Ectopia of the lens is its complete or partial displacement from its normal position. Pathology can be either congenital or acquired. There are two types of ectopia: subluxation (subluxation) and dislocation (luxation). In the first case, it moves partially, while remaining within the pupil. During luxation, it prolapses into the anterior chamber or vitreous, and the eye becomes aphakic.
Congenital ectopia of the lens is almost always bilateral and is combined with other defects in the development of the visual organ. The pathology can be inherited in an autosomal dominant or autosomal recessive manner and is often accompanied by pupil displacement, aniridia, changes in corneal diameter, glaucoma, and cataracts. The disease may appear immediately after birth or later in life.
Causes of hereditary ectopic lens
Hereditary ectopia of the lens can accompany both diseases without systemic changes and genetically determined systemic pathologies. The first group includes:
- Familial ectopia, which is characterized by the superior temporal direction of lens displacement. In this case, the dislocation is two-sided. The type of inheritance of this disease is autosomal dominant. The first signs of lens luxation usually appear in early childhood, but sometimes the disease manifests itself later.
- Displacement of the pupil and lens. This pathology does not occur often; displacement occurs in different directions; the type of inheritance is utosomal-recessive. With this disease, the pupil becomes slit-like and small and dilates poorly. It can also cause transillumination of the iris and changes in the shape and size of the lens itself (microspherophakia). Often, the disease is accompanied by glaucoma, an increase in the diameter of the cornea, and associated cataracts.
- Aniridia (absence of the iris), which can also be accompanied by secondary ectopia of the lens.
However, most often, ectopia of the lens becomes one of the signs of a genetic systemic pathology. For example, Marfan syndrome, the inheritance of which is an autosomal dominant type, is accompanied by damage to the connective tissue, which also affects the eyeball:
- In most patients, symmetrical bilateral dislocation of the lens occurs in the superotemporal direction. At the same time, the ligaments of Zinn are not damaged and accommodation is preserved. However, there have been cases of lens displacement into the vitreous body or anterior chamber of the eye. There is also a change in the size and shape of the lens (microspherophakia).
- In the case of congenital pathology, with the involvement of the anterior angle in the process, dense processes of the iris are formed, and the thickness of the trabecular plates increases. This symptom often causes intraocular hypertension, which is also detected in the vast majority of patients.
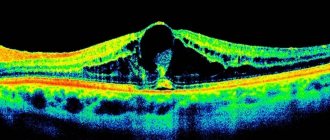
- A severe complication of the disease can be retinal detachment, which often occurs against the background of lattice degeneration and high degrees of myopia.
- Less often than other changes are detected: hypoplasia of the pupil dilator muscle, strabismus, flattening of the cornea, translumination of the iris, blue color of the sclera.
Another systemic disease accompanied by ectopic lens is Weil-Marchesani syndrome. This rare disease is also accompanied by changes in connective tissue. Among its clinical manifestations, in addition, there is mental retardation, decreased joint mobility, growth retardation, and brachydactyly. The type of inheritance is autosomal dominant or autosomal recessive. Eye changes include:
- Bilateral synchronous downward displacement of the lens and microspherophakia, which occur in half of patients in childhood and adolescence.
- Secondary angle-closure glaucoma, which occurs as a result of a congenital disorder of the structure of the angle of the eye or due to pupillary block (with anterior displacement of the lens and spherophakia).
- Presenile destruction of the vitreous body, asymmetrical axis length.
Ectopia of the lens occurs with homocystinuria, a disease inherited in an autosomal recessive manner, which is classified as a congenital disorder of metabolic processes. It is characterized by the accumulation of homocysteine and methionine in the body, as well as a lack of cystathionine beta synthetase (liver enzyme). The disease is accompanied by changes in skeletal bones and an increased tendency to form blood clots. Visual changes include:
- Displacement of the lens medially downwards, manifested by the age of ten. Loss of accommodation due to damage to the ligament of cinnamon, which is associated with the accumulation of cysteine.
- Secondary angle-closure glaucoma occurs when the lens moves into the anterior chamber of the eye, causing pupillary block.
Lens dislocation also accompanies hyperlysinemia, a very rare autosomal recessive hereditary disease that occurs due to deficiency of lysine-alpha-ketoglutar reductase. Patients with hyperlysinemia are characterized by muscle and ligamentous weakness, mental retardation, and epileptiform seizures.
Ectopic lens is characteristic of a very rare autosomal recessive disease caused by sulfite oxidase deficiency due to impaired sulfur metabolism. At the same time, it is accompanied by muscle rigidity and mental retardation. With this disease, patients rarely live more than 5 years.
Displacement of the lens is accompanied by two more hereditary syndromes: Ehlers-Danlos and Stickler. The latter syndrome is also characterized by dangerous retinal detachment.
PATHOLOGY OF THE LENS (DEVELOPMENTAL ANOMALIES, CATARACTS)
The lens is one of the most important optically active structures and components of the accommodative apparatus of the eye. Its normal functioning is possible only if transparency, correct location and structure are maintained. Cloudiness or dislocation of the lens leads to decreased vision and disruption of the act of accommodation. Therefore, early diagnosis and treatment of lens pathology constitute an important section in pediatric and age-related ophthalmology.
Pathological conditions of the lens in children primarily include anomalies of its development (microphakia, spherophakia, anterior and posterior lenticonus or lentiglobus, coloboma) and location (subluxation or dislocation), as well as congenital opacities (cataracts, remnants of the vascular bursa of the interpupillary membrane). Aphakia, a congenital absence of the lens, is extremely rare. In addition, lens pathology can be acquired. This is both dislocation and clouding caused by a wide variety of general and local causes, including age-related changes (senile cataracts).
ANOMALIES OF LENS DEVELOPMENT
MICROPHAKIA (SMALL LENS)
Changes in the anterior part of the eye are characterized by some deepening and unevenness of the anterior chamber, slight iridodonesis (tremor of the iris), detected when the eyeball moves, as well as a more or less pronounced decrease in vision due to ametropia and a weakening of accommodative ability. Even with a slight dilation of the pupil in the presence of microphakia, the contours of a small lens and ciliary ligaments are visible in transmitted light and in lateral lighting.
Treatment is only surgical if visual acuity with spectacle correction is below 0.2. The essence of the operation is the removal of the lens, followed by the prescription of appropriate glasses or contact lenses or the introduction of an intraocular lens (IOL). It is better to replace the removed lens with an IOL at puberty (high school, adolescence).
MACROPHKIA (LARGE LENS)
It manifests itself as a small anterior chamber, decreased vision and weakened accommodation. Intraocular pressure may increase. A refined diagnosis of macrophakia is made on the basis of biomicroscopic and echo-ophthalmographic studies.
Treatment is the same as for microphakia.
LENTICONUS
Lenticonus can be either anterior or posterior. In this case, the cone-shaped part of the lens has a different radius of curvature and height. Anterior lenticonus can be suspected by the reduced size and unevenness of the anterior chamber, decreased vision and deterioration of accommodation. Posterior lenticonus can be detected only with skiascopy, biomicroscopy and echoophthalmography. Only low visual acuity can suggest the presence of a posterior tape-cone. In the presence of lenticonus, there is often mixed irregular lens astigmatism, which is practically not amenable to spectacle correction.
Treatment is the same as for micro- and macrophakia.
DISLOCATION OF THE LENS
Lens dislocation may manifest as subluxation or dislocation into the anterior chamber or vitreous. Depending on the type and degree of dislocation of the lens, changes in the anterior part of the eye can be different. Vision is reduced to varying degrees and accommodation is impaired. The anterior chamber, the size and rigidity of the pupil change (deepen or decrease), and iridodonesis is noted. Symptomatic (secondary) hypertension (increased intraocular pressure) often occurs, which develops into secondary glaucoma. The causes of hypertension are varied and depend on the nature of the dislocation (irritation of the ciliary body, blockade of the iridocorneal angle).
Most often, lens dislocation occurs in Marfan and Marchesani syndromes. The process is two-way.
Treatment is only surgical and consists mainly of removing the subluxated or dislocated lens. The question of indications and time of surgery is decided depending on the state of intraocular pressure and visual acuity. Prolonged hypertension, even in the presence of relatively good vision, is an indication for urgent surgery. The choice of surgical method depends on both the nature of the dislocation and the state of vision.
In conclusion, it must be emphasized that anomalies in the development and location of the lens are almost always accompanied by a decrease in visual acuity, and often the appearance of strabismus. Diagnosis of anomalies is difficult and is possible mainly as a “finding” during the study of clinical refraction. Therefore, pediatricians should always check the clinical refraction of all children by the age of one year.
CATARACTS
All cataracts, i.e., clouding of the lens, are accompanied by a decrease in visual acuity down to light perception. Low vision usually leads to the development of nystagmus and strabismus, as well as amblyopia. Cataracts can be divided into congenital and acquired. Congenital cataracts can be of different origins: some of them are hereditary (family), others are a consequence of intrauterine pathology. Thus, the cause of congenital cataracts can be hypocalcemia and hypothyroidism in pregnant women. In animal experiments, excluding vitamin A from the diet of experimental pregnant females and creating oxygen starvation can cause lens pathology in the fetus.
Congenital cataracts can also be caused by severe diabetes, toxoplasmosis, or viral infections (rubella) in pregnant women. The question of the nature of congenital cataracts in each individual case can be resolved by conducting a thorough family history and studying the course of pregnancy.
In addition, one should distinguish between stationary cataracts (with some exceptions - congenital) and progressive (almost all acquired). The division of cataracts according to their localization and the massiveness of the opacification is of well-known importance. Among congenital cataracts, polar, zonular (layered), nuclear, membranous, cortical, complete (total), etc. are more common, and among acquired cataracts - initial, immature, mature, overripe or partial, incomplete, complete. An indirect sign of the intensity of lens opacification is the magnitude (degree) of a decrease in visual acuity in each child or adult with cataracts. An important role is also played by the pathological condition of the eye (inflammation, trauma, etc.) and the body as a whole (diabetes, toxoplasmosis, etc.) in people with cataracts.
CONGENITAL CATARACTS
The average incidence of congenital cataracts is 5 per 100,000 children. The most accessible and simplest characteristic of congenital cataracts is their location and intensity of opacification.
Polar cataract is characterized by the presence in the pupil area (in the center) of a grayish or whitish spot about 2 mm in diameter. These cataracts can be located at the anterior or posterior poles of the lens capsule. Mostly anterior polar cataracts are visible to the naked eye. Posterior polar cataracts are detected by transmitted light or, best of all, by biomicroscopy. Polar cataracts are almost always bilateral.
If polar cataracts do not occupy most of the pupil, then vision is not greatly reduced, but if they correspond to the entire size of the pupil, then visual acuity is significantly reduced. Polar cataracts are usually not treated. But in cases where vision is reduced, the pupil is dilated using mydriatic means, and sometimes they resort to surgery.
Complete (total) cataract is characterized by clouding of the entire lens, which is determined in conditions of a dilated pupil. It is almost always bilateral. Vision decreases down to light perception with correct projection. In early childhood (up to one year), treatment is surgical.
Membranous cataracts are distinguished by the fact that, as a rule, there is diffuse opacification of the entire lens. There are almost no lens masses between the anterior and posterior capsules and the lens is not spherical. This is manifested by the fact that the anterior chamber of the eye in children with membranous cataracts is deeper than, for example, with complete cataracts, and there is also iridodonesis. It is possible to clarify the diagnosis of these cataracts using biomicroscopy in echobiometry (one lens echo peak instead of two). Object vision with membranous cataracts is absent and only light perception with the correct projection is determined. Surgical treatment at an early age (first six months of life).
Zonular (layered) cataracts are most often detected from the first days of birth, but can develop during the first year of life. The diagnosis of such cataracts can only be made after dilation of the pupil. It is visible in the form of a gray round spot (disk) in the center with a clear edge and processes located on this edge, perpendicular to it, “riders”; there are zones of clearing (type of rings). In transmitted light, the cataract has an uneven dark gray color against a pink background of the peripheral part of the pupil. With ophthalmoscopy, individual areas of the fundus are visible. Usually zonular cataracts are bilateral. Visual acuity can be significantly reduced, but improves with pupil dilation.
Treatment is usually surgical. The indication for surgery is visual acuity (less than 0.2).
Nuclear cataracts are somewhat similar to polar and zonular cataracts. However, after dilation of the pupil and especially during biomicroscopy, it is discovered that the opacification of the lens is not located superficially (as with polar) and not in the form of layers (as with zonular), but corresponds to the so-called embryonic nucleus of the lens. The remaining parts of the lens are transparent and in transmitted light a bright red reflex from the fundus of the eye is visible behind the clouded area. Ophthalmoscopically, the condition of the fundus is visible. Visual acuity is significantly reduced, increasing with pupil dilation. If visual acuity is below 0.2, treatment is surgical.
Cortical cataracts are discovered mainly by chance, when dilation of the pupil is required, and opacities are visible in the equatorial zone of the lens. Throughout the rest of the length, the lens is transparent, the fundus of the eye is clearly visible. Visual acuity is high. Treatment is usually not carried out.
Polymorphic cataract, as the name implies, is characterized by atypia, diverse opacities in various parts of the lens; opacities alternate with transparent areas through which the fundus of the eye is visible. Depending on the intensity and magnitude of the clouding, visual acuity decreases to varying degrees. Treatment is often surgical.
In order to identify and assess the severity of cataracts, every doctor must carefully examine the pupil area and accurately determine visual acuity. If it is impossible to do this (due to young age), we must remember that an indirect sign of low vision is the massiveness of the clouding (the pupil area is closed). Depending on the visual acuity of the better eye with correction, as well as the size and intensity of the clouding of the lens, the question of the feasibility, timing and methods of treating cataracts is decided.
Of utmost importance in assessing the severity of cataracts is not only the condition of the lens, but also the complications that it caused. Among them, nystagmus and strabismus are the most common. In addition, as a result of cataracts (especially membranous and complete), underdevelopment of the retina is possible due to insufficient light entering the eye, as well as so-called obscuration amblyopia, caused by inactivity of the eye. These dysfunctions of the visual analyzer require special, sometimes long-term and not always effective treatment after eliminating cataracts. Therefore, early diagnosis and appropriate treatment of cataracts in children (mydriasis 4-figure light) are very important for the prevention or reduction of these complications.
It is no less important to take into account concomitant pathological changes of a local nature or in the form of general severe suffering (diabetes, tetany, etc.). Naturally, the treatment of cataracts in such children is less effective in comparison with the treatment of simple and complicated cataracts.
To resolve issues related to the choice of methods and timing of treatment, as well as determine the prognosis and rehabilitation, it is necessary to formulate a diagnosis strictly in accordance with the classification: for example, bilateral congenital cataract, family hereditary, zonular, 2nd degree, complicated by strabismus, with concomitant aniridia or cataract of the right eye, congenital, intrauterine, complete, 3rd degree, simple.
In the first case, it is necessary to treat cataracts, strabismus, and aniridia, i.e. the prognosis is doubtful. In the second case, it is only necessary to remove the cloudy lens. A good outcome is beyond doubt.
COMPLICATED CATARACTS
Complicated cataracts are opacities of the lens that occur due to general diseases (diabetes, tetany, collagenosis, etc.), as a result of various eye diseases (myopia, glaucoma, uveitis, retinal detachment, retinal pigmentary dystrophy), poisoning (mercury, nitrates, uterine horns), protein starvation, ionizing radiation, trauma, etc. A number of authors call these cataracts complicated (complicated).
In children, the most common causes of sequential cataracts are trauma, uveitis, diabetes and tetany.
In adults, sequential (complicated) cataracts more often occur under the influence of high myopia, primary glaucoma and skin diseases (syndermatotic cataracts), etc.
Diabetic cataracts occur in 1-4% of children with diabetes.
The development of cataracts in children and adolescents with diabetes almost always indicates a severe course of the disease. However, such parallelism is not typical for older people with diabetes. Typically, diabetic cataracts in children are bilateral and rapidly progressing. The opacities are located in the form of individual gray lumps and are visible under the epithelium of the anterior capsule, and often under the epithelium of the posterior capsule.
The pre-cataract state of the lens in both children and adults is usually characterized by a change in clinical refraction. The lens is still transparent, and patients have worse vision into the distance. This condition gets worse quickly (weeks). So-called transient myopia appears, which can quickly disappear under the influence of insulin therapy. If treatment does not compensate for the diabetic process, then transient myopia, which, according to researchers, occurs due to swelling of the lens due to increased permeability of the capsule to aqueous humor, may give way to the appearance of opacities in the lens. Treatment is medicinal and surgical. Just as transient myopia disappears under the influence of rational treatment, diabetic cataracts can often resolve as a result of active antidiabetic therapy. If there is no effect from drug treatment, cataract extraction is possible.
Hypoparathyroid (tetanic) cataract, as the name suggests, occurs in early childhood in connection with tetany and spasmophilia. Opacities, as a rule, involve the superficial layers of the lens. If the disease ends quickly, then subsequently these clouded layers of the lens are pushed inward by newly formed transparent masses, creating a picture of a layered cataract with a transparent core, a layer of cloudy fibers and a transparent cortex of the lens. Treatment of such cataracts consists of early treatment of tetany (intravenous injections of 10% calcium chloride solution, taking thyroid medications), which can delay the development or progression of hypoparathyroid cataracts, and also promote the resorption of relatively fresh lens opacities. If drug treatment is ineffective and vision is poor, surgery is indicated.
UVEITIC CATARACTS
Uveitic cataracts most often occur in children due to inflammation of the choroid (uveitis, iridocyclitis of tuberculous etiology), as well as in rheumatoid arthritis (nonspecific infectious polyarthritis). Cataracts against the background of tuberculous uveitis are characterized by the fact that clouding of the lens begins from its posterior capsule and initially has a cup-shaped appearance. Subsequently, opacities also affect the middle layers of the lens. The anterior capsule and surface layers of the lens remain transparent for a long time. As accompanying changes, there are posterior adhesions of the iris, opacities in the vitreous body, and lesions in the fundus. Complications include strabismus and amblyopia. These cataracts are accompanied by a rapid and pronounced decrease in visual acuity. The process is often one-sided.
Cataracts in rheumatoid arthritis are manifested by opacities predominantly in the anterior part of the lens due to deposits and the organization of exudate on its capsule, and then the rest of its parts become cloudy. The process is almost always two-way. Cataracts with this disease occur in approximately 25% of cases. They can be complicated by strabismus and amblyopia. Concomitant changes in this type of cataract are characterized by band-like degeneration of the cornea, fusion and fusion of the pupil, opacities in the vitreous body and changes in the fundus.
Treatment of uveitic cataracts consists of the active use of absorbable agents (ultrasound, oxygen, ethylmorphine hydrochloride, etc.), the prescription of mydriatic agents under the control of intraocular pressure. If there is no effect and visual acuity drops below 0.2, cataract extraction can be performed. The operation is performed only in the absence of active inflammation of the eye and against the background of remission of the general process. Outcomes are not always favorable, both due to the presence of complications and associated changes, and as a result of postoperative exacerbation of uveitis (especially with Still's disease).
SENILE CATARACTS
The most common and common form of acquired cataract is senile (cataracta senilis). It usually occurs over the age of 50 years. These cataracts differ sharply from congenital ones in their appearance and development. They are always progressing. There are incipient, immature, mature and overripe senile cataracts.
Incipient cataracts (cataracta incipiens) appear, as a rule, from the periphery along the meridian plates of the lens. In such cases, the central part of the lens, its nucleus, can remain transparent for a long time, and vision suffers little. When examining the lens in transmitted light, against the background of the red pupil, radial or sector-shaped dark stripes are visible along its periphery, with their apex directed towards one of the poles. These opacities are located in the cortical layers. When illuminated from the side, opacities appear as grayish streaks. Sometimes they start from the core. In such cases, visual acuity decreases early. The periphery and cortical layers of the lens remain transparent for some time. The cloudy nucleus of the lens is visible in transmitted light in the form of a dark round disk with clear edges - this is an incipient nuclear cataract. In lateral illumination, nuclear cataracts may go undetected due to the transparent anterior cortices. We can assume that incipient cataracts are characterized by a drop in visual acuity to 0.3. Treatment of such cataracts begins with the prescription of agents that promote resorption: solutions of potassium iodide, cysteine, papain, ethylmorphine hydrochloride, vitamin complexes, etc. Drug treatment is carried out only as prescribed by an ophthalmologist. There are no indications for surgery, even if lens opacities are present in both eyes.
Immature cataract (cataracta nondum matura) differs from the initial one in that almost the entire lens appears gray and cloudy, but the clouding is uneven, has a pearlescent appearance, and is located in the layers of the lens adjacent to its core. The layers of the lens close to the capsule remain transparent. This can be judged by the wide shadow falling from the iris onto the cloudy layers of the lens when the eye is illuminated from the side. The shadow looks like a dark crescent-shaped strip between the pupillary edge of the iris and the cloudy layers of the lens. It is visible from the side of the pupil on which the light source is located. Vision at this stage of cataract can already be significantly reduced, up to 0.05. At this stage, with a bilateral process, there are indications for cataract extraction surgery with subsequent optical correction.
Mature cataract (cataracta matura) is a complete diffuse opacification of the entire mass of the lens. In this case, vision, as a rule, is reduced to light perception with the correct projection. Treatment of cataracts at this stage is carried out only surgically, even in cases of a unilateral process.
Overmature cataracts (cataracta hypermatura) occur when the cortex of the lens begins to liquefy and turns into a milky mass in which a yellowish core floats. The edge of the lens nucleus is quite clearly contoured. The nucleus shifts to the sides at different positions of the patient's head. This is the so-called Morganian cataract. Overripening may be accompanied by wrinkling of the lens, a decrease in its volume, which results in a number of symptoms: formal vision may appear (usually counting fingers at close range), the anterior chamber becomes deeper, the lens moves somewhat away from the iris and it, having lost support, trembles (iridodonesis ). A crescent-shaped shadow appears again between the iris and lens. Overmature cataracts are subject to extraction.
A special place in the pathology of the lens in children and adults is occupied by the so-called residual and secondary cataracts. To exclude arbitrary interpretation of these two types of cataracts, they should be characterized.
Residual cataracts are the remains of the cloudy lens capsule and the cloudy (organized, dense) remains of its masses. They occur either as a result of partial resorption of cloudy lens masses during drug treatment of sequential (perioral, diabetic, hypoparathyroid, etc.) cataracts, or after extracapsular cataract extraction. Vision is always reduced to one degree or another. Treatment consists of repeated operations, and the issue is decided depending on corrected visual acuity (less than 0.2).
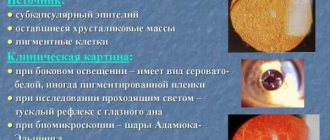
Secondary cataracts are cataracts that arose some time (months, a year) after extracapsular cataract extraction as a result of proliferation of the epithelium of the transparent equatorial part of the lens capsule. They look like the so-called Adamyuk-Elypnig balls. Under combined lighting or biomicroscopically, numerous balls of different sizes, such as soap bubbles, are visible in the area of the pupil. The fundus of the eye is difficult to see. When viewed with the naked eye, the pupil area appears dark, i.e., almost normal, but vision with maximum spectacle correction remains poor. Repeated surgical treatment is indicated taking into account visual acuity.
The diagnosis of residual or secondary cataract, according to the classification, can be as follows: secondary cataract of the right eye, second degree, complicated by high amblyonia, with concomitant vitreous hernia.
Lenticonus
Lenticonus is an abnormally changed shape of the surface of the lens. The condition is rare and is predominantly a congenital anomaly, although there are known cases of lenticonus that arose as a result of trauma. Pathology can be anterior, posterior and internal, usually being one-sided. Anterior lenticone is a cone-shaped, less often spherical, protrusion into the anterior chamber of the anterior surface of the lens. In posterior lenticonus, such a protrusion of the posterior lens surface faces the vitreous body. The internal lenticone is characterized by a cone-shaped protrusion facing the inside of the lens.
The pathogenesis of the abnormal condition has not been sufficiently studied. The origin of anterior lenticonus is associated with defects in lens lacing, abnormal attachment of zonular fibers and/or their complete absence, weak resistance of the tissue of the anterior lens bag, adhesion of the lens and the posterior surface of the cornea. With the development of posterior lenticonus, they speak of tension or rupture of the posterior capsule of the lens associated with the reverse development of the embryonic vitreous artery. In addition, the inflammatory genesis of the anomaly cannot be excluded.
Lenticonus can vary in the degree of protrusion and the diameter of its base. The protruding portion of the lens is usually transparent, so changes that resemble a drop in oil or kaleidoscopic phenomena are visible in transmitted light. If clouding of the lenticonus is observed, then in transmitted light a red fundus reflex can be detected against the background of which a dark disk is clearly visible. Throughout the rest of its length, the lens is transparent. Eye movements cause the anterior lenticone to move in the direction of movement, and the posterior lenticone to move in the opposite direction. There is some shadedness in the front Purkinje figures. In the area of the lenticone, high myopia is determined, while at the periphery of the lens emmetropic refraction, farsightedness or a high degree of myopia can be observed. The anomaly is always accompanied by decreased vision and can cause amblyopia.
Lenticonus is diagnosed when a characteristic clinical picture is identified and visual acuity is reduced. For anterior and posterior lenticonus, differentiated diagnosis is carried out with anterior and posterior polar cataract.
Therapeutic measures for lenticonus are limited to the prevention of amblyopia (medical dilation of the pupil, performing special exercises). With lenticonus of significant size with a sharp decrease in visual acuity, in some cases it becomes necessary to remove the lens.
Treatment of lens ectopia
Serious complications of lens ectopia are: glaucoma, uveitis, lens myopia, astigmatism.
To treat dislocation, the following methods are used:
- Spectacle correction, which is especially effective in the case of slight subluxation that causes astigmatism and in the correction of aphakia, when most of the axis remains without a lens in a state of physiological miosis.
- Surgical removal of a dislocated lens in the event of uveitis, cataracts, secondary glaucoma, or damage to endothelial tissue.
Results of the study using the method of A.A. Kozhukhova
Studies were conducted for a long time, during which a significant reaction of the patients’ pupils to light was noted, which meant that the diaphragm function of the organ was working well. Many zonular ligaments remained intact, and this served as an impetus for the development of a new, more advanced technique. The use of the treatment method described above in people with ectopic lens allowed us to achieve correct fixation of the lens
while maintaining
pupil function
. The duration of observation of patients ranged from one to four years.
According to the results of the study, the average visual acuity after surgery without additional correction was approximately 0.4-0.7, with correction - 0.7-0.9.
In addition, patients were given courses aimed at functional stimulation of the visual organ: eye massage, electrical stimulation, training on a special Amblyokor apparatus, as well as spectacle correction. After performing these measures, the observed patients showed a significant improvement in vision - its acuity without correction was up to 0.7, with correction - up to 1.0.
Microphakia
Microphakia is a congenital anomaly associated with stopping the growth of the lens, which is accompanied by a decrease in its size. Most authors are inclined to believe that it is constantly combined with spherophakia, although cases of isolated true microphakia are also known. As a rule, the lesion is bilateral. At the same time, microphakia can be observed as an isolated eye anomaly or combined with other constitutional anomalies. Spheromicrophakia is considered one of the typical manifestations of Marchesani and Marfan syndromes.
The anomaly is characterized by a family hereditary nature. Its occurrence is usually associated with a primary defect in the development of the ciliary girdle, degeneration and stretching of the zonular fibers.
Among the signs of microphakia, a decrease in the size of the lens, which has a spherical shape, very close attachment of the thinned fibers of the ciliary band to the equator, and iridodonesis are noted. When the pupil dilates, a golden ring can be visualized throughout, representing the equatorial edge of the lens. Often there is clouding of the lens and myopic refraction of the eye.
In microphakia, the lens may become pinched in the pupillary opening or prolapse into the anterior chamber. This leads to a sharp jump in intraocular pressure and is accompanied by pain. In this case, its urgent removal is necessary.
Symptoms of lens damage
Age-related changes make the structure of the nucleus and cortex of the lens more dense, which causes its weaker response to ligament tension and changes in surface curvature. Therefore, upon reaching the age of 40, it becomes increasingly difficult to read at close range, even if a person has had excellent vision all his life.
An age-related slowdown in metabolism, which also affects intraocular structures, leads to changes in the optical properties of the lens. It begins to thicken and lose its transparency. The images visible in this case may lose their former contrast and even color. There is a feeling of looking at objects “through cellophane film”, which does not go away even with glasses. With the development of more pronounced cloudings, vision decreases significantly.
The opacities inherent in cataracts can be localized in the nucleus and cortex of the lens, as well as directly under the capsule. Depending on the location of the opacities, vision decreases to a greater or lesser extent, faster or slower.
Age-related lens opacities develop quite slowly, over months and even years. Therefore, people sometimes do not notice the deterioration of vision in one eye for a long time. To identify cataracts at home, there is a simple test: look at a white and clean sheet of paper, first with one eye, then with the other, if at some point it seems yellowish and dull to you, then there is a possibility of developing cataracts. In addition, with cataracts, halos appear around the light source when looking at it. People notice that they see well only in bright light.
Often, clouding of the lens is caused not by age-related changes in metabolism, but by a long-term inflammatory process in the media of the eye (chronically ongoing iridocyclitis), as well as prolonged use of tablets or the use of drops with steroid hormones. In addition, many studies have confirmed that the presence of glaucoma makes the clouding of the lens faster and occurs much more often.
The cause of clouding of the lens can also be blunt trauma to the eye and/or damage to the ligamentous apparatus.
Recommended clinics for cataract treatment
“Dr. Shilova’s Eye Clinic” is one of the leading ophthalmological centers in Moscow, where all modern methods of surgical treatment of cataracts are available. The latest equipment and recognized specialists are a guarantee of high results. Go to the organization's page in the catalog >>>
“MNTK named after Svyatoslav Fedorov” is a large ophthalmological complex “Eye Mycosurgery” with 10 branches in various cities of the Russian Federation, founded by Svyatoslav Nikolaevich Fedorov. Over the years of its work, more than 5 million people have received assistance. Go to the organization's page in the catalog >>>
“Helmholtz Institute of Eye Diseases” is the oldest research and medical state institution for ophthalmology. It employs more than 600 people who provide care to people with a wide range of diseases. Go to the organization's page in the catalog >>>
Add a comment JComments
Spherophakia
Spherophakia is a pathology in which the lens has a spherical shape, usually combined with dislocations, microphakia, and general constitutional anomalies. It is a congenital family-hereditary anomaly, the occurrence of which is caused by defects in the development of the ciliary girdle.
Clinical manifestations of spherophakia are a spherical shape of the lens, increased depth of the anterior chamber of the eye, iridodonesis and myopia. It can often be accompanied by secondary glaucoma, subluxations and dislocations of the lens. Spherophakia cannot be treated. If complications are detected (glaucoma, dislocations), surgical intervention is indicated - antiglaucomatous operations, removal of the dislocated lens.
Lens abnormalities
Diagnosis of lens anomalies is based on anamnestic data, results of external examination, biomicroscopy, gonioscopy, visometry, tonometry, B-mode ultrasound (US), optical coherence tomography (OCT). On external examination of patients with microphakia, mydriasis is observed. The biomicroscopy method reveals an anomaly of the lens, in which the size, as well as the ciliary ligaments, do not correspond to the reference values. The depth of the anterior chamber of the eye increases, the walls become uneven, which is visualized during gonioscopy. In patients with macrophakia, OCT shows a significantly enlarged lens. The size of the anterior chamber of the eye of this lens anomaly decreases. The tonometry method determines the increase in intraocular pressure. Both micro- and macrophakia are accompanied by impaired accommodation. This leads to a decrease in visual acuity, which is confirmed by visometry.
In primary aphakia, using biomicroscopy, a complete absence of the lens in the cavity of the eyeball is observed. For differential diagnosis with a secondary form of the disease, OCT is performed. Unlike primary aphakia, with secondary aphakia an underdeveloped lens or parts thereof are visualized. In 30% of patients with coloboma, biomicroscopy reveals clouding of the biological lens. In the lower quadrant, a triangular, crescent-shaped or ellipsoidal defect is detected. In case of lens anomalies manifested by dislocation (luxation, subluxation), part of the biological lens is displaced into the anterior chamber of the eye, which is diagnosed by gonioscopy.
With lenticonus, biomicroscopy is used to determine the protrusion of one of the walls of the lens with complete preservation of transparency. In patients with the anterior variant of this lens anomaly, the anterior capsule becomes thinner, the number of epithelial cells decreases, and the cortex of the anterior layer bulges. The lens has the shape of a ball or cone. The movement of the eyeballs is accompanied by dislocation of the anterior lenticonus in the same direction. In the posterior form of this lens anomaly, a shift occurs in the opposite direction. The biomicroscopy method reveals thinning of the posterior capsule with an abnormal structure of the nucleus. With internal lenticone, the external structure of the lens is normal, but the fibers are cone-shaped.
Human diseases accompanied by lens luxation
Frequent cases:
- Marfan syndrome
- Homocystinuria
- Weil-Marchesani syndrome
- Sulfite oxidase deficiency
- Hyperlysinemia
Rare:
- Ehlers-Danlos syndrome
- Crouzon syndrome
- Refsum syndrome
- Knist syndrome
- Treacher Collins syndrome
- Sturge-Weber syndrome
- Conradi-Hünermann syndrome
- Pfoundler's disease
- Robin syndrome
- Wildervanck syndrome
- Sprengel deformation