Ophthalmologists at children's clinics, during a routine examination of almost every newborn (especially if it is the first-born), hear complaints of strabismus. More experienced parents treat episodes of uncoordinated eye movements much more calmly, understanding that at the stage of development of neuromuscular coordination, as they say, “anything can happen to babies.” In most cases, infant strabismus is transient, transient in nature and disappears without a trace over time. However, if by the age of six months the position of the eyeballs remains persistently incorrect and movements remain asynchronous, it is necessary to be examined and take adequate corrective measures.
Causes
The disease can be congenital or acquired.
The main causes of the congenital form.
- A rare genetic disease with an autosomal dominant pattern of inheritance. Distant relatives may be sick, but parents are usually apparently healthy. Males are more often affected. Combined with other eye anomalies and disorders of the cardiac, skeletal, and reproductive systems.
- Exposure to negative factors during intrauterine development that disrupt the formation of the eyelids and palpebral fissure. The second month of pregnancy is especially important - the time when the eyelids form, and the seventh, when they split into the upper and lower eyelids.
The acquired form is more common than the congenital form and develops against the background of chronic inflammatory diseases of the organs of vision. With long-term blepharitis, conjunctivitis, and trachoma, adhesions may form in the area of the outer canthus. A number of diseases of the endocrine, nervous, and muscular systems can contribute to the occurrence of pathology.
Variable convergent strabismus in children
Forms of unstable strabismus in children associated with accommodation problems:
- Divergent accommodative strabismus is a consequence of untreated myopia and occurs in school-age children from ten years of age. May be accompanied by “switching off” of the weak eye - amblyopia.
- Non-permanent convergent strabismus in children is non-accommodative - usually congenital, so it is not immediately noticed by parents. The child begins to grow, and the deviation of the eyes in different directions gradually increases.
The size of the squint angle is also taken into account when the baby is looking down or up. For example, with convergent strabismus, if the child looks down or looks at objects in front of him, the angle will decrease, and when looking into the distance or up, it will increase. This option is referred to as “A” syndrome. With divergence, everything is the other way around (“V” syndrome). And finally, the last option: an equal decrease in the angle of strabismus when looking in any direction (“X” syndrome).
Through the eyes of a baby. Features and possible problems
When looking at a newborn, parents look especially carefully at his eyes. Everyone is interested in whether the child’s eye color is “mother’s” or “father’s” and whether the baby sees well. The eyes cause great concern if there are any alarming symptoms: redness, hemorrhage, inflammation. And, probably, no other organ is associated with so many misconceptions and superstitions. How does the vision of a newborn actually differ from the vision of an adult, and what points should parents pay special attention to? How does a newborn's eye work? The eye of a newborn child, like the eye of an adult, resembles a camera and is part of a complex system called the “visual analyzer.” It includes the eye itself, special nerve fibers that carry visual information to the brain, and those parts of the brain that perceive and analyze what they see. The eye itself consists of an optical part (it can be compared to a lens), which includes a lens system: the lens and cornea, and a sensitive part - a special shell that lines the eye from the inside, the retina (“photo film”). The eye of a newborn is very similar to the eye of an adult, but it is not yet capable of full function. The baby's visual system is imperfect, and it will undergo rapid development. The vision of a newly born child is assessed at the level of the sensation of light; subsequently, visual acuity increases, increasing hundreds of times, and by the end of the first year of life it is 1/3-1/2 of the adult norm. The fastest development of the visual system occurs in the first months of a baby’s life. At the same time, the act of vision itself stimulates its development. Only the eye, onto the retina of which the surrounding world is constantly projected, is capable of developing normally. To do this, it is necessary that the optics of the eye be able to focus the image on the retina, and the retina must be able to perceive it. Any pathological processes that occur in utero, during childbirth or in the first day of life, which can disrupt the transparency of the media of the eyeball, the function of the retina and optic nerve, lead to a serious delay in the development of the visual analyzer. In addition to the fact that the eye develops functionally, it gradually increases in size. The eyeball of a newborn is approximately 6 mm shorter than the eye of an adult. This circumstance is the reason that a newborn’s eye is farsighted. As the eyeball grows, farsightedness gradually decreases. It is important to correctly assess the development of the visual analyzer over time. Vision in children is assessed by fixation and tracking reactions. In the first week of life, vision is assessed by the pupil's reaction to light. Short-term fixation appears from the second week of life; it can last only a few seconds and is only possible when an object is slowly moved in front of the child’s face. By the beginning of the second month of life, vision can be assessed as objective: at this time, stable fixation with both eyes is formed. At this time, parents note that the child begins to actively monitor objects and vision grows “week by week”; the child begins to react vividly to the mother. By 6-8 months, the child begins to distinguish simple figures, and from 12 months - drawings. Vision develops throughout childhood, and early detection of developmental abnormalities can often prevent serious pathology. Therefore, assessing the condition of the eyeball is a sacred duty of medical personnel and the baby’s parents. Pay attention to eyelash growth . It happens that eyelashes may not grow quite evenly and touch the child’s eyeball, which can lead to inflammation and damage to the cornea. The palpebral fissure of the newborn is narrow; see if there is a pronounced difference in the width of the slit of the left and right eyes, and whether the eyeballs stand out from the sockets equally. Notice if there is any difference in the size of the eyeballs. It is very important to remember that the eyes of a newborn are normally smaller than the eyes of an adult. Enlarged eyeballs may indicate a serious pathology - congenital glaucoma at 1 month (a condition in which the pressure of the eye increases, which leads to a rapid and irreversible decrease in vision). All visible structures of the eye normally look intact, the cornea is transparent. See if the pupils are the same size, what color the eyes are, if the coloring is uniform, if the eye color is the same. It is important to ensure that the pupil is round. It is necessary to evaluate the reaction of the pupil to light. This is quite difficult to do; It is better to use a point light source in a darkened room. When a beam of light hits the eye, the pupil should constrict. If something doesn't seem quite normal to you, contact your pediatric ophthalmologist. For early detection of pathology, scheduled consultations with an ophthalmologist are carried out. If there is a risk of developing any eye disease (for example, due to prematurity), then the first consultation is carried out in the maternity hospital. It is better to carry out routine consultations in children without obvious pathology at 1 month (the doctor examines the fundus and assesses visual functions), at 6 months (an assessment of the pupil’s reaction to light is added) and at 1 year.
I would like to dwell on certain situations when an urgent consultation with an ophthalmologist is necessary. 1. If your baby was born premature (especially if he received oxygen during the postpartum period). Such children have a high risk of developing severe pathology - retinopathy of prematurity, when the immature retina of the eye can detach due to excessive growth of blood vessels in the periphery of the fundus. The earlier the birth and the lower the birth weight, the higher the risk of developing retinopathy of prematurity. It is better to monitor such children in special centers where it is possible to treat this pathology. Retinopathy of prematurity can quickly lead to low vision and blindness, so a premature baby needs constant monitoring by a pediatric ophthalmologist during the first months of life. 2. If the size of your eyes seems large to you or your eyes are of different sizes (even a 1 mm difference is important). This may be an early sign of another pathology - congenital glaucoma, in which intraocular pressure rises so much that the eye begins to enlarge. First of all, an increase in the cornea (anterior transparent membrane) is noticeable; The depth of the space between the cornea and the iris (the one that determines the color of the eyes and forms the pupil) also increases. The border between the cornea and the white (sclera) becomes wider (more than 1 mm) and appears blurred. In more severe cases, clouding of the cornea is possible; it is formed due to the penetration of fluid from the eye under pressure into the thickness of the cornea. If you think your baby has any of these symptoms, contact your eye doctor immediately. 3.If the pupil acquires a grayish or whitish tint. If it is clear that the pupil is white, then there is an obstacle to the passage of light; such an eye will lag behind in development. It is necessary to exclude a serious pathology - congenital cataract. You can also indirectly evaluate the transparency of media when photographing when the “red-eye” effect appears: this occurs due to the reflection of light from the fundus of the eye. If the transparency of the media is impaired, this effect may be absent. If in a photograph one eye is a different color from the other, this should also be a cause for alarm. 4. If severe strabismus is noted. In the first two months of life, barely noticeable squint does not go beyond normal limits. This is due to the tone of the oculomotor muscles, immaturity of the cortex and oculomotor centers of the brain. However, in case of severe strabismus, you should consult an ophthalmologist. Speaking of photography. Flash photography is not harmful to the baby's eyes, but it can frighten him, so it is advisable not to photograph the baby too closely. In some cases, it may be not so much ophthalmologists who are against photography, but, for example, neurologists if the baby has a neurological disorder. Fortunately, severe congenital eye pathology is a relatively rare occurrence, and more often parents have to deal with other issues that relate to eye care: light conditions, choice of toys. About hygiene requirements The child's eye is sunny. This means that a baby’s need for light is greater than that of an adult. Good lighting is an important factor in eye development. It is better when the child is in a room with combined lighting (daylight and electric light). When a child is awake, he needs natural sunlight; if this is not enough, you can add electric lighting. A child sleeps better not in complete darkness, but in twilight light , which can be created using a night light. Outdoor walks are very important (even though the child usually sleeps outside). Good lighting is especially important in rooms with small windows and in cloudy weather. It is recommended to illuminate the room with incandescent lamps. Light sources that are designed according to a different principle (fluorescent lamps) can blink at the frequency of the electrical network, which is not very beneficial for the child’s eyes. Considering the fact that a child’s visual acuity is low, it is understandable why a higher level of illumination is required to perceive images of the surrounding world. Visual acuity is a function closely related to the perception of color. The same cells in the fundus of the eye, the cones, are responsible for both of these functions. Color vision develops along with visual acuity, and therefore it is desirable that the child is surrounded by bright colored objects. The cones, which are responsible for the perception of red color, are most abundant in the center of the retina, but there are almost no “blue” cones there. It is the center of the retina, as it develops, that has the greatest resolving power (sightedness). In a newborn baby, this center is in an undeveloped state. Therefore, the eye needs more red, yellow, green colors and their shades. Already in the first month of life, you can hang a garland in front of the baby. The elements of the garland should be arranged based on the child’s vision characteristics: they should not be very small; It is better to place a red element in the center, then orange (or yellow), green and blue at the edges. It is better to hang the garland rattle over the crib so that its main elements are located about 30 cm above the baby’s tummy. Proper care of the eyes of a newborn baby is also very important. Sometimes after sleep, discharge may accumulate in the corners of the eyes, which worries parents. If the discharge is white, it is, as a rule, desquamated epithelium of the conjunctiva and tear elements; The appearance of such discharge is normal. But purulent discharge is also possible (it has a yellowish tint). If there is no pathology, then cleaning the eyes should be done once in the morning after sleep, wiping each eye with a cotton swab dipped in water along the upper and lower eyelids in the direction from the outer corner of the eye to the inner. Each eye should be treated with a separate swab. If purulent discharge appears, you should consult a doctor. For treatment, as a rule, parents use a chamomile solution or tea leaves, but such solutions can sometimes cause allergies. Therefore, it is better to use a solution of furatsilin. The solution is stored for one day and a new one is prepared every day at the rate of 1 tablet of furatsilin per glass of boiling water. Use a moistened sterile cotton swab to wipe the eye, moving from the temple to the nose. You should not rub your child's eyes too hard: it is important to remember that during this procedure we wash away the tear film, which contains special antimicrobial agents. If the doctor has prescribed drops for your baby, sometimes there may be problems with instillation. The easiest way to do this is when the baby is lying on the changing table, and you, holding a bottle of drops, put your hand on his forehead and drop it into his open eye. If there is a need to open the eyelids (and this is especially difficult to do when the baby is crying), it is more convenient to do this with the thumb and forefinger, placing them at the very edge of the eyelids. Do not press hard on the eyeball - a slight force is enough to open the eyelids. The ointment is applied in a similar way to the lower eyelid; this is enough for the medicine to be evenly distributed over the entire surface of the eyeball. The baby will probably cry at the same time, so after applying the ointment, the baby’s eyes will be closed. Common misconceptions There is an opinion that a newborn sees everything upside down. However, modern data do not confirm this. The erroneous opinion is based on the fact that the image on the retina is inverted (the top changes to the bottom, the left side to the right), and this is how it can supposedly be perceived by a newborn. This is wrong. The first acts of short-term surveillance confirm this. Otherwise, the tracking response would be directed opposite to the direction of movement of the presented object. This is also evidenced by complex functional research methods. Superstitions also include statements that a baby should not be held in front of a mirror for up to three months, and that one should not approach the crib from behind (supposedly this provokes the development of strabismus). The color of a baby's eyes, which is often a subject of intense interest to the child's relatives and friends, is inherited from the parents and encoded in special genes. As a rule, eye color is determined at birth, but its shades can change in the first three months of life. Unfortunately, it is impossible to cover all the issues related to children's eyes. Yes, this is probably not necessary. If in any doubt, parents should consult a doctor and get advice. Bondar Vadim Andreevich, children's ophthalmologist. pediatrics.ru
31.10.2007
Vision of a newborn up to 1 year: norm and pathology
How to check a newborn's vision
Vision is the most important system of the human body.
It begins to develop in the child in the womb and continues to develop over the next few years.
Parents of a newborn, carefully examining his eyes, try to identify deviations in the baby’s vision. What is normal, and what changes in a baby’s eyes require prompt intervention?
Normal vision in a newborn
A newly born baby has congenital farsightedness, which occurs due to the fact that the size of the baby’s eye is somewhat flattened in anteroposterior size, as a result of which the image is projected further than the retina. A newborn has low visual acuity; the acuity index reaches 0.01 only at the end of the first month of his life.
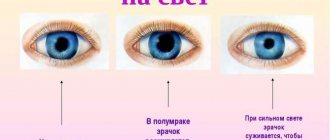
Reaction to light
The baby’s meaningful reaction to light appears from 2-5 weeks.
By this time, the child is able to highlight the luminous surface and fix his gaze on it for a short time. But the baby is not adapted to bright light, his light sensitivity is reduced. Under the influence of light, a newborn reflexively closes his eyes and throws his head back.
Colors
It is also normal that a newborn cannot distinguish colors. This ability appears in him only at the age of 2.5-3 months.
Strabismus
Almost all children in the first month of life have strabismus. This is also not a pathology, since the baby’s eyes have not yet learned to move and react to the world around them at the same time. However, strabismus can also be caused by serious reasons, which only a specialist can determine.
How and when can vision pathology in a newborn be detected?
The first examination of a newborn's eyes is carried out by a doctor in the maternity hospital. During this period, some congenital vision changes may be detected, for example, cataracts, glaucoma, ptosis, nystagmus.
Next, the child must visit an ophthalmologist every month, six months and a year.
The doctor will examine the baby’s fundus, examine the size and symmetry of his pupils, look at the reaction of the pupil to light irritation, and assess the state of visual function, as well as the tear ducts. The most serious diseases of the eyes of an infant, which initially do not have external manifestations, are optic nerve atrophy and retinopathy of prematurity.
Optic atrophy
In this case, the visual signal pathways leading from the eye to the brain are affected. With complete atrophy, vision is absent.
Retinopathy of prematurity
This disease is characterized by stopping the growth and normal development of retinal blood vessels, which can cause retinal detachment and loss of vision. These diseases can only be detected by an experienced ophthalmologist.
Eyeballs
From the first days of their baby’s life, parents should monitor his or her vision. First, you should pay attention to the size of the baby's eyeballs. Normally, they should be the same size, not too reduced or enlarged.
A one-month-old baby whose eyeballs are slightly enlarged and protruding requires an urgent examination by an ophthalmologist.
This feature can be caused by congenital glaucoma, as a result of which vision can be greatly reduced, up to absolute blindness.
Baby's pupils
Secondly, parents should evaluate the child's pupils. Their shape is normally round, the pupils are equal in diameter, and under the influence of light they should narrow. If a baby has any deviations from the normal state of the pupils, this is also a reason to visit an ophthalmologist unscheduled.
The color of both eyes should also be the same, but this will only become final by the age of three months.
At 2 months
Parents should monitor whether the baby, starting from the age of two months, is able to fix his gaze on a nearby object.
At 3 months
Can a three-month-old child actively follow a moving object?
At 6 months
At the age of six months, the child should already be able to distinguish simple figures, and at the age of one year he should be able to see drawings.
When to sound the alarm?
Parents should immediately show the child in the first months of life to an ophthalmologist if the following symptoms are detected:
- lack or slowness of tracking the movement of an object;
- the appearance of strabismus after three months of age;
- redness of the tunica albuginea;
- accumulation of pus on the eyelids and in the inner corners of the eyes.
However, do not panic if a specialist has identified a pathology in your baby’s vision: modern medicine allows you to restore impaired eye function in most cases.
© Ilyina Natalia, dealinda.ru
Source: https://Dealinda.ru/magazine/8/178/
Features of the congenital form
Congenital defects with this pathology:
- myogenic – eyelid dysplasia, including dystrophy of the orbicularis oculi muscle that lifts the upper eyelid;
- neurogenic – the formation of the oculomotor nerve is disrupted.
May appear as an isolated external defect or as part of a systemic lesion when other developmental stigmata are present:
- microphthalmos;
- wide-set eyes;
- microcephaly;
- syndactyly (fusion of fingers, the presence of a skin membrane between them);
- mental development disorders.
Classification of the congenital form of the disease:
- blepharophimosis and bilateral ptosis;
- telecanthus (wide-set eyes), ptosis;
- telecanthus, ptosis, epicanthus.
Convergent and divergent, alternating and concomitant strabismus in children
Clinically, there are two types of strabismus:
- Concomitant strabismus in children - in which there is a violation of symmetry, the correct position of the eyeballs without loss of eye movements in any direction.
- Unfriendly convergent alternating strabismus in children - it includes all other types of strabismus: various syndromes, variants of paresis and paralysis of the oculomotor muscles, improper attachment of the oculomotor muscles, anatomical defects in the structure of the tendons of the oculomotor muscles and many other pathological conditions, including those associated with damage to the central nervous system systems (primary hypoxia, cerebral palsy, primary intracranial hypertension, etc.).
Convergent concomitant strabismus in children is divided into several subtypes.
According to the degree of involvement of the eyes in the deviation of the visual axis:
- unilateral converging strabismus in children, i.e. only in one eye (monolateral);
- alternating from one eye to the other (divergent alternating strabismus in children).
By stability level:
- constant convergent strabismus in children (one and the same eye squints all the time);
- periodic or intermittent convergent strabismus in children (the affected eye squints from time to time).
The horizontal direction of the squinting eye is taken into account:
- Esotropia, or converging concomitant strabismus in children, is the diseased eye or both eyes slanting towards the bridge of the nose. With convergent strabismus, the child's eyes can be compared to the broken wheels of a car, facing inward. By turning the steering wheel, you can align only one of them, but not both at once. So the child has the opportunity to straighten only one eye, and the second is simply doomed to deviate.
- Exotropia, or divergent concomitant strabismus in children, is when the eyes look in different directions. This type can be intermittent, appearing only when the child is tired or sick, but over time, without treatment, the displacement becomes permanent.
Symptoms of the disease
The following symptoms are typical for superior orbital fissure syndrome:
- When the upper eyelid droops, ptosis . The palpebral fissure may close completely or partially.
- , paralysis of the eye muscles may occur . This condition is called ophthalmoplegia . A sick person has a lack of motor activity of the eyeball.
- The skin of the eyelids and cornea becomes less sensitive to tactile contact.
- After the lesion, the pupil may dilate ( mydriasis ). This condition is caused by a decrease in the amount of light, as well as poisoning by chemicals.
- With the syndrome, the retinal veins dilate , and changes occur in the arteries.
- As a result of damage to the trigeminal nerve, the cornea becomes inflamed . The process is called neuroparalytic keratitis and is sluggish.
- Sometimes there is the occurrence of bulging eyes - exophthalmos , in which protrusion of the eyeball occurs.
Signs of the syndrome may not be fully identified. It depends on the degree and amount of nerve damage. If the patient experiences two or more alarming signs, it is necessary to urgently visit a doctor for examination.
Why does a child have one eye larger than the other - ways to correct it
- By nature, the human face is asymmetrical .
- Natural asymmetry is almost invisible and does not cause any inconvenience to a person.
- Differences are especially common between the right and left eyes.
- Concern should arise if the asymmetry occurs unexpectedly or the differences are quite pronounced.
- Let's consider the most common pathologies that this symptom may indicate.
These include stye and conjunctivitis.
In this case, the disease can affect the mucous membrane of the eye, the tissue of the eyelid or the hair follicles of the eyelashes.
The tissues surrounding the diseased eye swell and prevent it from opening completely . If a person develops internal inflammation, a clear difference between the eyes will indicate a problem.
This disease can occur as a result of banal hypothermia or tooth root infection .
The pathology affects the facial nerves , resulting in obvious asymmetry of the eyes.
Poor blood circulation in the brain
A change in the shape of the eyes is a characteristic symptom of cerebrovascular accident.
Additional symptoms of brain problems include difficulty swallowing food and memory problems .
Various injuries
The eye can shrink as a result of various injuries and hematomas .
Violation of the rules for wearing contact lenses, contact with a foreign object on the mucous membrane, or rubbing of the eyelids can affect the size of the eye.
Allergic reactions
- The most common change in eye size occurs as a result of allergic edema .
- In some cases, the swelling can be so severe that the patient has difficulty opening his eyes.
- In addition, differences in eye size can indicate various internal diseases , ranging from kidney problems to cancerous tumors.
Eye asymmetry in a child: causes
The causes of ocular asymmetry in children are practically no different from the causes of pathology in adults . The most common of them include:
- kidney disease - in this case, the outflow of fluids from tissues is disrupted, swelling is formed, which often leads to similar problems;
- injuries, for example, as a result of playing sports;
- eye infections;
- disorders of the brain.
You should definitely contact your pediatrician in the following cases::
- if the defect occurred unexpectedly against the background of the child’s complete health;
- if, in addition to the difference between the eyes, the child experiences additional symptoms in the form of pain, itching or burning;
- if the difference between the eyes is large enough, or if the eye practically does not open.
Eye asymmetry in newborns
Only a pediatrician can determine the exact cause and make the correct diagnosis. However, we can give the most common reasons for different eye sizes, according to Dr. Komarovsky .
Congenital edema
The main symptom of this condition is a decrease in eye size.
After some time, the problem goes away on its own and does not require any outside intervention.
Heredity
If eye asymmetry was observed in the baby’s parents, grandparents or other close relatives, then most likely the difference between the eyes in this case is normal.
Torticollis
The problem can arise both during childbirth and in utero.
Birth injuries
Moreover, in addition to the difference between the eyes, the newborn will also experience other symptoms, ranging from frequent regurgitation to paralysis.
If there is a difference in eye size in newborns, the child should be shown to a pediatrician and undergo a comprehensive examination. It is important to take a general blood test and do an ultrasound of the brain .
Treatment of ocular asymmetry
Treatment of this problem depends entirely on the root cause that caused the pathology.
Thus, eye infections require consultation with an ophthalmologist , and a problem arising from a stroke requires treatment by a neurologist.
- undergoing a comprehensive examination by a therapist or pediatrician . In this case, the doctor conducts an external examination and asks the patient about the presence of accompanying symptoms;
- taking tests and undergoing an ultrasound examination.
Once the examination provides general information about the underlying cause, the patient's physician should make a referral to a specific specialist, such as a surgeon, nephrologist, or ophthalmologist.
A baby's eyes are different in size and open differently: symptoms of asymmetry
People only think their faces are symmetrical. In fact, the left side can be very different from the right. There are pictures that show completely symmetrical faces.
If you look at such a photograph, it immediately becomes clear that it is unnatural. In life, one eye may open more than the other. If this occurs in a child, parents may be seriously concerned.
Usually there is no reason for alarm, but in some cases various kinds of deviations from the norm, sometimes serious, are actually observed.
The child has different eye sizes
What to do if a baby's eyes are different sizes?
Reasons for different eye sizes
The sizes of both the eyes themselves and the pupils may differ. As a rule, the fact that one eye opens more than the other means that the baby has infantile palpebral ptosis, a condition in which the eyelids droop, closing the eyes. The baby cannot open its eyes completely.
Baby with facial asymmetry
This is a fairly serious disease that can subsequently lead to amblyopia, a condition in which the eye has difficulty seeing even though it looks normal. He is simply not stimulated enough and cannot express his full potential.
Different palpebral fissures in infants
If the shape of the palpebral fissure is different in newborns, this is usually a congenital condition. Caused by the fact that the muscles responsible for opening the eyelids are not developed enough.
Important! As a rule, the reason lies not in genetics, but in the characteristics of intrauterine development.
Why does one eye open more than the other?
If a newborn has one eye larger than the other, the reasons may be the following :
- Allergic reactions.
- Muscle diseases, such as Steinert's disease. This is a condition characterized by dystrophic changes in muscles, leading to a weakening of their functions. In this case, the symptoms of the pathology spread to other muscles. Intellectual impairment and arrhythmia are also observed. In children under one month of age, Steinert's disease rarely occurs. As a rule, she makes her debut at 10-20 years old.
- Progressive supranuclear palsy is an atypical symptom of parkinsonism, in which gaze movement is limited by more than 50%, it is difficult to keep the gaze on an object located on the right side of the visual field without turning the head. Also, an infant cannot turn his head at the same time as his eyes. The disease is accompanied by cognitive impairment. In addition to different eye sizes, infants may have problems with appetite.
- Horner's syndrome. This condition is characterized not only by drooping eyelids, but also by narrowing of the pupil, as well as its poor reaction to light. In addition, there is a retraction of the eyeball. The disease is combined with heterochromia - different colors of the iris.
- Injuries.
In some cases, the cause of ptosis in an infant may be an intracranial tumor or aneurysm. To exclude these dangerous conditions, it is better to go to the doctor immediately when these symptoms appear.
One pupil is larger than the other - disease or normal
Pupils of different sizes in babies - why is one larger than the other?
Usually a child's pupils are the same size, but in some cases one may be larger than the other. If this difference exceeds 0.4 millimeters, doctors state anisocoria. This symptom may be caused by one eye responding more to light and the other less.
Mom with baby
It is possible to say that different pupils are the norm only if the difference in pupil diameter does not exceed 1 millimeter. In this case, there is no threat to vision. Another important condition that distinguishes normality from pathology is the preservation of the pupil’s reaction to light.
The child should already be born with different pupils. If the condition develops suddenly, this may indicate pathology. The reasons may be as follows:
- Horner's syndrome.
- Pathology of the oculomotor nerve. May appear due to neuropathy or trauma.
- Trauma to the muscles of the iris caused by various injuries, including surgery. In this condition, there is a deterioration in the eye's response to light.
Swelling or concussion can also cause different eye sizes in an infant.
Important! Some of the reasons why a baby's pupils are different sizes and why the eyelids droop are the same.
To make sure that the differences between the pupils are not caused by pathology, an ultrasound is performed. The doctor needs to rule out hydrocephalus, decreased brain size, and other conditions.
Which doctor should I contact?
Why is one testicle larger than the other in a child - the norm and deviations
First of all, if there is asymmetry of the child’s eyes, you need to go to the pediatrician, only if the baby’s health is really unwell. There is no need to worry without reason. The child will only be infected by the bad mood of the parents.
Depending on the cause of the disease, it can be dealt with by neurologists, ophthalmologists, oncologists and other specialists. The parent is not able to independently determine which specialist to go to. The pediatrician will refer you to the right doctor if he suspects some kind of disorder.
Dr. Komarovsky about different eye sizes
Why red eyes in a newborn baby - what to do
Source: https://xn--80aadc3bb0afph1dp3h.xn--p1ai/zrenie/pochemu-u-rebenka-odin-glaz-bolshe-drugogo-sposoby-ispravleniya.html
Diagnostics
The following medical measures are carried out:
- genealogical history (questioning and examination of parents and relatives, especially in the male line);
- examination (mobility of the eyelids, size of the palpebral fissure, presence of scars or adhesions in the eyelid area).
To see better with ptosis, a person tenses the muscles of his forehead, tries to raise his eyebrows, throws back or tilts his head.
When looking straight, the eyelid is lowered; when looking down, it is located higher than the eyelid of the healthy eye.
Signs and symptoms of strabismus in children
Any deviation of the eye from the visual axis in a baby cannot be considered normal.
Signs of strabismus in a child appear due to the fact that he not only has problems focusing, he sees a double image.
What does the brain do in this case? It “turns off” the chaotic signals coming from the diseased eye, as a result the baby begins to see with only one eye and is no longer able to perceive a full three-dimensional picture. There is no symmetry of the visual axes - no binocular vision, no three-dimensional, three-dimensional image!
Children with strabismus may develop a curvature of the neck: in an attempt to focus their gaze, they are constantly forced to tilt their head to the side. Lack of load on the oculomotor muscles of the squinting eye reduces visual acuity and makes it “weak.”
What may be associated with the development of strabismus? There are many reasons: congenital defects in the development of the extraocular muscles or acquired problems - decreased visual acuity in one eye, diseases of the retina or optic nerve.
The symptoms of strabismus in children are not always visible to a non-specialist: sometimes the angle of deviation of the squinting eye is so small that it seems as if the baby’s vision is fine. What should you pay attention to?
If you suddenly see that your child is closing his eyes or covering one eye with his hand in order to get a better look at the toy or you, consult a doctor immediately.
Symptoms for different types of strabismus differ slightly from each other, but if you have the following signs, do not delay a visit to the clinic:
- one eye or both constantly or alternately deviate to the side;
- the baby tilts his head to the side, trying to cover the whole picture with the field of vision of his healthy eye (while only squinting one eye);
- the child complains of fatigue, headache, dryness, burning eyes, double vision.
Eyes of different sizes in children
As mentioned above, facial asymmetry is a completely natural phenomenon. Therefore, if one eye is smaller or larger than the other in a baby, there is no need to worry ahead of time. If the pediatrician examined the child and said that he is healthy, then he is. Most likely, with age, it will become less noticeable that the child has eyes of different sizes. So it's best to just wait.
At the same time, different eye sizes in infants may indicate genetic diseases, congenital malformations or birth injuries. In this case, the child has other serious abnormalities. As a rule, they are identified by a pediatrician during an examination.
If a child has one eye open much more than the other, it is better to show it to a doctor so that he can find out the reason. It is possible that the baby does not open his eye well due to inflammation or a neurological disorder.
Different pupils in babies
If a child has pupils of different sizes, then for preventive purposes it is necessary to consult a specialist. Children are able to report other visual disturbances.
These include:
- visual impairment;
- objects became blurry;
- nausea;
- vomit;
- darkening of the eyes.
Serious processes begin to occur when a child experiences the urge to nausea and vomiting. Symptoms can overlap with others and parents mistakenly perceive this as another disease.
The pediatrician will conduct an examination and may refer you to an ophthalmologist. In some cases, they immediately contact the right specialist.
The hereditary manifestation of unequal pupil size appears after childbirth. Over time, this phenomenon passes. It takes at least 5 years to restore the size. In individual cases, different pupil sizes may remain forever.
When diagnosed, a child may be diagnosed with Horner's syndrome. Along with anisocoria, there is a drooping eyelid above the eye, where the pupil is narrow.
Reasons for different pupils in infants
In infants, the phenomenon of different pupil sizes occurs due to a disorder in the development of the autonomic nervous system. In other cases it refers to a hereditary pathology. Uneven pupil sizes could appear suddenly.
This portends the presence of the following pathologies:
- benign or malignant brain tumor;
- vascular aneurysm of the brain;
- injury;
- encephalitis.
Causes of different pupils in adults
Adults are no less susceptible to the phenomenon of different pupil sizes than children. The reasons for its appearance are similar to those for children.
These may include the following health problems:
- brain aneurysm;
- brain injury and possible bleeding;
- pathologies and diseases of the organ of vision;
- migraine with severe headache;
- glaucoma;
- medications;
- formation in the lymph node (Horner's syndrome);
- Roque's syndrome;
- injury to the eye and eye muscles responsible for pupil size;
- cerebral circulatory disorders;
- thrombosis, especially in the carotid artery;
- eye diseases that lead to inflammatory processes;
- hereditary pathology.
Developing myopia is considered a common cause of anisocoria. During this process, the pupil dilates in the eye, which begins to see poorly.
If anisocoria continues for more than a month in an adult, Holmes-Eydie syndrome develops. The pupils do not react to light and dilate slowly. The development of the disease is associated with the use of eye drops – pilocarpine. People do not observe and do not feel discomfort. Anisocoria may be caused by compression of the optic nerve.
This pathology is accompanied by:
- ptosis;
- diplopia;
- paresis.
To identify this process, you need to observe the eye. The pupil has a slow reaction to light.
Anisocoria occurs due to the use of medications. One pupil has a slow reaction to light. At the same time, there is no narrowing. If the sphincter or optic nerves are injured, one pupil can become enlarged.
The appearance of different pupil sizes is observed due to diseases.
These include:
- iritis;
- rubeosis of the iris;
- iridocyclitis.
If anisocoria appears suddenly, you should consult a specialist. It is worth paying attention to how long this phenomenon has been occurring. Along with different pupil sizes, other symptoms may appear. They should be taken seriously.
Methods for treating the phenomenon of anisocoria
After establishing an accurate diagnosis, specific therapy is prescribed. Medications are recommended after identifying the cause of different pupil sizes.
These include:
- migraine medications;
- corticosteroids – prescribed to reduce swelling of the brain;
- medications for seizures;
- antibacterial drugs - used for meningitis;
- anesthetic drugs for diseases and pathologies;
- antitumor agents.
The recovery process for different pupil sizes depends on the doctor. If he makes an accurate diagnosis, the treatment will be effective. Anisocoria is a symptom of an underlying disease. Therefore, you should get rid of the root cause.
To eliminate different pupils after eye injury, use:
- Irifrin, Atropine - relax the muscles of the iris;
- Cyclomed, Midriacil - used to dilate the pupil, often prescribed during myopia.
Irifrin AtropineCyclomed Mydriacyl
If a person is diagnosed with brain hematomas or injuries, then physiotherapy is prescribed. This therapy is aimed at restoring damaged cells.
Treatment methods have the following positive effects:
- Magnetic waves improve blood circulation;
- Infrared radiation relieves muscle spasms;
- Electrical stimulation helps in improving tissue and cell regeneration.
Traditional methods
Sometimes traditional methods are used to treat anisocoria:
- Aloe juice helps relieve inflammation. Used as a lotion on the eyes.
- An infusion is made from carrots and nettles. For cooking you need 2 tbsp. l of raw materials brew 1 l. hot boiling water. The product needs to brew and cool for 2 hours. The drink is then drunk throughout the day. Therapy can be repeated the next day if necessary.
A specialist needs to prescribe the correct treatment to get rid of the disease. Certain cases of anisocoria require surgery.
Complications that accompany deviation
- If anisocoria is pathological, then this portends an eye or brain disease. Without proper treatment, complications may occur. Certain cases can be fatal.
- The sign of different pupil sizes occurs due to injury to the eye muscles or nerve endings.
When a person does not deal with this problem in time, inflammation of the iris may occur. This complication occurs in adults under 40 years of age. - The pattern of the iris can change during complications of anisocoria.
Visual acuity decreases and blurriness occurs. The person begins to feel a headache. It radiates to the temple area. After the chronic course of the pathology, atrophy of the eye occurs. - Anisocoria without proper treatment can lead to strabismus.
This can often be found in children who have impaired functioning of the eye muscles. The squinting eye does not participate in the process of vision. Treatment will require certain medications and special glasses. To avoid serious consequences of unequal pupils, timely assistance from specialists is necessary.
Preventive measures for the phenomenon of anisocoria
The symptom of unequal pupils does not require special preventive measures. To reduce the risk of developing anisocoria, it is recommended to use protective equipment when playing sports. It is necessary to monitor your health. If there are any deviations, seek help immediately.
In some cases, the problem does not pose a health threat. Experts recommend limiting yourself to maintaining a healthy lifestyle. To strengthen the body, it is recommended to take vitamin and mineral complexes.
Anisocoria is considered a symptom that needs to be monitored.
After all, unequal pupil sizes can be not only a physiological feature, but also a harbinger of the development of serious diseases.
If this symptom occurs and is accompanied by additional signs, then urgent help from a specialist is needed. It should be remembered that self-medication of eye diseases can lead to complications and other negative consequences.
Ophthalmologist of the highest category and author of the website vizhuchetko.com. For more than 10 years, she has been successfully helping adults and children fight eye diseases.
Possible reasons
Heredity is one of the factors influencing changes in pupil size. If you have a genetic predisposition to this manifestation of individuality, then you should be less enthusiastic about suspecting hidden diseases.
Some medications can also affect the pupils, in particular, inhalers for asthmatics and various kinds of drops. Naturally, after detecting such a reaction, you should stop using the drug.
Pupils may become different sizes as a result of blunt or cutting trauma to the eye. This may be due to damage to the muscles responsible for accommodation - narrowing and widening of the opening in the iris. Asymmetrical pupils appear when the iris is inflamed - iritis leads to narrowing of one of them in the affected eye.
Angle-closure glaucoma, on the contrary, leads to widening of the iris opening and cessation of response to stimuli. The reasons may lie in malfunctions of the optic nerves. Then the transmission of the signal about the presence or absence of light is disrupted and the pupils do not react. Muscle atrophy is a possible cause of size differences.
Anisocoria as a symptom
By analyzing the size of the pupils, one can assume the presence of tumor processes, aneurysms, vascular and infectious diseases. Temporal arteritis and diabetes mellitus are also possible causes of asymmetry.
https://www.youtube.com/watch?v=CANtKcwoyu4
If anisocoria intensifies in the dark, it may be associated with Horner's syndrome. It usually manifests itself when the sympathetic pathways in the cervical bone marrow, hypothalamus and brain stem are damaged.
Possible reasons are very varied. These are tumors, inflammatory processes of the central nervous system, stroke, trigeminal neuralgia, migraine, alcohol intoxication. And many more.
In short, you cannot make a diagnosis yourself.
The reasons can only be determined by a doctor after conducting a series of tests. Therefore, if noticeable anisocoria appears, it is necessary to contact specialists - a neurologist and an ophthalmologist.
When you visit your doctor, you may receive a referral for the following procedures: general and biochemical blood tests, computed tomography of the brain, cerebrospinal fluid examination, x-ray examination or MRI. They are necessary to exclude or detect the diseases listed above and some others. It is possible that nothing terrible will be discovered, then the unusual pupils can be considered a genetic feature.
Asymmetry may be accompanied by other symptoms:
- headache;
- blurred vision, double vision;
- nausea, vomiting;
- torticollis;
- trembling, fever, increased temperature;
- photophobia.
If these accompanying signs of disorders are detected, you should consult a doctor immediately. You especially need to be attentive to such manifestations in a child. The younger he is, the less you can learn about his feelings from the baby himself. And the more carefully parents need to monitor the child’s well-being.
Anisocoria in a child
Different sizes of iris holes can be observed quite often in infants. Most often this goes away on its own, without treatment. But still, consultation with a neurologist is necessary.
If there are no other violations, the child is usually released before reaching 6 months.
If the pupil sizes are not equalized before this, then a more thorough examination is prescribed, including the tests described earlier.
In addition to the diseases already listed, a birth injury in the neck area can be a cause for anisocoria in a child. In such cases, treatment is prescribed immediately after birth. Infections (for example, meningitis), increased intraocular pressure, head injuries - all of this can serve as a prerequisite for the disorder.
Thus, anisocoria may indicate the presence of a large set of diseases or be just a feature of the body. In any case, only a doctor can tell you definitively about this.
Paying attention to your body will allow you to maintain health for many years. Do you agree? We look forward to your comments on this issue.
Take care of your health and listen to your body, internal and external symptoms of disorder.
Source: https://babytwins.ru/raznye-zrachki-u-grudnichka/
Indications for ultrasound of the eyes
- clouding of optical media;
- intraocular and intraorbital tumors;
- intraocular foreign body (its identification and localization);
- orbital pathology;
- measurement of parameters of the eyeball and orbit;
- eye injuries;
- intraocular hemorrhages;
- retinal disinsertion;
- pathology of the optic nerve;
- vascular pathology;
- condition after eye surgery;
- myopic disease;
- evaluation of ongoing treatment;
- congenital anomalies of the eyeballs and orbits.
Creating an almond-shaped eye
While Easterners try to get rid of some ethnic characteristics, many European women strive for the opposite effect. They want to give their eyes an “oriental” flavor, which is associated with mystery, femininity and sexuality.
The problem is successfully solved by an operation aimed at creating an “almond-shaped” eye shape. To do this, the surgeon just needs to slightly raise the outer corners of the eye and, depending on the initial data, change the height of the palpebral fissure. Women with naturally large and round eyes get excellent aesthetic results.
Congenital and acquired strabismus of one or both eyes in children
Strabismus in children, or strabismus , is a disease in which one or both pupils deviate to the side when trying to fixate on objects.
This results in a violation of binocular or stereoscopic vision, which brings not just discomfort, but a serious decrease in the quality of life. The child sees the world as flat and unvoluminous.
Many people mistakenly believe that acquired strabismus in children is only an external defect. That is, the eye squints to the side, well, he sees, right? This is a deeply erroneous opinion. Strabismus reduces visual acuity, as it is a direct consequence of a violation not only of perception, but also of the analysis of visual information.
A child with strabismus does not see a full-fledged three-dimensional picture because the connection between both eyes and the work of the extraocular muscles are disrupted.
As you remember, two versions of the picture simultaneously enter our eyes, and then they are processed in the visual analyzer of the brain; where the “merging” of two images occurs and the formation of one holistic image.
There are three levels of two-eyed perception, which are impaired in congenital strabismus in children to varying degrees depending on the type of disease and the duration of its existence. In this case, one level is built on another. And only their simultaneous correct functioning ensures normal vision.
- The lower level is bifoveal fusion: the image falls into the center of the zone of visual cells, and the picture from the left and right eyes is initially combined in the head into a single visual image.
- Intermediate level - binocular vision: the ability to clearly see the image of an object with both eyes at the same time. The operation of this level is checked in the following way: if a person is presented with certain colored sources on a plane (usually green and red), he should be able to see them simultaneously, looking at the plane through appropriate optical filters, the color of which matches the color of the presented sources .
- The highest level is stereoscopic vision: the ability to see the world in volume, in SD format.
If a person has a dysfunction at the lower level (bifoveal fusion), then none of the subsequent levels will work: neither binocular vision nor the ability to visually perceive a three-dimensional image will be able to function. Conversely, without stereoscopic vision, a child will live in a flat world. Accordingly, each of these levels must be developed at a certain stage of treatment of such a formidable disease as strabismus, or other forms of oculomotor pathologies.
Strabismus can affect one or both eyes at once; sometimes a child’s eyes squint alternately. Deviation is possible in any direction: up or down, towards the nose or temple.
Look at how strabismus manifests itself in children in the photo, which illustrates typical symptoms: