the iris and clouding of the pupil are observed. Vision is restored in aphakia by installing an intraocular lens into the lens capsule.
What is a cataract?
A cataract is a clouding of the lens. This disease develops mainly in old age and can lead to complete loss of vision. In the initial stages, the pathology is treated with medications. However, they only help to stop the clouding and eliminate some of the symptoms of cataracts.
These include:
- decreased visual acuity;
- diplopia;
- glare in low light;
- deterioration of twilight vision;
- increased photosensitivity;
- color vision disturbance;
- “flies” before the eyes;
- white and gray spots around the pupil;
- inability to select correction tools for refractive errors.
Cataracts can only be completely cured surgically, that is, by removing the clouded lens and then replacing it with an IOL.
How is the lens replaced?
The operation is performed on an outpatient basis. An anesthetic drug is instilled into the patient's eye, after which the procedure to remove the lens begins. Today there are two methods of treating cataracts:
1. Ultrasonic phacoemulsification. During this operation, a phacoemulsifier is inserted into the chamber of the eyeball after making a small incision on its surface. With its help, the contents of the transparent body are destroyed. The impact on the lens is ultrasound.
After this, the resulting emulsion is removed from the eye through a special pump. The posterior portion of the lens capsule is left in place. It becomes a barrier between the vitreous body and the iris. Next, the doctor polishes the capsule from the inside, removing any remaining tissue, and implants a rolled-up IOL into it.
Inside, it straightens out and takes the correct position. There is no need for stitches after surgery. Damaged tissues heal quickly. 2. Femtolaser phacoemulsification.
This operation is carried out according to exactly the same algorithm as the previous procedure, but instead of ultrasound, a laser is used, which turns the lens into a homogeneous emulsion.
Contraindications for surgery
The IOL implantation procedure is not performed in the following cases:
- development of an inflammatory process in the eye;
- small size of the anterior chamber of the eyeball;
- retinal disinsertion;
- small eye diameter, as with progressive farsightedness;
- suffered a stroke or heart attack in the last six months.
Some contraindications are relative, others are absolute. Before the operation, the patient undergoes a detailed examination.
What types of IOLs are there?
There are three main types of lenses - anterior chamber, pupillary and posterior chamber. The first ones are installed in the frontal part of the eyeball. Subsequently, the IOL may come into contact with the cornea and iris. Because of this, synechiae - adhesions - form in the corner of the anterior chamber. For this reason, anterior chamber lenses are rarely used.
The pupils are built into the pupil using the clip principle. The IOL is held in the chamber using special elements, anterior and posterior supports. The lens may become dislodged if there is minor trauma to the eye.
Today, the latter type of IOL is mainly used. The posterior chamber lens is inserted into the lens bag after its removal and fully performs the functions of a transparent body, providing high quality vision.
In addition, after implantation of such lenses, the risk of complications is reduced. The IOL contacts only the walls of the lens capsule, which does not have nerves or blood vessels.
In this regard, with pseudophakia there is no inflammation in the eye.
Lenses are made from hard and soft materials. Hydrogel IOLs are virtually indistinguishable from conventional contact optics for everyday use.
Depending on the type of pathology, the condition of the cornea, and the financial capabilities of the patient, the following types of lenses are used:
- Spherical and aspherical. The latter are more relevant, as they provide the highest contrast image and wide field of view. Additionally, aspherical lenses are free from glare.
- Monofocal and multifocal. The former do not completely imitate the lens. The latter guarantee normal focusing at different distances, since they have several optical zones. Multifocal IOLs correct presbyopia - “age-related farsightedness.” Toric lenses are also available to correct astigmatism.
- IOL with protective functions. These “artificial lenses” are the most expensive. But they protect the eyes from ultraviolet radiation. This type of lens is usually yellow or blue. This does not affect color perception in any way.
Pseudophakia of the right and left eyes
IOLs can also be placed in both eyeballs. This happens with bilateral aphakia, cataracts in both eyes, severe myopia or farsightedness, which are treated surgically. The operation is performed first on one eye.
The second is operated on only after a few months, that is, after the patient has fully recovered. Lens replacement is performed using minimally invasive methods, which ensures rapid tissue healing.
In some cases, treatment of the second eye is carried out already 2 months after the first procedure.
Consequences of lens replacement
Are there complications with pseudophakia? They rarely develop.
Their occurrence depends on the type and quality of the IOL, individual physiological characteristics, the condition of the eyes before surgery, the patient’s compliance with rehabilitation rules and other factors.
There are such complications:
- Secondary cataract. It occurs due to the proliferation of tissue remaining in the capsule.
- Glaucoma. Increased intraocular pressure may be a temporary side effect.
- Retinal detachment. The defect is eliminated during laser coagulation.
- Dislocation or loss of the lens with damage to the tissue of the eye, which most often occurs due to injury.
- The development of an infectious or inflammatory disease - iridocyclitis, keratitis, etc. The cause of such complications is a violation of hygiene rules during the recovery period.
- Formation of adhesions in the anterior chamber of the eyeball. Previously, such a defect was observed when installing anterior chamber IOLs.
- Protein deposits on the IOL. The lens is being cleaned.
Source: https://www.ochkov.net/informaciya/stati/artifakiya-glaza—chto-eto-takoe.htm