One of the most serious and dangerous pathologies of the visual system is atrophy of the iris. Ophthalmologists call this disease essential mesodermal progressive iris dystrophy. We will talk about what this disease is and how it is treated in this article.
In this article
- First noticeable symptoms
- Why does iris atrophy occur?
- Who is more susceptible to iris atrophy?
- Why does glaucoma develop in parallel?
- Conservative treatment methods
- In what cases is surgery necessary?
- Types of surgical interventions
The development of iris atrophy, as a rule, is not preceded by anything. In simple terms, illness can come out of nowhere. It begins to progress without any symptoms or signs of inflammation, and therefore most people are not aware that any changes are occurring in the structure of their eyeball. Before the initial signs of the disease appear, the patient can only notice discomfort in the eyes or headaches.
In addition, even in the presence of pronounced changes in the cornea, visual acuity continues to remain high. In most cases, this is the main reason why many patients are in no hurry to see an ophthalmologist.
First noticeable symptoms
For a long time, atrophy of the iris of the eye occurs unnoticed by the patient; the symptoms of the disease still make themselves felt, but after a certain time. The first thing you should pay attention to is a change in the natural color of the iris and deformation of the pupil. When conducting a biomicroscopic examination at this stage, specialists can already detect an increase in the vascular network of the limbal pattern, an increase in venous trunks and petechial hemorrhages, which, by their nature, although insignificant, provoke the appearance of specific points - petechiae. In addition, small, pigmented, grayish deposits may appear on the posterior surface of the cornea. The permeability of the corneal endothelium, the layer of cells covering the blood vessels, is disrupted, and the eye muscles lose their original shape.
Subsequently, the sensitivity of the cornea begins to decrease, and changes in the color of the iris become more noticeable. In some cases, the color changes in the direction from the limbus to the pupil. This indicates damage to the iris stroma. The next stage in the development of the disease is the transition of changes to the posterior layer of the iris. The pupil first takes on a pear-shaped shape and then becomes like an ellipse. At the same time, an eversion of the posterior pigment sheet occurs, which is sometimes mistaken for a neoplasm. In the area towards which the pupil becomes “pulled”, the ophthalmologist can detect the formation of synechiae - the fusion of tissues located close to each other. In some cases, this may also be local fibrosis - the proliferation of connective tissue, which is often quite difficult to distinguish from a tumor.
One of the last stages in the manifestation of symptoms is the exposure of the vessels of the iris. If its atrophy was not detected at earlier stages, then by this time the iris of the eye may already have many holes, albeit invisible to humans. In the most extreme cases, with late diagnosis, it can be so changed that it visually resembles a narrow border running along the pupil. At this stage, vision problems begin, the most common of which is diplopia, in other words, double image. The main danger of atrophy is that it often provokes the development of glaucoma, which can be either open-angle or closed-angle.
According to ophthalmologists, the second form is the most dangerous, as it entails a rapid decrease in vision and is much less amenable to drug treatment.
Why does iris atrophy occur?
It is quite difficult to talk about the reasons why iris atrophy occurs. The pathogenesis of this disease has not been fully studied by specialists. The main assumptions are a disruption in the development of the mesoderm surrounding the eyeball. The hereditary factor also plays an important role. If there was a diagnosis of “iris atrophy” in the family, then it is likely that the disease will make itself felt again, perhaps even after several generations. In addition, according to researchers of this pathology, people at risk include:
- suffering from neurotrophic disorders;
- predisposed to allergic reactions;
- prone to protein metabolism disorders.
In addition, some experts believe that sclerosis, as well as degeneration of the vessels of the iris, play an important role in the development of the disease. Other experts believe that damage to the vascular area is not the cause of the disease, but its consequence.
Causes of rubeosis of the iris
The etiology of the disease is not fully understood. Activation of the neovascularization process is provoked by a number of internal and external factors. The main causes of rubeosis include:
- Metabolic disorders
. Rubeosis often occurs secondary to diabetic retinopathy in patients with decompensated diabetes mellitus. - Retinal vein occlusion
. Thrombosis of the central vein of the inner lining of the eye leads to ischemia, which increases vascular proliferation. - Retinal detachment
. Normally, the inner membrane of the eyeball provides trophism to the iris. Retinal detachment or its degenerative-dystrophic changes underlie regional hypoxia, which provokes angiogenesis. - Pathology of the ophthalmic artery
. Damage to the vessels supplying the eyeball as a result of long-term atherosclerosis or arteritis leads to increased angiogenesis, the occurrence of rubeosis of the iris and neovascularization of the cornea.
Who is more susceptible to iris atrophy?
More often than others, women are susceptible to iris atrophy. Moreover, the pathology does not belong to the age-related category, such as cataracts or glaucoma. Quite often it is detected during examination of women whose age does not exceed 30-35 years. Experts have also noticed that damage to the visual organs can occur in several family members at the same time.
In addition, research by scientists has revealed cases of the development of iris atrophy based on the principle of anticipation. Simply put, if the disease is hereditary, then in representatives of each subsequent generation the disease will manifest itself at an earlier age. For example, if a grandmother was diagnosed at 45 years old, her daughter at 25, then a grandson or granddaughter may begin to develop atrophy in preschool age.
Why does glaucoma develop in parallel?
As we wrote earlier, eye atrophy often leads to the development of glaucoma, a dangerous ophthalmological disease that involves increased intraocular pressure and is one of the main causes of complete blindness. Why does this pathology occur against the background of iris atrophy? Ophthalmologists explain this pattern as follows: the formation of synechiae and the proliferation of fibrous tissue provoke difficulty in the outflow of intraocular fluid. The pressure inside the eye begins to increase when the fibrous tissue covers half of the iris.
In addition, in addition to the disruption of the outflow of intraocular fluid, a decrease in its subsequent release occurs. Experts explain this by degenerative processes occurring in the ciliary body - part of the choroid of the eyeball, which ensures the normal functioning of the lens and accommodation processes.
Causes of pathology
Factors causing rubeosis of the iris are considered to be diseases that lead to ischemia or insufficient blood supply to the tissues of the eye. Particularly common causes of neovascularization are: diabetes mellitus complicated by diabetic retinopathy, retinal vein thrombosis, as well as extensive, long-term retinal detachment. Often, systemic diseases also lead to the development of rubeosis, for example, disturbances in blood flow in the orbital artery, which feeds the eyeball, such as atherosclerosis.
These diseases lead to the fact that the main part of the retina, partly covering the posterior surface of the iris, remains in a state of prolonged ischemia. The state of ischemia causes the cells of the retina to release active substances, one of which is the so-called VEGF - vascular endothelial growth factor. A similar mechanism is universal for our body, for saving tissues from hypoxia. However, in this situation he poses a serious threat.
And the point is this: the walls of the newly formed vessels of the iris are very thin and fragile, in any case, they easily rupture, causing bleeding. Bleeding leads to the accumulation of blood in the anterior chamber of the eye - the so-called hyphema. In addition, newly formed vessels have the ability to grow into the area of the anterior chamber angle, where they should not be. As a result, another serious complication develops - secondary glaucoma, which is caused by blockage of the outflow pathway of intraocular fluid. This form of glaucoma has a very severe course, usually progresses quickly and often does not give the desired results in response to standard therapy.
Conservative treatment methods
One of the most important steps in treating iris atrophy is reducing intraocular pressure. In such cases, ophthalmologists prescribe antiglaucomatous drugs to patients to help accelerate the outflow of intraocular fluid. To achieve a greater effect, drugs that normalize metabolism and improve microcirculation in the tissues of the eyeball can also be prescribed. Selecting medications is not the easiest task, since before this the specialist will need to conduct a thorough examination of the patient, and also take into account many factors, including the presence of chronic diseases. The medications prescribed by your doctor must be used in strict accordance with the instructions and in no case should you stop taking them prematurely.
Most often, ophthalmologists prescribe the following medications to help accelerate the outflow of intraocular fluid:
- Pilocarpine;
- Latanoprost;
- Glaucon;
- Epiphrine;
- Travatan.
In addition, today there are combination drugs that simultaneously contain several components that have different effects. Thanks to their properties, it is possible to replace two or even three medications with one, which is not only convenient to use, but also very beneficial for the patient financially. These are drugs such as:
- Fotil;
- Azarga;
- Kosopt;
- Proxofeline;
- Normagluon.
Depending on the degree of development of the pathology, the ophthalmologist may prescribe other remedies, but all this is decided individually and only after a thorough examination and collection of anamnesis for a particular patient.
Treatment of neovascularization (rubeosis) of the iris
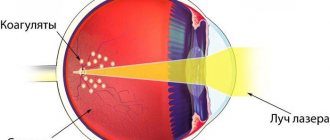
For successful treatment of iris rubeosis, it is necessary to carry out correct and adequate treatment of the underlying disease that provokes the development of neovascularization. If rubeosis of the iris or areas of retinal ischemia are detected in diabetic retinopathy, it is necessary to undergo a course of panretinal laser coagulation of the retina as soon as possible. To do this, small burns of up to 1200-1500 units are produced with a laser in the area of ischemic areas of the retina in order to remove these areas from metabolism and not stimulate the production of VEGF and the growth of new blood vessels.
If retinal vein thrombosis is detected, it is imperative to monitor the condition of the retina itself and, if necessary, perform laser coagulation in a timely manner.
The modern direction in the treatment of rubeosis is anti-VEGF therapy. With this technique, a drug is injected into the eye cavity using a syringe, which blocks the action of the growth factor of newly formed blood vessels. These drugs are produced using genetic engineering; They have a fairly pronounced effect, but their effect is short-lived, so repeated courses of therapy are necessary.
With the development of glaucoma against the background of rubeosis in the initial stages of the disease, intraocular pressure is reduced with the help of eye drops. However, quite often, this does not bring the desired result and surgical correction is recommended to the patient.
Types of surgical interventions
As a rule, with atrophy, surgical treatment is aimed primarily at normalizing the outflow of intraocular fluid.
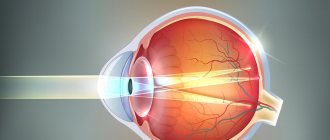
Such operations can be performed using either microsurgical intervention or laser vision correction. The latter option, due to its minimally invasive nature and short rehabilitation period, is the most preferable for most patients. If the patient has been diagnosed with “iris atrophy,” then the most effective way to solve the problem is to perform fistulizing operations, during which ophthalmic surgeons manage to create a new path for the outflow of fluid without damaging the muscles of the diseased eye. If the patient has a large lens, or in addition to atrophy of the iris, cataracts have developed, as often happens in elderly patients, then the doctor may recommend phacoemulsification - a procedure in which the iris of the eye is exposed to ultrasound.