Description
Retinopathy of prematurity.
Vasoproliferative damage to the retina caused by immaturity of the eye structures in children born prematurely. Retinopathy of prematurity is characterized by a disruption of normal vasculogenesis and often regresses spontaneously. In other cases, it is accompanied by opacification of the vitreous body, myopia, astigmatism, strabismus, cataracts, glaucoma, and tractional retinal detachment. Retinopathy is diagnosed during an examination of a premature baby by a pediatric ophthalmologist using ophthalmoscopy, ultrasound of the eye, electroretinography, and visual EP. Treatment of retinopathy of prematurity may include cryo- or laser photocoagulation of the retina, vitrectomy, and scleroplasty.
Additional facts
Retinopathy of prematurity is a disorder of retinal vascularization processes in children of low gestational age. The frequency of retinopathy of prematurity in neonatology and pediatric ophthalmology closely correlates with the degree of maturity of the child’s body: for example, in children weighing less than 1500 g, retinal pathology develops in 40-50% of cases; less than 1000 g – in 52-73%; and in very premature infants weighing less than 750 g - in 81-95% of cases. The paradox of the situation is that improving the conditions for caring for children with extremely low body weight leads to an increase in cases of retinopathy of prematurity, which in developed countries is becoming the leading cause of blindness in children.
Retinopathy of prematurity
Background retinopathy and retinal vascular changes
7
aafa.orgtoday at 15:37
Regular hand washing is the best way to prevent coronavirus infection and flu. But with hand eczema it turns into sheer torture. Dryness, cracking of the skin and the likelihood of infection. How can people with eczema protect their skin from coronavirus?
SkinSkin DiseasesChinese PneumoniaCoronavirusRash
20
MedVisors editors today at 15:14
Leukemia is a cancer of the blood or bone marrow that produces blood cells. The disease usually develops due to problems with the production of white blood cells, that is, leukocytes.
BleedingLeukemiaOncologyCancer
17
Editorial staff of MedVisoryesterday at 15:26
Children bitten by mosquitoes literally go crazy from severe itching. If a child scratches a mosquito bite until it bleeds, it’s time to disinfect the wound. And at the same time, make sure he doesn’t itch anymore.
SkinProteinChildInsect BitesBaby Care
6
Debra Rose Wilson, www.healthline.comyesterday at 2:44 pm
Since proper hygiene is critical to combating the spread of coronavirus, hand sanitizers have become very popular.
There is an expiration date on the packaging of any disinfectant. It indicates the time over which testing has confirmed the stability and effectiveness of the active ingredients in the disinfectant.
But what happens when the expiration date expires? Necessary...
BacteriaHygieneInfectionsChinese PneumoniaCoronavirus
10
MedVisor Editorial May 16
The warm season is the peak activity of ticks. Being carriers of dangerous infections such as encephalitis or Lyme disease, small parasites pose a threat to humans. Many people open the summer season in the spring, when ticks wake up from winter hibernation. Read on to learn how to prevent tick bites.
14
MedVisor Editorial May 17
Lyme disease or tick-borne borreliosis is an infectious disease caused by the bacteria Borrelia Burgdorferi. The bacterium enters the human body through the bite of an infected tick. Because infection is preventable, it is important to know how to prevent Lyme disease.
13
Tim Newman Reviewer Christina Frank, DDS, MedicalNewsToday.com May 17
Bad breath affects about 25 percent of people. There are many reasons why your breath may smell bad, but most come down to hygiene issues.
9
KidsHealth.com Reviewer Keith M. Cronan, MD May 16
When relaxing outside the city, do not forget about your country first aid kit. It should contain the most necessary medications to provide first aid in any situation.
DiseaseMedicinesPoisoningFirst Aid
17
Natalie Olsen, www.medicalnewstoday.com15 May
As part of a healthy, balanced diet, it is recommended to consume less foods and drinks high in sugar. Such food leads to caries, excess weight and problems with blood vessels and heart. Therefore, you need to know how much sugar you can eat per day.
DietFoodFoodSugar
Chronic pancreatitis is an extremely serious disease that requires dietary restrictions. A patient with pancreatitis cannot do almost anything, especially snacking on the run and eating fatty foods. But what about meat? Is it possible to eat kebab with pancreatitis if friends invite you to the dacha?
PancreasProteinPainDietComplications
5
MedVisor Editorial May 14
As soon as the sun begins to warm up, the desire to have a picnic in the fresh air and fry meat on the fire immediately appears. Despite the fact that you want to relax, you must not forget about safety. Poisoning from barbecue is not uncommon, so you need to take the preparation of meat seriously.
StomachIntestinesPoisoning
13
Tim Jewell, reviewer Judith Marcin, MD, HealthLine.com May 14
You have probably felt more than once how it sucks or hurts in the pit of your stomach after a hearty dinner. Pain in the epigastric region can be painful and acute, but most often it is ordinary discomfort that goes away without any problems. In this article we will give 10 reasons for such pain and look at each in more detail.
StomachPancreasAlcoholismPainGastritis
13
MedVisor Editorial May 13
Abdominal pain is pain that occurs in the area from the ribs to the pelvis. The abdominal cavity contains many organs, the stomach, liver, pancreas, small and large intestines, as well as reproductive organs and large blood vessels.
StomachIntestinesPainFirst Aid
22
MedVisor Editorial May 13
These country kebabs obviously won't do you any good if you eat too much of them. Today we’ll talk about what happens if you overeat meat. Especially if it is fatty and cooked over fire
StomachIntestinesProteinPainBloating
14
Cynthia Cobb, www.healthline.comMay 12
Belching is the body's way of getting rid of excess air in the digestive system. This air contains oxygen, carbon dioxide and nitrogen. Usually this phenomenon occurs after a person has eaten a heavy meal. In some cases, this is a symptom of a disease. Belching and cancer - could there be a connection between them? Let's look at it in the article.
StomachIntestineGastritisOncologyCancer
15
Jenna Fletcher Reviewer Saurabh Sethi, MD, MPH, MedicalNewsToday.com May 12
Abnormal twisting of the large or small intestine leads to a dangerous pathology that requires surgical intervention.
IntestinesPainDiagnosticsDietSurgery
11
Meredith Goodwin, www.healthline.com May 11
COVID-19 is being closely monitored by scientists around the world. Many symptoms of the disease are already known. However, it is believed that red eyes can also be a sign of coronavirus.
EyesChinese pneumoniaCoronavirusMyths
6
Susan Perry, MinnPost.comMay 11
As the COVID-19 pandemic progresses, new symptoms are appearing in the overall clinical picture. Doctors around the world are now reporting coronavirus 2020 rashes in some patients. Skin rashes on the feet that are similar to cold urticaria are called “Covid toe rash.”
SkinSkin DiseasesVirusesChinese PneumoniaCoronavirus
6
William Morrison, www.medicalnewstoday.com10 May
Arthritis of the joints is one of the main causes of knee pain. There are different types of arthritis that can affect the knee joint. The most common are osteoarthritis and rheumatoid arthritis. Treatment depends on the specific condition.
JointsArthritisLegs PainMedicationsRheumatoid Arthritis
12
Shawn Radcliffe, www.healthline.com May 9
Even if you follow all the precautions, in theory, you could become infected with coronavirus during a normal trip to the store.
The new virus is thought to spread mainly through personal contact, but it can also live on surfaces - including food packaging - for several days.
From all this, a logical question arises - how to treat products from the store against coronavirus...
Chinese pneumoniaCoronavirusProducts
Source: https://medvisor.ru/medicine/mkb/h00-h59/h30-h36/h35/0/
Causes
Normal vasculogenesis (vascular growth) of the retina in the fetus begins from the 16th week of intrauterine development and ends by 40 weeks of gestation. Thus, the younger the child’s gestational age, the more avascular zones are contained in his retina. The most susceptible to retinopathy of prematurity are children born from premature birth before the 34th week of gestation with a body weight of less than 2000. The development of retinal vessels is regulated by various mediators - growth factors, of which the most significant and studied are vascular endothelial growth factor, fibroblast growth factor and insulin-like factor. Dysregulation of normal angiogenesis and the development of retinopathy in premature infants are facilitated by conditions that cause changes in the partial pressure of oxygen and carbon dioxide in the blood. The fact is that metabolic processes in the retina are carried out through glycolysis, i.e., the breakdown of glucose, which occurs without the participation of oxygen. Therefore, a child’s prolonged stay on mechanical ventilation, oxygen therapy, and fluctuations in the administration of surfactants contribute to the development of retinopathy of prematurity. Additional risk factors influencing the occurrence of retinopathy of prematurity are fetal hypoxia, intrauterine infections, respiratory distress syndrome, intracranial birth injuries, sepsis, anemia of newborns, etc. One of the likely triggers for the development of retinopathy is exposure of the immature retina of a premature infant to excessive illumination, whereas normally Retinal angiogenesis occurs in utero in the absence of light exposure. The pathogenesis of retinopathy of prematurity is associated both with a violation of the formation of new retinal vessels and with changes in already formed vascular tracts. With retinopathy of prematurity, the formation of blood vessels in the avascular zones of the retinal periphery stops, and the newly formed vessels begin to grow into the vitreous body, which subsequently leads to hemorrhages, new formation of glial tissue, tension and tractional retinal detachment.
Short description
Diabetic retinopathy is a retinal lesion in diabetes, characterized by narrowing of the capillaries, increased aggregation of blood cells, retinal edema, and progressive obliteration of retinal capillaries. New formation of capillaries occurs in the retina, optic nerve, and vitreous body. Diabetic retinopathy ranks first among the causes of blindness and low vision. Frequency. Approximately 50–75% of patients with diabetes suffer from diabetic retinopathy. Visual disability is observed in more than 10% of patients with diabetes. Women suffer more often than men from type 2 diabetes. Risk factors • Long-term diabetes (more than 10 years) • Labile diabetes • Pregnancy • Renal failure • Arterial hypertension.
Code according to the international classification of diseases ICD-10:
- E10-E14 Diabetes mellitus
- H36.0 Diabetic retinopathy (e10-e14 with common fourth digit .3)
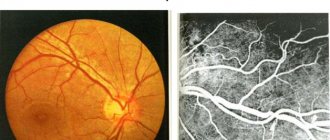
Classification • Non-proliferative (simple) diabetic retinopathy. Microaneurysms, hemorrhages, retinal edema, exudative lesions. Hemorrhages look like small dots or spots of a round shape, dark in color, and are localized in the central zone of the fundus or along large veins in the deep layers of the retina. Retinal edema is located in the central (macular) region or along the course of large vessels • Preproliferative diabetic retinopathy . Venous anomalies (clear-cut, tortuosity, doubling and/or marked fluctuations in the caliber of vessels), large amounts of lipid deposits, cotton-wool exudates (infarcts in the nerve fiber layer), intraretinal microvascular abnormalities, many large retinal hemorrhages. It occurs in 3 phases: •• vascular •• exudative •• hemorrhagic or exudative - hemorrhagic • Proliferative diabetic retinopathy. Neovascularization of the optic nerve head and/or other parts of the retina, vitreous hemorrhages, formation of fibrous tissue in the area of preretinal hemorrhages. Newly formed vessels are thin and fragile, which causes repeated hemorrhages. The resulting vitreoretinal traction leads to retinal detachment. Newly formed vessels of the iris (rubeosis) often lead to the development of secondary (rubeosis) glaucoma. Ophthalmological examination - measuring visual acuity and assessing the condition of the iris, lens, vitreous body and retina. Special Studies . Fluorescein angiography - disturbances in retinal hemodynamics, increased capillary permeability, the appearance of newly formed vessels and ischemic zones in the retina. Differential diagnosis . Retinopathy due to retinal vein thrombosis and hypertensive retinopathy.
Classification
The classification of retinopathy of prematurity, accepted in world practice, distinguishes active and cicatricial (regressive) phases during the course of the disease. The active phase of retinopathy of prematurity, depending on the location and severity of vascular changes, is divided into 5 stages: • Stage I.
The formation of a demarcation line is a narrow boundary separating the vascular (vascular) part of the retina from the avascular (avascular) part.
• Stage II.
Formation of an elevation in place of the demarcation line - a demarcation shaft (ridge).
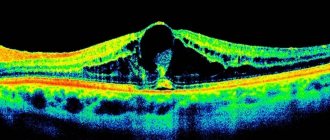
The vessels grow into the shaft and may form small areas of neovascularization. • Stage III.
Extraretinal fibrovascular proliferation appears in the shaft area.
Connective tissue and blood vessels grow over the surface of the retina and penetrate the vitreous body. • Stage IV.
Corresponds to partial retinal detachment caused by an exudative-traction mechanism.
This stage of retinopathy of prematurity is divided into substages: IVa - without macular detachment and IVb - with involvement of the macular zone in the detachment. • Stage V.
Total funnel-shaped retinal detachment (with a narrow, wide or closed funnel profile). In 70-80% of cases of stage I and II retinopathy of prematurity spontaneously regress, leaving minimal residual changes in the fundus. Stage III is the “threshold” stage and serves as the basis for preventive coagulation of the retina. Stages IV and V of retinopathy of prematurity are regarded as terminal due to the unfavorable prognosis for visual functions. In most cases, with retinopathy of prematurity, a sequential, stage-by-stage development of changes is observed, but a fulminant variant (“plus” disease), characterized by a malignant, rapid course, is possible. The duration of the active stage of retinopathy of prematurity is 3-6 months. If during this time there is no spontaneous regression of the changes, a scarring phase begins with the development of residual effects. At this stage, the child may develop microphthalmia, myopia, strabismus and amblyopia, late retinal detachment, vitreous fibrosis, complicated cataracts, secondary glaucoma, and subatrophy of the eyeball. Objective ophthalmological data are the only manifestations of retinopathy of prematurity, especially in its active phase, and therefore can simultaneously be regarded as symptoms of the disease.
What are the main symptoms of background retinopathy?
Regardless of the form, background retinopathy has the same clinical picture. The first symptoms are detected during the transition from the second to the third stage of the disease:
- patients may see floating spots;
- there is a significant deterioration in vision;
- there is a possibility of blood entering the vitreous body.
If at the stage of development of the disease a person has diabetes mellitus, then background retinopathy makes itself felt with the following symptoms:
- photopsia - sparks or flashes of light may appear in the eyes;
- inability to perceive colors correctly;
- decreased contrast of visible objects.
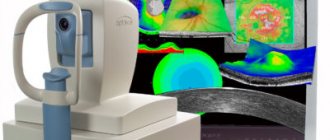
Diagnostics
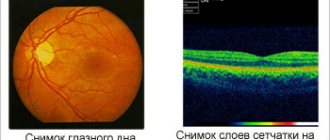
To identify retinopathy, all premature babies are examined by a pediatric ophthalmologist 3-4 weeks after birth. At an earlier age, signs of retinopathy of prematurity do not yet appear, but an ophthalmological examination may reveal other congenital eye pathologies: glaucoma, cataracts, uveitis, retinoblastoma. Further tactics involve dynamic observation of the premature baby by an ophthalmologist every 2 weeks (in case of incomplete retinal vascularization) or weekly (at the first signs of retinopathy), or once every 2-3 days (in case of “plus” disease). Examinations of premature babies are carried out in the presence of a neonatologist and an anesthesiologist-resuscitator. The main method for detecting retinopathy of prematurity is indirect ophthalmoscopy, performed after preliminary dilation of the pupil (mydriasis). Ultrasound of the eye additionally reveals extraretinal signs of retinopathy of prematurity in stages III-IV. For the purpose of differential diagnosis of retinopathy of prematurity and optic nerve pathology (developmental anomalies or atrophy of the optic nerve), a study of visual EP and electroretinography is performed on the child. To exclude retinoblastoma, ultrasound and diaphanoscopy are informative. To assess the degree of retinal detachment, it is proposed to use optical coherence tomography.
Background eye retinopathy
The term “retinopathy” in ophthalmology combines diseases of the retinal vessels (retina) that are not associated with inflammation.
“Background” refers to changes that occur against the background of various systemic diseases. In the general classification they are also called secondary. Background retinopathy and retinal vascular changes occur without pain, but can not only accompany the disease, but lead to serious complications. Therefore, the participation of an eye doctor in the diagnosis of vascular pathology is so important.
Changes are observed in both children and adults, regardless of the person’s gender. In ICD-10, the pathology is classified in the group of other retinal diseases under code H35.0.
Types of background retinal vascular disorders
The types of background retinopathy are determined by the underlying disease. The reasons may vary. According to the clinical classification, retinopathy is identified when:
- hypertension;
- injury;
- diabetes mellitus;
- blood diseases;
- atherosclerosis.
Some clinicians also add:
- autoimmune type;
- retinopathy due to radiation injury;
- as a consequence of thrombosis in the central retinal vein.
Let us consider the features of the pathogenesis, clinical picture and treatment of this pathology.
Hypertensive retinopathy
The characteristic change in blood vessels in the body during hypertension is completely reflected in the eyes: spasm of small arteries in the fundus occurs. The changes are more pronounced the more persistently high blood pressure persists, and depend on the duration of the disease.
During the course, there are 4 stages of pathological transformations:
- functional - the spasm is reversible and may disappear without treatment;
- angiosclerosis - hardening of the arterial walls appears, sclerotic lesions narrow the lumen and disrupt the nutrition of the retina, the changes become organic, therapeutic measures can prevent the spread, but it is completely impossible to get rid of them;
- hypertensive retinopathy itself - disrupts the structure of the tissue, minor hemorrhages and plasmorrhagia appear (swelling due to the release of plasma), fatty degeneration occurs in the cells, lipids are deposited in the arterioles, zones of ischemia and infarction are formed, requires constant maintenance treatment;
- neuroretinopathic stage - accompanied by swelling of the optic nerve, vascular hyalinosis, the appearance of foci of exudation and retinal detachment; With optic nerve atrophy, vision is irreversibly lost.
The last stage of hypertensive retinopathy accompanies the malignant course of hypertension, renal failure, and toxicosis during pregnancy.
In hemophthalmia, after the destruction of red blood cells, hemoglobin turns into hemosiderin and settles as grains in the tissues of the vitreous body, they form strands that contribute to retinal detachment
Ophthalmoscopy reveals the following picture:
- sharp narrowing of retinal vessels to complete obstruction;
- displacement of veins at the intersection with arteries deeper under the influence of heavy and dense vessels;
- exudation.
Lack of medical care leads to complications such as:
- retinal vein thrombosis;
- relapses of hemophthalmos.
In case of such phenomena in a pregnant patient, termination of pregnancy is recommended to preserve vision and prevent blindness.
Retinopathy due to traumatic injury
Eye injury is possible when:
- direct sudden action on the eyeballs (impact, pressure);
- creating conditions of acute ischemia under the influence of narrowing of the vessels of the chest and spine (especially those in the neck) - the carotid and vertebral arteries, which supply blood to the organs of the head (concussion, fractures, closed and open skull injuries, bleeding from the central vessels).
Post-traumatic cataract occurs when there is a sudden disruption of the blood supply to the eye
In response to ischemia, retinal cells experience oxygen deficiency. Hemorrhages occur, areas of damage appear with fluid effusion.
Most often, swelling of the space between the retina and the choroid occurs, clouding in the lower layers. This variant is called contusion or Prussian opacities. Lack of treatment leads to atrophic damage to the optic nerve.
Retinopathy in diabetes mellitus
Diabetes mellitus is accompanied by an increased concentration of glucose in the blood and metabolic disorders. Retinopathy complicates the course of the disease in patients with:
- overweight;
- anemia;
- hypertension;
- changes in the kidneys;
- high glucose levels and a long period of illness.
The development of retinopathy goes through 3 stages:
- angiopathy;
- retinopathy itself - the first and second stages do not differ from the hypertensive and atherosclerotic forms;
- proliferation - new small capillaries appear that penetrate the vitreous body, accompanied by hemorrhages and hyalinosis, this contributes to the rupture of the connections of the retina with the vitreous body, detachment.
Complications of diabetic retinopathy include:
- hemophthalmos,
- retinal detachment,
- formation of early cataracts.
Retinopathy and blood diseases
Most often, retinopathy occurs with the following blood diseases:
We advise you to read: Angiopathy in diabetes mellitus
- leukemia,
- polycythemia,
- multiple myeloma,
- different types of anemia.
The peculiarity of morphological changes is:
- overflow of the venous network of the fundus, leading to swelling of the optic nerve;
- thrombotic complications.
With ophthalmoscopy, the veins are bright red against the background of a bluish fundus.
With anemia, the fundus of the eye is paler than normal, the vessels are dilated, and there are areas of hemorrhage in the retina and vitreous body (hemophthalmos). Retinal detachment is possible.
Leukemia is accompanied by increased tortuosity of blood vessels, accumulation of exudate, swelling of the optic nerve head, and pinpoint hemorrhages.
With Waldenström's macroglobulinemia and multiple myeloma, general blood thickening occurs, retinal vein thrombosis occurs, hemorrhages occur, and microaneurysms form.
Atherosclerotic and postthrombotic retinopathy
The systemic disease affecting the retinal vessels in this case is widespread atherosclerosis. The deposition of plaques in the vessels supplying the brain and organ of vision leads to their narrowing.
As a result of a drop in blood flow and subsequent ischemia, the retinal arteries go through the same first 2 stages as with hypertension.
But ultimately, in severe cases, frozen microcrystals of exudate are deposited along the vessels.
Areas of hemorrhage are detected in the fundus, and the optic disc is paler than normal.
Complications of atherosclerosis manifest themselves as:
- thrombosis of small arteries;
- atrophy of the retina and optic nerve.
Postthrombotic retinopathy is associated with thrombosis in the area of the central retinal vein, possibly in its other branches. The formation of auxiliary collaterals and shunts in the vessels of the eye occurs slowly, not earlier than three months. At this time, exudative foci of varying density are visible in the fundus.
How does background retinopathy manifest clinically?
The symptoms of background retinopathy of different forms are almost the same. They appear at the border of the second and third stages:
- patients note decreased vision;
- see floating spots (scotomas);
- blood may enter the vitreous body (hemophthalmos).
In patients with diabetes mellitus, the disease begins with:
- disturbances in near visual acuity (farsightedness);
- the appearance of intermittent floating spots, veils before the eyes.
Ultimately, the pathology leads to irreversible blindness.
Early symptoms of background retinopathy are:
- photopsia - flashes of light or sparkles in the eyes;
- impaired perception of colors;
- decreased contrast of visible objects.
Methods for identifying underlying circulatory disorders
Diagnosis of retinopathy requires:
- participation of specialists of various profiles (ophthalmologist, endocrinologist, neurologist, pediatrician, cardiologist);
- conducting a complete study of visual acuity and fields (perimetry) - allows us to judge the functional state of retinal cells;
- mandatory ophthalmoscopy (direct and indirect) when dilating the pupil with a special medication;
- Ultrasound of the eyeballs - to determine areas of compaction, hemorrhages, scars, hyalinosis inside the eye.
These methods are used by territorial clinics.
Diaphanoscopy - transillumination of the eyeball with a narrow light beam in order to detect retinal detachment and differential diagnosis with tumors
More subtle ways are:
- fluorescein angiography of the fundus;
- biomicroscopy of the eye;
- electrophysiological techniques (electroretinography) - allows you to assess the viability of retinal tissue;
- angiography;
- magnetic resonance imaging.
They are carried out in specialized centers and departments.
Treatment
To treat secondary retinal pathology, therapy for the underlying disease is necessary.
For hypertension and atherosclerosis, treatment requires:
- correction of blood pressure;
- the use of antispasmodics and arterial dilators;
- administration of anticoagulants to prevent thrombosis.
Prescribed:
- vasodilators;
- diuretics;
- anti-sclerotic drugs;
- antihypertensive.
In case of diabetes mellitus, to maintain normal glucose levels, the necessary optimal dosage of a hypoglycemic agent is selected.
Background retinopathy in blood diseases is difficult to treat and often leads to irreversible blindness.
For any form of retinopathy you need:
- angioprotectors;
- vitamins;
- drugs that improve microcirculation;
- antioxidants that improve tissue resistance to oxygen deficiency.
At the stage of neuroretinopathy, a course of electrophoresis on the eyeballs with proteolytic enzymes can be effective.
The treatment method for detecting signs of retinal detachment is laser coagulation. A beam is used to cauterize the separated flap to its place.
For scars and hemorrhages in the vitreous, operations are performed to remove it - partial, complete or vitreoretinal vitrectomy
To saturate the eye tissues with oxygen, therapy is prescribed in special pressure chambers.
Retinopathy in childhood
In children, manifestations of background retinopathy are possible after injury, with severe diabetes mellitus, and blood diseases. Causes such as hypertension and atherosclerosis are very rare.
But there is a special form that is unique to children - retinopathy of prematurity.
Among babies born prematurely, the greatest risk is:
- born at a gestational age of 31 weeks or less;
- with body weight less than 1.5 kg;
- have had a blood transfusion;
- receiving oxygen for a long time to restore their general condition.
Retinal pathology requires compliance with oxygen-free methods of metabolic processes in the body to complete development. But to nurse babies and ensure the growth of vital organs, oxygen is needed in inhalation, which is supplied to special children's incubators. It turns out that retinopathy is formed as a result of treatment.
In order to timely detect pathology, an ophthalmologist examines newborns from risk groups at the age of three to four weeks, then every 2 weeks until the retina completes maturation.
Types of complications:
- formation of early myopia;
- glaucoma;
- strabismus;
- amblyopia (disorders of the visual function of one of the eyes);
- retinal detachment and blindness.
Amblyopia is called the “lazy eye” disease.
At the initial stage, the child may self-heal. When the consequences appear, ophthalmologists decide which operation is best to use:
- laser coagulation;
- cryoretinopexy (freezing of the detached portion of the retina);
- more serious interventions with lens replacement.
Children diagnosed with retinopathy during the neonatal period should be examined annually by an ophthalmologist.
To prevent the disease, a complex of preventive treatment is carried out for pregnant women with kidney diseases, hypertension, blood pathologies, diabetes mellitus, and those who have suffered injuries.
The conditions for caring for premature infants must be prepared to preserve the health of the child in case of any identified pathology. The effectiveness of treatment of underlying retinal vascular lesions depends entirely on the possibility of compensating for disorders caused by the underlying disease. Therefore, supportive and preventive therapy and periodic consultations with an ophthalmologist are so important.
Source: https://icvtormet.ru/bolezni/fonovaya-retinopatiya-glaz
Treatment
In stages I–II of retinopathy of prematurity, treatment is not indicated. In stage III, in order to prevent the progression of retinopathy of prematurity to the terminal stages, prophylactic laser coagulation or cryocoagulation of the avascular zone of the retina is performed (no later than 72 hours from the moment of detection of extraretinal proliferation). The effectiveness of preventive coagulation treatment for retinopathy of prematurity is 60-98%. Local complications of surgical procedures include eye burns, hyphema, preretinal membranes, iridocyclitis, and occlusion of the central retinal artery. General somatic complications may include apnea, cyanosis, bradycardia or tachycardia. The effectiveness of coagulation treatment for retinopathy of prematurity is assessed after 10-14 days. When the process stabilizes or regresses, treatment is regarded as effective. In case of ongoing extraretinal proliferation, cryo- or laser coagulation may be repeated. In the regressive and postoperative period, instillations of medications (disinfectants, antioxidants, anti-inflammatory), physiotherapeutic effects (electrophoresis, magnetic stimulation, electro-oculostimulation) are prescribed. In case of further progression of retinopathy of prematurity to stages IV-V, the need arises for vitrectomy (lensvitrectomy) or circular filling of the sclera (extrascleral filling).
Forecast
In most children, retinopathy of prematurity does not progress beyond stages I-II, changes in the retina undergo reverse development; At the same time, sufficiently high visual acuity is maintained. However, in half of them, by the age of 6-10 years, refractive errors (myopia, farsightedness, astigmatism) and oculomotor disorders (strabismus, nystagmus) are detected. When retinopathy of prematurity progresses to stages IV-V or the fulminant form of the disease, the prognosis for maintaining visual function is unfavorable.
Prevention
Prevention of retinopathy of prematurity is, first of all, prevention of premature birth; carrying out therapy aimed at prolonging pregnancy; proper nursing of premature infants, their dynamic monitoring by a pediatric ophthalmologist. Children who have suffered retinopathy of prematurity should undergo regular ophthalmological examinations at an older age, including visometry, refractometry, electrophysiological studies, computer perimetry, etc.