330
Retinopathy in diabetes mellitus, also called diabetic eye disease, is one of the main chronic complications of diabetes mellitus. Diabetic retinopathy is the leading cause of vision loss among the economically active population in developed countries. Vision complications are observed in 85% of patients with type 1 diabetes, and our city is no exception. You can undergo an initial examination and consultation in the city of Mariupol at city hospital No. 2 at an appointment with an endocrinologist, with a referral for examination to an ophthalmologist.
Let's look at the main symptoms, causes, treatment methods and prevention of this disease.
The main cause of retinopathy is damage to the small blood vessels of the eye that supply blood to the retina.
This complication occurs as a result of elevated blood sugar levels. Blood sugar acts as a toxin, damaging nerves and blood vessels. As a result, the blood vessels in the eyeball, retina and vitreous body are destroyed. An eye deprived of blood supply slowly deteriorates to the point of blindness. According to WHO, in 2020, diabetic retinopathy was the cause of blindness among 1.8 million people (4.8%) in the world.
The mechanism of development of diabetic retinopathy
The appearance of diabetic retinopathy is not affected by diabetes as such, but by hyperglycemia (high blood sugar) and strong jumps in this indicator.
Diabetic retinopathy can appear in patients with both type I and type II of the disease. Moreover, in patients with insulin-dependent diabetes, retinal damage occurs 2 times more often.
The eye pathology itself develops slowly - over 7-10 years, so it is necessary to identify the disease as early as possible and begin treatment.
1 Diabetic retinopathy: symptoms and treatment
2 Diabetic retinopathy: symptoms and treatment
3 Diabetic retinopathy: symptoms and treatment
Diagnostics
A thorough diagnostic examination can identify early symptoms of diabetic retinopathy. To assess the condition of the retina, determination of visual acuity, perimetry (examination of visual fields), ultrasound scanning, measurement of intraocular pressure, examination of the fundus, etc. are used.
Patients suffering from diabetes, regardless of the presence or absence of vision complaints, should be examined at least twice a year to prevent complications and preserve vision!
Causes of diabetic retinopathy
The occurrence of this disease is associated with increased permeability and damage to the blood vessels of the retina, blockage of capillaries, the growth of new (abnormal) vessels and, as a consequence, the appearance of scar (proliferative) tissue. One or both eyes may be affected (to varying degrees).
The main risk factors influencing the rate of development of the disease include the following factors:
- elevated blood sugar levels;
- arterial hypertension;
- genetic predisposition;
- long term diabetes mellitus;
- chronic renal failure;
- the patient is overweight;
- metabolic syndrome;
- smoking, etc.
Classification of diabetic retinopathy
The following stages of diabetic retinopathy are distinguished: non-proliferative , pre-proliferative and proliferative diabetic retinopathy .
Nonproliferative diabetic retinopathy is the initial manifestation of the pathology. The retinal vessels begin to expand, then thicken, their walls become permeable to the liquid part of the blood with dissolved proteins and fats.
The accumulation of fluid leads to swelling and hardening of the retina. In diabetes (especially type II), swelling of the center of the retina (macula), which is responsible for clear object vision, often occurs. Due to insufficient blood supply, retinal cell death begins. Damage to blood vessels leads to hemorrhages.
Preproliferative diabetic retinopathy is a further development of the disease. The damage to the retina increases, and entire lesions with dead cells appear (foci of soft exudates). And if treatment is not started at this stage, retinal detachment will follow, leading to a sharp deterioration in vision.
Proliferative diabetic retinopathy . A decrease in blood supply and destruction of retinal vessels lead to the fact that the body begins to produce new pathological vessels in different parts of the retina, including in the area of the visual spot. These vessels have very fragile walls, which provokes the appearance of new hemorrhages. Fibrous tissue and scars appear on the affected retina, and cords appear. This leads to retinal detachment and blindness.
Symptoms
The symptomatic range of diabetic retinopathy is not so extensive:
- feeling of discomfort in the eyes;
- general deterioration of visual acuity up to short-term periodic blindness;
- blood stains on the eyeball;
- feeling of a veil before the eyes, the appearance of black spots in the field of vision, inability to read and write.
Important!
If such signs appear, timely contact with an ophthalmologist and constant monitoring of blood sugar are necessary.
Diabetic retinopathy, in the absence of timely intervention, causes a number of complications:
- Increased intraocular pressure;
- Hemophthalmos due to which blood enters the lens;
- Blindness due to retinal detachment.
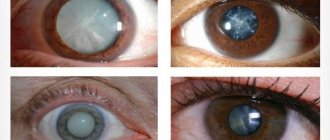
The pathogenesis of retinopathy can be traced in the photo:
Stages of the disease
- Non-proliferative stage: early stage of pathology development. The beginning of the processes of damage to the capillaries that supply the retina of both eyes. Small vessels are always destroyed first. Due to degenerative processes, the capillary walls become more permeable, which causes retinal edema to form.
- Preproliferative stage: this stage, if not intervened, can become a catalyst for irreversible transformations in the visual organ. Many pockets of hemorrhage and even entire areas of ocular ischemia appear, and fluid begins to accumulate in the eye. It is at the preproliferative stage that a significant lack of oxygen for the eyes begins.
- Proliferative stage: at this stage of development of the pathology, a massive expansion of the network of new blood vessels occurs, as the body tries to replace damaged pathways for the delivery of oxygen and nutrients. New vessels are formed weak, also unable to cope with their task; only generate new foci of hemorrhage. Due to blood entering the retina, the nerve fibers of the retina increase in volume, and the central zone of the inner shell of the eye (macula) swells.
- Terminal stage at which irreversible necrotic processes occur. At the described stage, hemorrhages into the lens are possible. Hemorrhages form many blood clots, which further load the retina, deforming it and initiating the process of retinal rejection. The prognosis at this stage is not comforting, since over time the lens loses the ability to focus light rays on the macula and the patient gradually loses visual acuity to the point of blindness.
There is also a classification of retinopathy according to the degree of damage to the retina:
- Mild: this type is characterized by microdamage to blood vessels. During ophthalmoscopy, they are defined as small red dots, the presence of which cannot be determined without equipment;
- Moderate: the number of microdamages increases, the volume of veins increases, signs of retinal hypoxia appear;
- Severe: microscopic hemorrhages form over the entire area of the retina. A significant part of the eye capillaries ceases to function. Immediate consultation with an ophthalmologist is required.
Symptoms of diabetic retinopathy
The insidiousness of diabetic retinopathy is that the disease occurs without noticeable symptoms.
It is necessary to pay attention to the following signs of eye pathology:
- the appearance of a veil;
- blurred image;
- the appearance of “flies” before the eyes;
- decreased visual acuity.
1 Diabetic retinopathy: symptoms and treatment
2 Diabetic retinopathy: symptoms and treatment
3 Diabetic retinopathy: symptoms and treatment
Diagnosis of diabetic retinopathy
To identify initial changes in the retina, every patient suffering from diabetic retinopathy must undergo regular examination by an ophthalmologist. This will help prevent the appearance of a proliferative form of the disease.
To identify pathology, the following diagnostic methods are used:
- eye perimetry;
- visometry;
- biomicroscopy;
- tonometry;
- ophthalmoscopy;
- examination of the fundus using a fundus camera;
- Ultrasound of the eye;
- electrophysiological studies;
- fluorescein angiography;
- laser scanning tomography of the retina.
What to do?
The cells of the inner lining of the eye are unable to regenerate, so the main goals of therapeutic therapy are to save intact macular cells and normalize blood sugar. An effective method of treating diabetic maculopathy is laser photocoagulation of the retina. It involves cauterizing the altered vessels of the organs of vision and creating new pathways for the outflow of fluid accumulated inside.
There is no drug treatment for diabetic maculopathy, since drugs are not able to treat and stop pathological processes in the retinal capillaries.
A clinical condition such as optical haze limits the use of laser in the treatment of diabetic maculopathy. For such pathologies, the following surgical treatment is used:
- Cryoretinopexy. The destruction of the inner membrane of the organs of vision is carried out by exposing it to cold, which leads to an improvement in metabolic processes and blood circulation in the retina.
- Vitrectomy. Pathologically altered tissues that cause tension in the eye shell are removed from the vitreous body of the organs of vision.
Damage to the macula area is a serious consequence of diabetes. Therapeutic therapy prevents further spread of the pathological process, but cannot completely restore visual acuity. Diabetics are recommended to undergo mandatory examination by an ophthalmologist twice a year. To prevent the development of diabetic maculopathy, it is necessary to stabilize blood glucose levels, prevent increased pressure in the arteries and restore lipid metabolism in the body. To slow down or ease the process of macular damage in diabetic maculopathy, it is recommended to take a course of vitamins or use dietary supplements.