The eyes play an irreplaceable role in human life, allowing him to navigate in space and receive information from the environment. Deterioration of vision negatively affects the quality of life and emotional state of a person in general. Numerous changes in the body that occur over time also affect the visual system, causing eye diseases.
It should be remembered that age-related changes cannot be avoided, so visiting an ophthalmologist after 40 years will allow you to see the full picture of the condition of your eyes and small deviations that can be corrected in time.
Age-related changes in the lens of the eye
Phakosclerosis is a disease of the eye lens in which there is a gradual thickening of the lens. The process begins with a slight decrease in elasticity, and over time leads to complete sclerosis of the lens.
Transformations are carried out very slowly over many years; they can be roughly divided into the following periods:
- The lens of newborns is very soft, transparent and has a round shape, resembling a ball. With age, these characteristics undergo changes, the front part of the lens becomes flat, and the color becomes beige, sometimes turning yellow.
- In adolescence, the first changes begin, tissue rigidity appears, affecting the cortical regions, and then moving to the core.
- At the age of 30, density indicators in the cortical regions and nucleus level out, and later an increase in rigidity is noted.
- At the age of 40, the first pronounced symptoms appear, the cause of which is a noticeable loss of elasticity of the lens; during this period, many people develop presbyopia and farsightedness appears.
- At sixty, the ability of the lens to transform significantly deteriorates, and usually during this period the ophthalmologist detects sclerosis of the lens of the eye. Since these changes are associated with a person’s age, they affect the visual system as a whole, so most patients are diagnosed with phacosclerosis of both eyes.
Features of the lens
The lens tends to change throughout a person's life. In infants, the lens is colorless and soft, it has a spherical shape. In children, it becomes a flat lens at the front of the eyeball. In adults, crystals turn from transparent to yellowish.
By the age of forty, a person’s lens begins to lose its elasticity, and presbyopia develops (a defect that leads to the inability to distinguish small print up close). At sixty, most people are diagnosed with sclerosis of the lens nucleus. The pathology is fraught with deterioration in the perception of objects near.
Research by scientists in this area
For many years, doctors have been familiar with such a problem as phacosclerosis of the eyes. In order to conduct laboratory studies and study the thickening of the lens of the eye that appears over time (what it is and what it depends on), scientists involved representatives of different ages in the experiments. Thanks to special devices, it was possible to take measurements and record data on the degree of lens hardness in young, middle-aged and elderly people.
| Hypotheses have been raised about possible dehydration of the lens over time. But further research has proven that this does not happen, and the fluid content inside the lens does not change over the years. |
To date, the problem has not been completely solved, and there is no precise explanation of the lens compaction mechanism. Continued research in the field of ophthalmology may yield positive results in the future and allow us to better understand the processes taking place.
Main types of cataracts
Let's look at the different types of cataracts and their characterological features.
First of all, cataracts are divided into congenital and acquired. Accordingly, congenital cataracts are formed in the fetus during intrauterine development, as a result of which the baby is born with eye pathology.
Acquired cataracts develop during a person’s life under the influence of predisposing factors. Congenital cataracts do not progress, that is, the number of opacities and their intensity do not increase over time.
And any acquired cataracts progress - over time, the number of opacities and the degree of their intensity in the lens increase.
- Age-related (senile, senile) cataracts. developing due to age-related changes in the body;
- Traumatic cataracts. developing as a result of injury or contusion of the eyeball;
- Radiation cataracts. developing due to exposure of the eyes to ionizing, radiation, x-rays, infrared radiation or electromagnetic waves;
- Toxic cataracts. developing with long-term use of medications, smoking. alcohol abuse or poisoning;
- Complicated cataracts. developing against the background of other eye diseases (uveitis, iridocyclitis, glaucoma, etc.);
- Cataracts against the background of severe chronic pathologies (for example, diabetes, thyroid diseases, metabolic disorders, dermatitis, etc.);
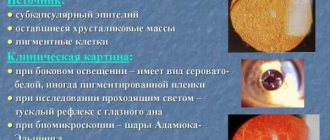
- Secondary cataracts. developing after one operation to remove a cataract and install an artificial intraocular lens (lens).
- Initial cataract. An excess of fluid appears in the lens, as a result of which water gaps form between the fibers, which are foci of opacities. Cloudiness usually appears in the peripheral part of the lens, and rarely in the center. Foci of opacities when looking inside the pupil in transmitted light look like spokes in a wheel. At this stage, vision is not significantly affected.
- Immature cataract. Cloudiness from the peripheral spreads to the optical zone of the lens, as a result of which a person’s vision sharply deteriorates. The fibers swell, causing the lens to increase in size.
- Mature cataract. The entire lens is cloudy, and a person sees practically nothing, but can only distinguish whether it is light or dark indoors or outdoors.
- Overripe cataract. The fibers disintegrate and the lens substance liquefies, accompanied by an inflammatory process, which leads to increased intraocular pressure and complete blindness. If the substance of the lens has completely liquefied before this structure is removed, then its core sinks down, and such a cataract is called a blink cataract. Sometimes the substance of the lens liquefies, but the shell remains dense, and in this case it shrinks. The operation to remove the lens at this stage is performed only for the purpose of preserving the eye, since vision during the transition of cataracts to overripe, as a rule, is lost irretrievably due to damage to the structures of the ocular analyzer by toxic decaying lens structures. An overmature cataract appears as a large (dilated) milky-white pupil with numerous white spots. In rare cases, an overripe cataract appears as a black pupil due to excessive sclerosis of the lens nucleus.
- anterior and posterior polar;
- fusiform;
- layered;
- nuclear and cortical (are the most problematic for treatment);
- posterior subcapsular (posterior capsular cataract);
- complete cataract.
- anterior and posterior polar;
- fusiform;
- layered;
- nuclear and cortical (are the most problematic for treatment);
- posterior subcapsular (posterior capsular cataract);
- complete cataract.
1. Layered peripheral cataract (picture 1 in figure 2). The opacities are located under the lens shell, with transparent and opaque areas alternating.
2.Zonular cataract (picture 2 in figure 2). The opacities are located around the center of the lens, with alternating transparent and opaque areas.
3. Anterior and posterior polar cataracts (picture 3 in Figure 2). Cloudiness in the form of a round white or grayish spot is located directly under the capsule in the region of the posterior or anterior pole of the lens in the center of the pupil. Polar cataracts are almost always bilateral.
4. Fusiform cataract (picture 4 in Figure 2). The opacification in the form of a thin gray ribbon has the shape of a spindle, and occupies the entire width of the lens along its anteroposterior dimension.
5. Posterior subcapsular cataract (picture 5 in Figure 2). The opacities are whitish wedge-shaped lesions located along the outer edge of the posterior part of the lens shell.
6. Nuclear cataract (picture 6 in Figure 2). Cloudiness in the form of a spot approximately 2 mm in diameter, located in the center of the lens.
7. Cortical (cortical) cataract (picture 7 in Figure 2). Opacities are whitish wedge-shaped lesions located along the outer edge of the lens shell.
8. Complete cataract (picture 8 in Figure 2). The entire substance of the lens and capsule is cloudy. As a rule, such cataracts are bilateral, that is, both eyes are affected.
Figure 2 – Types of cataracts depending on the location and shape of the opacities.
Congenital cataracts can be represented by any of the above types, and acquired ones are only nuclear, cortical and complete. The shape of cataract opacities can be very diverse - stellate, disc-shaped, cup-shaped, rosette, etc.
Symptoms of phacosclerosis
If you are accidentally diagnosed with eye phacosclerosis during an examination by an ophthalmologist, symptoms may not appear immediately. This disease is not characterized by a sharp decline in vision; the situation worsens gradually, and over time the following signs of the disease may appear:
- Overexertion accompanied by headache and feeling of fatigue (asthenopia)
- The appearance of dry eyes or, conversely, constant tearing
- Unpleasant sensations or pain
- Decreased visual acuity when text “floats” when reading
- Eye sensitivity to bright light
- Decreased ability to distinguish colors (they become “pale” and patients complain that “everything has become gray and dull”)
- Gradual development of presbyopia
With this disease, both eyes are affected, and with severe symptoms, a person is forced to turn to a specialist for help.
Return to contents
Causes of phacosclerosis
We can say that the slow compaction of the lens is a natural process that no one can avoid. But sometimes it happens a little faster than expected, and the reasons can be very different:
- Changes in the body due to age
- Genetically determined susceptibility to disease
- The patient has a disease such as diabetes mellitus
- Complications of glaucoma
- Inflammation of the iris, formation of cataracts, ulcers on the cornea of the eye
What lens is used to replace the lens during atrophy?
There are several types of IOLs.
They differ in the material from which they are made and functionality. Today, soft lenses are mainly used. To install them in the eye, you do not need to make a large incision, which reduces the risk of complications and shortens the recovery period. Based on the method of refraction of light rays, IOLs are divided into spherical and aspherical. Aspherical lenses are more expensive. They provide good vision in the dark, prevent glare, and provide a wide overview. Spherical IOLs provide less clear images at twilight.
Multifocal toric lenses guarantee 100% vision. These are the most expensive prostheses. They provide excellent vision at any distance at any time of the day. They are prescribed in cases where patients have also been diagnosed with astigmatism or presbyopia.
Sometimes the doctor suggests that the patient install an IOL with protective functions. They have protection from the ultraviolet spectrum of sunlight. These lenses are usually blue or yellow. Their color does not affect color perception in any way. Lens atrophy is an irreversible and very dangerous process. Just a few decades ago people were doomed. It was impossible to save the visual functions of the eye. Today, lens replacement surgery allows a person, even in old age, to regain good vision.
How is lens sclerosis diagnosed?
If you experience some of these symptoms, contact your ophthalmologist for advice. A timely examination will allow you to diagnose the disease and take measures to prevent a sharp decline in vision.
An accurate determination of the disease is carried out using the following diagnostic methods:
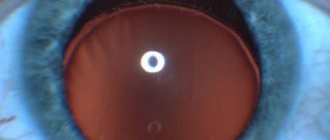
- Visual ophthalmological examination. Transmitted light, side lighting and special lenses give the doctor the opportunity to closely examine the lens and determine whether its shape has changed.
- The slit lamp gives the ophthalmologist the opportunity to use biomicroscopy for diagnosis. This method allows you to not only notice the changed shape, but also the position of the lens. Its transparency is assessed and turbidity is detected
- Carrying out a procedure such as echobiometry helps the specialist to detect the exact location of the lens seals, the intensity and location of the opacities
Diagnostics
Phacosclerosis of the eye lens progresses very slowly, which is why it often goes unnoticed. Often, pathology is discovered by chance, during an ophthalmological examination for another reason. To make an accurate diagnosis, it is necessary to carry out a number of examinations:
- Ophthalmoscopy. The lens is studied in detail under suitable lighting, using various lenses. In particular, the IOL is examined under lateral illumination using a 20 diopter lens.
- Biomicroscopy. Using a slit lamp, the density of the lens nucleus is determined, which at this point usually turns yellow. Also, during biomicroscopy, the shape, location and transparency of the IOL are revealed.
- Visometry. Allows you to determine the degree of visual acuity and diagnose myopia or farsightedness.
- Ultrasonography. During the examination, the thickness, depth, length and some other parameters of the intraocular lens are determined. The procedure is performed with the patient in an upright position, after the anesthetic is administered.
Autorefractometry and some other diagnostic measures may also be prescribed. All procedures must be carried out as prescribed by a doctor and by an experienced specialist.
Treatment methods for phacosclerosis
Ophthalmologists do not recommend using medications to treat this disease. The fact is that medications are not effective in the case of age-related changes affecting the visual organs.
Some remedies can be used to combat the symptoms of the disease and provide corrective measures with the help of glasses. Since there is no radical therapy, attention should be paid to measures that can be taken to slow down the process of sclerosis.
After the diagnosis, the doctor will definitely tell you what can be done to improve the condition of the visual organs in your case. The main emphasis is on a healthy lifestyle, varied diet and periodic intake of special vitamins. Return to contents
Traditional methods of treatment
We have already talked about the ineffectiveness of treating eye phacosclerosis with drugs. But you can help your body using folk remedies. Make sure you have fruits and vegetables on your table every day.
Carrots, bell peppers, pomegranates, oranges, spinach, apricots, blueberries, sweet potatoes, broccoli, and cherries are very good for vision. Eat nuts and dried fruits, eggs, fish and seafood. Introduce Chia seeds, sesame seeds and flax grains into your diet. Drink green and white teas, which are rich in antioxidants.
Treatment of nuclear cataracts
If a person is diagnosed with nuclear cataract, treatment is prescribed depending on the stage of the disease. At the first stage of the development of the disease, maintenance therapy is used to stop the progression of the disease.
When moving into the next phases and a significant drop in visual ability, the patient is advised to undergo surgery to replace the biological lens with an IOL
Drug therapy
The purpose of using medications is to slow the progression of the disease. Such therapy does not help the patient recover, but only delays the moment of necessary surgical intervention. The following medications are recommended to the patient:
- Vitamins and medications for correcting metabolism and maintaining vision (nicotinic acid, cysteine, riboflavin, glucose, vitamin complexes)
- Drops that are prescribed to patients with nuclear cataracts of various etiologies (“Smirnov Drops”, “Quinax”, “Katachrome”, “Vitafacol”, “Taufon”, “Vicein”, “Vita-Iodurol”, etc.)
Surgery
If with the help of medications you can only stop the course of the disease, then surgery helps to completely restore vision. The cloudy lens is removed and an artificial lens is installed.
The operation lasts 30–40 minutes, and the patient is allowed to go home a few hours after the operation. Lens replacement is painless; manipulations are performed under anesthesia.
An instrument is inserted through a small incision to remove the lens (a laser or ultrasound may be used). After removing the biological lens, an implant is installed. The incision heals on its own without stitches
Return to contents
Cost of the operation
The cost of such operations consists of several components and depends on the clinic where the lens replacement will be performed, the chosen surgical technique, and the type and quality of the implant. The total cost can range from 30 to 120 thousand rubles. In most cases, such manipulation with the installation of a good quality lens costs patients 50 thousand rubles.
Main types of operations
There are three common types of operations, differing in the method of execution, the degree of trauma to the visual organs and the rehabilitation period:
- An extracapsular treatment method is an intervention in which the capsule in which the clouded lens is located is preserved. It is removed through a small incision, after which an IOL is installed and the incision is sutured. The operation is followed by long-term rehabilitation, during which vision will gradually recover.
- During intracapsular surgery, the human biological lens is frozen with a special cryoextractor and removed along with the capsule. After this, the IOL is inserted. This method is the most traumatic and is rarely used.
- A new method of phacoemulsification, which uses laser equipment or ultrasound, is considered safe. The lens breaks and turns into liquid, which is removed with a special instrument. The incision is very small, so no stitches are required. Sealing and healing proceed quickly, rehabilitation is completed in the shortest possible time.
Possible complications after surgery
IOL transplantation operations have minimal risks of complications, but sometimes a person develops secondary cataracts or phacogenic glaucoma. Among the possible difficulties, ophthalmologists name pigmentary degeneration or retinal detachment, the appearance of strabismus or other pathologies of the eyeball.
Preventative measures to prevent complications
In order to prevent the development of complications, patients, for their part, must adhere to the ophthalmologist’s instructions and observe the following precautions:
- During the postoperative period, you should refrain from physical activity
- Do not lie or sleep on your side on the side of the healing eye.
- You need to wear a special bandage to protect your eye from infection.
- Care should be taken when swimming to avoid getting water, gel and shampoo into your eyes.
- At first you should not go outside, and if this cannot be avoided, you need to wear sunglasses
- It is undesirable to expose the operated eye to temperature changes or stay in cold air for a long time.
Prevention
We have already said that there is no special treatment for lens sclerosis. You can only take preventive measures in order to prevent the premature manifestation of the disease and prevent the appearance of severe symptoms. For this:
- Give up alcohol and tobacco products
- Don't forget about training, choose a sport that you like and practice 2-3 times a week
- Take synthetic vitamins additionally 1-2 times a year (Okuwait Lutein Forte, Blueberry Forte with Lutein, Complivit Ophthalmo, Vitrum Vision Forte, Biori have a good effect).
- Maintain a normal weight. Obesity can lead to the development of type 2 diabetes, and this will negatively affect the visual system.
- Avoid eye injury
Follow these simple tips, undergo scheduled examinations with an ophthalmologist - and you will maintain good vision for many years!