In what cases do doctors use needles to irrigate the tear duct?
In medical practice, the problem of obstruction of the lacrimal canal is often encountered. The danger of the pathology lies not only in the discomfort it brings to the patient; for example, the eyes can continuously water, which interferes with the normal functioning of the visual apparatus. With obstruction, bacteria and viruses harmful to the body are activated, which find themselves in a favorable environment for development and reproduction. As a result, infectious diseases may develop.
You can eliminate congestion in the tear ducts by introducing a special liquid into their cavities. Filling occurs under slight pressure. Washing can be prescribed for diagnostic purposes and as targeted therapy for a number of ophthalmological diseases, such as:
- Corneal ulcerations requiring sanitation of primary foci of infection;
- Slight stenosis of the lacrimal canals and nasolacrimal duct;
- Congenital or acquired dacryocystitis in the first days of a baby’s life;
- Other inflammatory processes in the eye area.
Depending on the throughput, a specialist during the procedure can diagnose the condition of the lacrimal canal, identify incipient pathologies, unwanted protein and other deposits.
If there is no blockage, the liquid administered under slight pressure should come out freely through the nose. During the procedure, doctors use special sets of instruments, including needles for rinsing the tear duct.
Possible complications and additional information
In most cases, the lacrimal canal is washed in the prescribed manner, and the patient experiences absolutely no complications.
The most common mistake in carrying out the procedure itself is that the cannula begins to rest against the wall of the nasolacrimal duct.
This method perfectly helps to cope with the task at absolutely any age. However, if the anatomical structure of the nose and cavity is not diagnosed in advance, this can lead to a worsening of the situation, since when using lavage, the pressure will be too great, which can lead to rupture of the walls.
You may be interested in Diagnosis of vision in children under one and 3 years old
Lacrimal duct lavage in newborns
Due to the physiological characteristics of the structure, the nasolacrimal ducts of a baby can be blocked to a greater extent by a gelatinous film, which should self-destruct 15 days after the birth of the child. In standard cases, this process is not facilitated by medication - it occurs independently under the influence of tears.
However, the film does not always dissolve naturally, which may indicate its excessive density or a congenital anomaly in the structure of the skull or tear ducts. In such cases, doctors recommend postponing rinsing the baby's lacrimal canal. As a rule, the procedure should be delayed until the child is at least 2 months old. In some cases, ophthalmologists prescribe a special massage to the baby, which helps clean the tear ducts without additional intervention. In the first stages of therapy, the child's mother can massage the required area on her own. The set of exercises is not that complicated. For example, after each feeding, the mother massages the baby’s tear duct up and down with force 6-10 times. However, it is important to perform the massage correctly. It must be preceded by a mandatory consultation with a specialist.
If a set of exercises does not help, the lacrimal canal is washed in newborns. During medical intervention, before the procedure begins, the doctor administers local anesthesia to the child for pain relief.
A special rinsing kit is then used, which may include:
- Conical instrument (Zakhil probe);
- Bowman's probe, which has a pointed base (with its help, the doctor pierces the gelatinous film that interferes with the outflow of tear fluid);
- Special blunt needles, etc.
Before surgery, the lacrimal canals are disinfected with a solution. The final stage of washing involves disinfection by introducing antibiotics, which subsequently eliminates the risk of inflammation and the development of infectious diseases.
Washing the nasolacrimal duct
The importance of tears for the organs of vision is difficult to overestimate.
Scientists jokingly claim that it was crying that helped humanity survive under conditions of natural selection. It has long been known that tears improve visual acuity. The lacrimal mechanism ensures constant renewal of the film on the cornea. By lubricating the eyeball, tears protect it from drying out, inflammation and saturate it with nutrients and oxygen.
They have antibacterial properties and help get rid of foreign bodies in the eye.
In order to perform all the functions inherent in nature, the lacrimal mechanism works like a clock and requires special attention and support. A number of reasons can cause blockage of the tear ducts, intended for the outflow of tear fluid. As a result of the disruption of the outflow, involuntary tearfulness of the eyes appears, which creates favorable conditions for the development of various types of infections of the visual organs.
Every fifth baby is born with this pathology, but adult patients can also suffer from it. Obstruction or narrowing of the tear ducts can cause serious eye diseases. To eliminate them, ophthalmologists practice the manipulation of washing the nasolacrimal canals, which will be discussed in this article.
A little anatomy
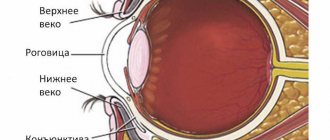
Nature has endowed humans with a unique lacrimal apparatus, which consists of the lacrimal gland and lacrimal ducts. The lacrimal gland is almond-shaped and located just behind the eye under the frontal bones of the skull.
A dozen tear ducts are laid from it to the eye and eyelid. When you blink, tears are released from the lacrimal gland, which washes the eye.
Sterile tears keep the eye clean, moisturize it, and the enzymes they contain destroy bacteria, preventing the spread of infection.
The lacrimal puncta in the inner corner of the eye (on the lower and upper eyelids) are connected to the lacrimal sac, from which tears enter the nose through the nasolacrimal duct. The uninterrupted outflow of ocular fluid is carried out due to negative pressure in the lacrimal sac.
In case of obstruction of the canals, the fluid formed in the eye stagnates in the lacrimal sac and can lead to its swelling and inflammation. In such cases, rinsing is required.
Symptoms of blocked tear ducts
The simplest example of the coordinated work of the nasolacrimal canal is the manifestation of a runny nose in the event of crying or an allergic reaction to the organs of vision.
In turn, malfunctions in its operation or infection of the tear ducts can be judged by the manifestation of the following symptoms:
- Watery eyes, excessive tearing.
- Persistent inflammation and infections.
- Pain in the corners of the eyes and their swelling.
- Discharge or accumulation of mucus.
- Blurry vision.
- Blood in tears.
Indications for manipulation
Blockage of the tear ducts can be congenital or caused by a number of factors, including age.
The most common indications for rinsing the nasolacrimal duct are listed below:
- Obstruction of the canals in infants, caused by an anomaly in the structure of the nasal bone or underdevelopment of the drainage system of the eye. It is characterized by the appearance of a mucous film, which can lead to inflammation with purulent discharge. In this case, the film is removed, followed by washing with disinfectants and anti-inflammatory substances.
- Blockage of the canals in newborns with a gelatinous plug that does not dissolve in the first two weeks after the birth of the child. In such cases, it is recommended to massage the lacrimal ducts after each feeding and only if there are no positive results.
- Narrowing of the entrance to the lacrimal canals in adults, caused by injuries, inflammatory diseases in the nasal cavity, tumors of the intraocular or surrounding tissue.
- Obstruction of the lacrimal canal in elderly people, caused by atherosclerosis, colds and swelling of adjacent tissues, injuries and other severe pathologies.
In addition to diagnosing pathologies of the lacrimal canals, manipulations to wash them are also carried out for medicinal purposes, for example, when identifying inflammation (canaliculitis). In this case, the procedure is preceded by cleansing the tubules of mucopurulent secretions.
During the manipulation of washing the nasolacrimal canals with diagnosed dacryocanaliculitis - inflammation of the lacrimal canals and dacryocystitis - inflammation of the lacrimal sac, medications are introduced into the cavity of the lacrimal canal or sac.
In addition, rinsing is used in the case of a diagnosis such as stenosis of the lacrimal canaliculi, as well as for mild degrees of stenosis of the nasolacrimal duct and corneal ulcer (to sanitize the primary source of infection).
Contraindications
Only an ophthalmologist can assess the function of drainage of the lacrimal canal and then select treatment methods.
However, the procedure for washing the nasolacrimal canal is not recommended in two cases:
- When the lacrimal sac is stretched and filled with mucus, such a procedure can give impetus to the spread of pus throughout the organs of vision.
- In case of purulent acute inflammation - hydrocele of the lacrimal sac - washing can cause its overstretching and lead to rupture of the structure of the sac.
Carrying out the procedure
In cases of nasolacrimal duct blockage, ophthalmologists recommend trying a less invasive treatment option first. The washing procedure can be carried out for both diagnostic and therapeutic purposes.
In the first case, this procedure allows ophthalmologists to verify the patency of the lacrimal ducts, for which liquid is injected into them under moderate pressure.
If there is a need for treatment, antibiotics, antiseptics or substances that improve patency are injected into the lacrimal canaliculi, depending on the indications.
Elimination of obstruction of the tear ducts is carried out under local anesthesia. In cases where there is no need to probe the lacrimal ducts, punctures are not performed.
An anesthetic is instilled into the conjunctival cavity, after which a special cannula with a syringe is inserted into one of the tear discharge points.
If the liquid gradually introduced into the cavity freely leaves the nasal sinuses, the lacrimal canals are not blocked, and the flow of liquid back from the eyes indicates the presence of pathology. In such cases, the nasolacrimal ducts are washed with a solution of furatsilin or an isotonic solution of sodium chloride.
The procedure is absolutely safe, does not injure tissue and is recommended for patients regardless of age, including newborns after they reach two months. Ophthalmologists do not recommend postponing the diagnosis of lacrimal duct pathology in adults, because such manipulation becomes more complicated with age.
The procedure and features of the procedure for newborns and adults are given below.
Irrigation of tear ducts in infants
At the birth of a baby, the nasolacrimal ducts in children are blocked by a gelatin film, which, under the influence of tears, should dissolve in the first two weeks of the child’s life. However, in 6% of newborns this does not happen due to the increased strength of the film or the abnormal structure of the canals and bones of the skull, which complicates the outflow of tears.
In such cases, no earlier than after the child reaches two months, ophthalmologists practice a series of manipulations related to the removal of the film with further probing and washing of the nasolacrimal canal.
Having previously numbed the procedure site, a special conical instrument called a Sichel probe is inserted. This manipulation is necessary for the initial expansion of the canal, into which the Bowman probe is then inserted.
With this tool, which has pointed ends, the gelatin film is pierced.
At the next stage, the lacrimal canals are washed with a disinfectant solution. In order to avoid infection of the lacrimal drainage system, the procedure ends with disinfection of the lacrimal ducts with antibiotic eye drops.
The washing process is absolutely painless and lasts no more than a quarter of an hour.
Over the next few days, the child should instill eye drops carefully selected by the doctor, taking into account the patient’s age, according to the scheme and dosage prescribed by the ophthalmologist.
To prevent relapse of the disease and prevent the formation of adhesions, ophthalmologists recommend massaging the child’s lacrimal tubules for two weeks after removing the film. To do this, use your index finger to lightly press on the inner corner of your eye for one to two minutes.
Often, on the eighth or ninth day of life, a child develops dacryocystitis - purulent inflammation of the eyes, accompanied by redness of the inner corner of the eyes, lacrimation and discharge of pus from the lacrimal opening when pressing on the lacrimal sac. This disease develops due to stagnation of tears caused by the remains of embryonic tissue in the nasolacrimal duct, which prevents the outflow of tears from the lacrimal sac.
For dacryocystitis in newborns, ophthalmologists practice a special massage, which is aimed at improving the patency of the lacrimal ducts, and only if it is ineffective, they prescribe treatment in the form of probing and washing the clogged lacrimal ducts.
At the first stage of treatment, the mother of the newborn is recommended to massage the baby's lacrimal sac (6-10 movements up and down with force) after each feeding. When the massage is performed correctly, the amount of pus coming out increases.
After the massage, it is necessary to rinse the eyeball with a solution of furatsilin (1 tablet dissolves in a glass of boiling water). Purulent particles should be removed by wiping the palpebral fissure with cotton swabs soaked in the solution, moving from the temple to the nose. The procedure ends with instillation of an antibiotic solution - 1 drop of 0.25% chloramphenicol at least 5 times a day.
The effectiveness of the procedure directly depends on the age of the child; the younger he is, the more effective this massage is. It is recommended to carry out such treatment for two weeks and only if it is ineffective, proceed to the second stage, namely the previously described probing and rinsing.
The course of therapeutic lavages for dacryocystitis in newborns in some cases can last for a week or two, and the procedures are carried out every one or two days.
Rinsing tear ducts in adults
Pathology of the lacrimal ducts in adults occurs at any age and is determined diagnostically.
Unlike infants, massage alone, as well as probing, cannot solve the problem of canal patency in adults.
Having established the passive patency of the tear ducts, the ophthalmologist, if pathology is detected, prescribes forced rinsing with disinfectants.
To achieve better results, ophthalmologists practice a combination of lavage and probing of the lacrimal ducts. This procedure is considered the most effective for obstruction of the tear ducts, since it simultaneously increases the lumen of the canal and helps relieve inflammation.
Moreover, it is less traumatic compared to hard probing.
The rinsing solution is injected into the area of the lacrimal punctum near the nose using a syringe with a blunt needle or cannula through a conical probe that widens the entrance to the canal. The cannula is inserted as deeply as possible without touching the walls. Pulling back the patient's eyelid, the doctor slowly presses the syringe plunger, observing during the procedure the dynamics and ease of passage of the solution.
For pain relief, drops are instilled into the eye before the procedure. If it is not possible to solve the problem with rinsing and pus continues to be released from the canals, ophthalmologists involve drug treatment with antibiotics and anti-inflammatory drugs, or surgery.
Analysis of results
Ophthalmologists interpret the results when washing the nasolacrimal canals according to the following scheme.
In the absence of pathology of the canals, the liquid easily flows through the nose. When introducing the solution, no particular effort is required; the liquid is injected with light pressure on the piston. Stenosis of the nasolacrimal duct or fusion of the canal orifices is indicated by the leakage of fluid from the opposite lacrimal punctum.
With stenosis of the nasolacrimal duct, fluid may begin to flow from the opposite lacrimal opening not immediately, but after a matter of seconds or after increasing pressure on the piston. At the same time, there are traces of blood in it. With stenosis of the internal part of the canal, fluid flows out from the same place where it was injected.
When the nasolacrimal duct becomes clogged, fluid flows out of the nose when the pressure on the syringe plunger increases.
Complications during the procedure
In the case when all contraindications are taken into account and the procedure technique is followed, no special complications are noted.
The only negative consequence may be a distortion of the results of the diagnostic test if the cannula with liquid is inserted incorrectly, in particular, the cannula touches the canal walls.
Source: https://FoodandHealth.ru/meduslugi/promyvanie-slezno-nosovogo-kanala/
Lacrimal duct rinsing in adults
Doctors can diagnose blocked tear ducts in patients of any age. Most often in adults, the procedure is performed for diagnostic purposes. Using this method, it is possible to determine the percentage of passive patency of the lacrimal ducts (in some cases, the diagnosis is carried out several times).
Problems with patency in adults are more difficult to eliminate than in infants. In this case, neither probing nor massage helps. Due to the tightly formed tissues, the only way to restore tear flow is repeated rinsing.
If a thick film blocks the tear ducts, as a rule, simple rinsing is not prescribed. In the appropriate situation, surgical intervention is advisable.
As with newborns, the patient is given antibiotics after the procedure to prevent complications. The drugs are taken during the rehabilitation period. They can be in the form of nasal sprays or drops.
How to rinse the tear duct
Before the specialist begins the rinsing procedure, he conducts a diagnostic examination to rule out anatomical pathology of the nasal structure. If the pathology is not congenital, then most likely it is associated with the development of a tumor.
Indications for rinsing
— Development of dacryocystitis in newborns, if special massage does not help to activate the tear fluid movement system.
— Development of an inflammatory process or stenosis spreading in the lacrimal canals.
— Lack of sufficient patency in one of the nasolacrimal ducts.
Possible contraindications
Rinsing the lacrimal canal is impossible in case of development of an inflammatory process or dropsy. In addition, if pus forms, the procedure is also postponed until the symptom is completely eliminated due to the likelihood of sepsis. Purulent discharge can also accelerate the spread of infection, which will only increase the scale of the problem.
Symptoms
There are a number of signs of problems in the functioning of the lacrimal ducts. These may be symptoms such as:
- Excessive tear production;
- Swelling, pain in the corners of the eyes;
- Infections, inflammations, and also disturbing a person for a long time;
- Mucus accumulation and excessive secretion.
In addition to the listed symptoms, patients with obstruction often complain of blurred vision. If the above symptoms appear, the right decision would be to seek qualified help. Timely treatment, preceded by early diagnosis, will help get rid of undesirable consequences.
Contraindications
As with any other procedure, there are some contraindications for washing the lacrimal ducts. Thus, the operation is not performed on people who have hydrops of the lacrimal sac or purulent inflammation of the eyes (hydropsus and phlegmon, respectively). Rinsing is not prescribed if the patient is diagnosed with a stretched lacrimal sac (it contains mucus) due to the risk of spread of pus. In a number of other cases, the procedure is not considered dangerous and does not require additional care, but during the healing period you will have to stop wearing soft contact lenses and other types of them (the use of glasses with diopters is recommended to correct refraction).
Rinsing the tear ducts is a safe method of diagnosis and treatment that does not injure the tissue. Ophthalmologists do not recommend delaying the examination, since the corresponding disorders are easier to eliminate in the early stages of development.
The website of the online store Ochkov.Net presents a wide range of contact correction products. From us you can order products from well-known brands such as Acuvue, Biomedics, Hera and others.
What complications may arise?
If the procedure is carried out by an experienced, qualified specialist, then there are no problems. Most complications are due to the doctor's inexperience or negligence. The most common complication is infection and inflammation of the tear duct as a result of injury.
Why is it best to undergo this procedure with us?
Judging by patient reviews, our clinic is considered one of the best in Chelyabinsk and the Chelyabinsk region among ophthalmological medical institutions. We employ only experienced, knowledgeable specialists, and use the latest equipment for treatment and diagnosis. By contacting us, you can be absolutely sure of the safety and high quality of all procedures performed.