Causes of postthrombotic retinopathy
The risk of blood clots increases with arterial hypertension, diabetes mellitus, atherosclerosis, heart rhythm disturbances, as well as with the activation of chronic infectious diseases. It increases many times in the case of increased blood clotting and in the presence of systemic autoimmune diseases. The cause of thrombosis is often the inflammatory process, neoplasms and traumatic lesions of the eyeball, as well as glaucoma.
When blood flow through an arterial vessel is disrupted, acute retinal hypoxia develops. In the case when a vein is thrombosed, the pathogenesis of the changes is more complex:
- as a result of blood stagnation, vascular permeability is impaired;
- blood leaves their bloodstream;
- swelling and hemorrhage occurs in the retina of the eye;
- after some time, new pathological vessels begin to grow.
Reasons for development
Postthrombotic retinopathy can be provoked by the following factors on the human body:
- blood pressure surges;
- atherosclerosis;
- diabetes;
- the presence of a focus of chronic infection;
- arrhythmia;
- autoimmune pathologies;
- smoking;
- uncontrolled use of medications;
- alcoholism;
- disruption of the production of sex hormones;
- heart valve defects;
- polycythemia;
- obesity;
- inactive lifestyle;
- frequent stress;
- malignant neoplasm;
- glaucoma;
- injury.
The pathology is dangerous because a person can become blind.
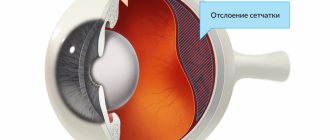
The occurrence of post-thrombotic retinopathy is caused by blockage of the arteries supplying the eye by a blood clot formed on the wall. As a result, ischemia of nerve endings and atrophy of the optic nerve head develops, which subsequently leads to loss of vision and disability of the patient. In this case, the pathology can affect either one or both eyes.
Symptoms of postthrombotic retinopathy
Retinal vascular occlusions are often the cause of vision loss. This occurs especially often in elderly people, patients suffering from arterial hypertension, atherosclerosis or diabetes mellitus. In most cases, unilateral vision loss occurs suddenly. Often older patients discover this after some time. In order to find out the cause of the disease, it is necessary to establish concomitant pathology. Often, vascular diseases of the brain and heart are diagnosed, which previously did not manifest themselves in any way.
In the case of thrombosis of the central retinal artery, complete blindness of the corresponding eye occurs in a matter of minutes. If there is thrombosis of a branch of the central retinal artery, then a certain field of vision is lost.
Thrombosis of the central retinal vein manifests itself as a gradual loss of vision over several days. This depends on the severity of the venous occlusion. The prognosis may vary depending on the location of the lesion and the area of retinal ischemia.
With non-ischemic occlusion, in most cases, visual acuity remains above 0.1, in the case of ischemic occlusion, only counting fingers in the face, or even lower. In 1/5 of the patients, progression of non-ischemic central vein occlusion to ischemic is observed.
Treatment of pathology
Heparin will help cope with the cause of this condition in humans.
Therapy for postthrombotic retinopathy involves eliminating the cause that could trigger the disease. It is also important to eliminate hemorrhages, restore normal blood flow in the retina and thereby improve the nutrition of the organ of vision. It is necessary to relieve swelling and prevent the formation of new blood clots. The use of fibrinolytics and antiplatelet agents such as Heparin or Nifedipine is indicated. Correction of hypertension involves the use of beta-blockers, ACE inhibitors and diuretics. Local hormonal anti-inflammatory therapy is also indicated; antispasmodics will help relieve pain. Angioprotectors and vitamin-mineral complexes will prevent the progression of the disease. Surgical treatment methods are also used, the use of laser, plasmapheresis and ultraviolet irradiation will be useful.
Medications
Treatment for retinopathy involves stabilizing blood pressure within normal limits. For this purpose, diuretics Furosemide or Hydrochlorothiazide are used. Beta-blockers Metapralol and Bisoprolol are indicated. An ACE inhibitor, such as Lisinopril, calcium channel blockers such as Verapamil and angiotensin receptor blockers are also used. Alpha-blockers Prazosin or Doxazosin are sometimes used. Fibrinolytics, direct and indirect anticoagulants or antiplatelet agents will help prevent the formation of blood clots. Steroid hormones and agents that improve local microcirculation in the tissues of the eyeball are used.
Angioprotectors and multivitamins are used.
Impact of massage
In the first hours after the development of the pathological condition, a person is allowed to do a light eye massage.
This treatment method is used as an emergency aid and is used if no more than 6 hours have passed since the blockage of the vessel. With the help of light pressing or kneading movements, it is possible to restore normal blood flow in the vessels of the eyeball. These actions must be careful not to cause injury to the organ of vision.
Laser Application
Laser therapy is a physiotherapeutic treatment method and is used only in combination with other means. It helps improve nutrition of the eyeball and retina, has an anti-inflammatory, analgesic and regenerating effect. Laser treatment accelerates the regeneration of tissues damaged due to hypoxia and is therefore well suited for eliminating the consequences of post-traumatic retinopathy.
Diagnostics
During an ophthalmological examination with occlusion of the central retinal artery, the following pathological changes are visualized:
- the arteries are sharply narrowed, thread-like, with segmental blood flow;
- ischemic retina (pale and edematous);
- against its background, the presence of a bright red spot is determined in the macula (the “cherry pit” symptom).
Central vein thrombosis has slightly different ophthalmological signs:
- the retina is swollen;
- veins are dilated, full-blooded;
- they show signs of stagnation;
- “crushed tomato” symptom (streak-shaped hemorrhages).
Somewhat later, with the development of postthrombotic retinopathy, “old” hemorrhages, swelling and changes in the macula, and new pathological vessels can be identified. Microaneurysms and hard exudates appear in place of old arteries and veins.
The research package includes the following diagnostic procedures:
- visual acuity test;
- fluorescein angiography;
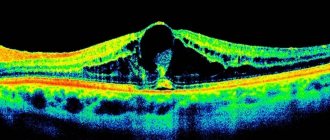
- optical coherence tomography;
- visual field assessment.
Consultations with related specialists are also often necessary.
Diagnostic methods
Fundus ophthalmoscopy reveals the presence of a red spot in the macula area to confirm the diagnosis.
The presence of retinopathy associated with thrombosis can be suspected by the presence of symptoms characteristic of this pathology in the patient. To confirm the diagnosis, it is recommended to conduct an ophthalmoscopic examination of the condition of the fundus, in which a characteristic red spot will be present in the area of the macula. Fluorescein angiography or injection of a contrast agent into the retinal vascular bed is also used. These methods make it possible to clarify the features of the course of the disease and identify the stage of the pathological process. It is recommended to conduct a visual acuity test and visual field assessment, as well as clinical and biochemical blood tests.
Treatment methods for postthrombotic retinopathy
The main goal of conservative treatment for central retinal vein occlusion is to restore blood circulation and prevent new thrombus formation. For this, the following medications are prescribed:
- drugs that reduce retinal swelling;
- thrombolytics;
- antiplatelet agents;
- means to improve microcirculation (pentoxifylline);
- means for strengthening the vascular wall;
- glucocorticosteroids;
- antispasmodics;
- multivitamins.
If there is pathological growth of newly formed vessels, laser coagulation of the retina is performed to eliminate edema and close ischemic areas, and intravitreal administration of anti-VEGF drugs is performed to suppress the growth of new vessels. For fresh retinal vein thrombosis, the Ozurdex hormonal implant is administered intravitreally.
Patients who have suffered thrombosis of the central retinal vein are recommended to regularly monitor the level of intraocular pressure, since pathological newly formed vessels tend to appear in other structures of the eye, and not just on the retina. If neovascularization of the anterior chamber angle occurs, the outflow of intraocular fluid becomes difficult. This leads in some cases to intraocular hypertension and the development of glaucoma.
Treatment
Therapeutic measures for occlusion of the central vein are aimed at restoring blood circulation in the retinal vessels and preventing new formation of blood clots. For this purpose, thrombolytics, drugs to reduce retinal edema, antiplatelet agents, agents that activate microcirculation (pentoxifylline), steroids and agents that help strengthen the walls of blood vessels, vitamins, and antispasmodics are prescribed.
To stop the growth of newly formed pathological vessels, laser coagulation is performed. Elimination of retinal edema and restoration of ischemic areas is ensured by intravitreal administration of anti-VEGF drugs, which are aimed at suppressing the growth factor of dysfunctional vessels. If retinal vein thrombosis is still fresh (up to 3-4 months), an excellent effect can be achieved by intravitreal administration of the hormonal implant Ozurdex (dexamethasone).
With thrombosis of the central retinal vein, in the future, patients need to monitor the condition of the retina and the level of intraocular pressure on a regular basis. This is caused by the risk of reappearance of pathological newly formed vessels on the retina, as well as in other ocular structures. If neovascularization affects the angle of the anterior chamber, the outflow of intraocular fluid is hampered, which can cause an increase in intraocular pressure - the development of glaucoma.
The specialists of our clinic have enough knowledge and practical experience to restore partial vision even in the most complex cases of retinal vascular occlusions. Thanks to the technical equipment of the center and the availability of all necessary drugs, patients have the opportunity to receive a full range of therapy that meets high international standards without the need for treatment abroad. Also, we accept patients for dispensary services and make every effort to ensure that such an eye catastrophe does not happen again, and other ophthalmological diseases are detected and eliminated as soon as possible.
Diagnosis of retinopathy
When the first symptoms of the disease or discomfort in the eyes appear, you should definitely consult an ophthalmologist. He will collect a history of the disease and examine the eyes and fundus using an ophthalmoscope. The doctor will also conduct a differential diagnosis with other pathologies and make a preliminary diagnosis. If necessary, he will order additional studies.
For successful treatment of retinopathy, you need to consult a specialist in time for diagnosis and diagnosis.
Additional research methods:
- Visometry - allows you to determine visual acuity.
- Perimetry - used to identify scotoma.
- Biomicroscopy - used to examine the vitreous body.
- Fluorescein angiography shows the condition of the blood vessels.
- Ultrasound of the eyes.
- Optical coherence tomography of the retina.
Features of the manifestation of postthrombotic retinal damage
In the initial stages of the disease, symptoms do not appear, and patients do not consult a doctor on time. Retinopathy is detected during medical examinations. Since postthrombotic retinal damage is progressive, it is important to identify the disease at an early stage and begin treatment. At this stage, the outcome of the disease is favorable.
Stages of the disease and their symptoms
| Prethrombosis stage | Patients do not feel any discomfort. When examined, dilated, tortuous and stagnant veins are revealed in the eye. Isolated hemorrhages also appear, which lead to a temporary deterioration in vision, but patients do not pay attention to this. |
| Thrombosis of the central retinal vein | Vision begins to rapidly deteriorate. Patients note the appearance of a “veil” before the eyes, the presence of a foreign body, and double vision of objects. On examination, vitreous hemorrhages and edema are visible. |
| Stage of postthrombotic retinopathy | Identification of old hemorrhages and newly formed vessels. All this has a bad effect on visual acuity. Its complete loss may occur. |