Causes
The disease is based on infection of the lacrimal sac by various pathogenic microorganisms - pneumococci, streptococci and other pyogenic microbes. Sometimes the disease can be triggered by inflammatory processes in the maxillary or nasal cavity, as well as in the ethmoid labyrinth. But most often, phlegmon of the lacrimal sac develops against the background of an exacerbation of chronic purulent dacryocystitis and is actually a complication of this disease.
Due to the fact that the disease develops quickly, measures to stop it must be taken in a short time to avoid the development of purulent and necrotic processes.
In some cases, phlegmon heals on its own, but tear secretion functions may be impaired.
Inflammation of the tear duct or dacryocystitis
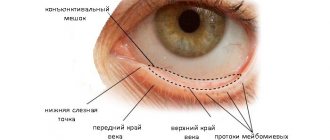
Swelling under the eye, redness, itching and discharge of pus - this is how inflammation of the lacrimal canal or dacryocystitis manifests itself. The disease occurs due to narrowing of the tear duct and infection in the lacrimal sac.
Inflammation of the tear duct is manifested by swelling and discharge of pus
Causes of pathology
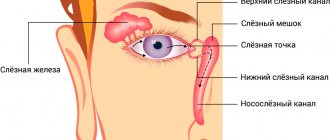
Most often, the disease develops against the background of congenital narrowing of the nasolacrimal duct, when the secretion of the lacrimal gland cannot be separated from the ducts at the required speed and stagnates in them. Pathogenic microflora is formed in stagnant tear fluid. Inflammation under the eye occurs not only due to the congenital structural features of the ducts, but also due to their blockage.
Diseases that lead to blockage of tear ducts include:
- deviated nasal septum;
- diabetes;
- eye diseases that provoke inflammation (styre, conjunctivitis, blepharitis, iritis);
- oncology of the eyes and nose;
- diseases that activate the vital activity of streptococcus aureus and staphylococcus (tonsillitis, otitis media, sinusitis);
- atherosclerosis;
- lacrimal caruncle cyst;
- formation of stones in the tear ducts.
Important! Inflammation of the tear ducts is often observed in newborns.
During the period of intrauterine growth, the tear duct is covered with a film; after birth, it is destroyed, which allows tears to be quietly separated. But sometimes this does not happen, and tear secretion, accumulating in the ducts, provokes an inflammatory process.
Inflammation under the eye can also be caused by:
- clogging of the tear duct with foreign objects and dust;
- hypothermia;
- eye damage;
- incomplete removal of cosmetics and poor hygiene.
Systematic hypothermia of the body leads to canal stenosis - narrowing of the lumen due to spasm.
Elderly people are also susceptible to inflammation of the lacrimal duct: with age, the lacrimal duct narrows, which provokes impaired tear production and the appearance of infection in the lacrimal sac.
Symptoms of inflammation of the tear duct
Signs of dacryocystitis appear gradually. You can see what inflammation of the tear duct looks like in the photo.
The first thing people notice is sudden profuse lacrimation at low air temperatures. The symptom indicates the initial stage of the disease.
Other signs of dacryocystitis:
- wet eye syndrome;
- swelling of the lower eyelid;
- blurred vision;
- itching, redness, soreness of the eyelids;
- enlarged lymph nodes behind the ears;
- uncontrollable lacrimation;
- purulent discharge from the lacrimal duct.
One of the signs of dacryocystitis is uncontrolled lacrimation
In severe cases, swelling of the lower eyelid narrows the palpebral fissure. Usually the disease is diagnosed only on one side.
Important! The first signs of the disease in a baby are redness of the inner corner of the eye, souring, uncharacteristic restlessness and refusal to breastfeed. If you notice these signs, consult a doctor immediately.
Which doctor should I contact?
Adults with symptoms of dacryocystitis consult an ophthalmologist. Children require an initial appointment with a pediatrician, who, if necessary, will give a referral to an ophthalmologist. If the inflammation has taken an advanced form, the ophthalmologist will refer you to a maxillofacial surgeon or dentist for surgery.
Treatment for inflammation of the tear duct
What to do if the tear duct is blocked? The disease is treated with medications, massage and folk remedies. In severe cases, surgery is performed.
Medicines
For the treatment of dacryocystitis, drugs are prescribed for both oral and topical use.
Levomycetin - eye drops
| Group of drugs | Action | Examples |
| Antibiotics | Destroy pathogenic microflora in the body, fight bacteria | Ampicillin, Oxacillin |
| Eye drops | Suppress the proliferation of pathogenic microorganisms | Sulfacyl sodium, Levomycetin, Gentamicin |
| Antiseptics | Disinfect, prevent suppuration and decomposition of tissues at the site of inflammation | Furacilin, Dioxidine, Chlorhexidine |
| Ointments | Have a local antibacterial effect, prevent the growth of bacteria | Tetracycline, Erythromycin, Floxal |
| Immunomodulators | Stimulate the immune system to actively protect the body | Tsitovir-3, Arbidol, Dibazol |
Important! If improvement does not occur within 3 days, the prescribed medications are not effective - inform your doctor.
Massage serves as a preventive procedure against eye diseases
Treatment of inflammation of the nasolacrimal duct only with pharmaceutical drugs has been found to be ineffective: along with taking medications, it is necessary to regularly massage in order to clear the lacrimal sac from accumulated pus as quickly as possible.
How to treat with folk remedies?
Treatment of obstruction of the nasolacrimal duct with folk recipes at home is permissible in combination with pharmaceutical drugs, provided there is no hypersensitivity to the components.
The most effective folk remedies:
- Aloe. Dilute fresh aloe juice with cold boiled water in a 1:1 ratio and drop it into your eyes 4-5 times a day.
- Kalanchoe. Squeeze out fresh Kalanchoe juice and place 2 drops in each nostril while lying down. To administer to a child, dilute the juice in equal proportions with boiled water. Kalanchoe causes sneezing, during which the tear duct is naturally cleared of pus. Do the procedure once a day.
- Chamomile. Brew 3 tbsp. l. dried chamomile flowers in 1 liter of boiling water, let it brew for 1 hour. Soak a cotton pad in the infusion and apply to the sore eye. The lotion should be warm, not hot. Keep the compress until it cools completely. It is recommended to apply chamomile lotions 2 times a day until recovery.
- Thyme. Brew 1 tsp. dry thyme in 200 ml of boiling water, strain after 30 minutes. Rinse your eyes with warm infusion of thyme 2 times a day.
- Tea. Make a very strong brew of black tea and use it to wash your eyes and remove pus from them at least 4 times a day.
- Propolis. Take 30 drops of propolis aqueous extract orally 3 times a day. Propolis is a natural antibiotic, strengthens the immune system and relieves inflammation from the inside.
Propolis extract serves as a natural antibiotic against inflammation
Make compresses and rinses not only for an eye clogged with pus, but also for a healthy one - this way you can protect the healthy eye from inflammation.
Massage for tear duct obstruction
Massage is done to remove pus from the lacrimal sac. The procedure is an integral part of the treatment of dacryocystitis in children. Massage is effective in the initial stages of the disease.
Do not massage with long fingernails - they can injure the eyes and mucous membranes.
Technique:
- Wash your hands thoroughly and treat them with antiseptic.
- Using a clean cotton swab soaked in furatsilin, clean the eye from accumulated pus.
- Feel the lacrimal sac: it is located below the inner corner of the eye. Place your finger on the lacrimal sac and massage it with slight pressure for 10 seconds, first clockwise, then counterclockwise.
- Finger on the lacrimal sac. Make 5-7 jerky upward movements with slight pressure, squeezing the pus inside upward.
- Repeat the same movements in the downward direction.
- Place your finger on the bridge of your nose at the inner corner of your eye. Using massaging movements with pressure, move your finger from the bridge of the nose to the corner of the eye, repeat 5-7 times.
- During the massage, pus will be separated from the lacrimal canal - upon completion of the massage, remove it from the eye using a cotton swab soaked in furatsilin.
Perform the massage in strict order. Frequency of execution – 5 times a day. Children are recommended to massage the lacrimal sac before feedings.
Important! You cannot massage if dacryocystitis is advanced - this can lead to the development of inflammation of the orbit or eyeball.
Possible consequences and complications
With delayed or improper treatment, inflammation intensifies, which is fraught with serious complications.
Brain abscess is one of the complications of inflammation of the tear duct
Taxes of dacryocystitis:
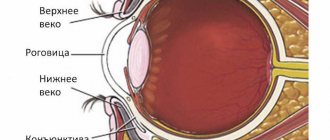
- thinning of the cornea;
- encephalitis;
- inflammation of the orbit;
- inflammation of the eyeball;
- meningitis;
- abscess of the brain or lacrimal sac.
Inflammation of the eye mucosa is accompanied by microtraumas of the cornea. With a long course of the disease, ulcers and erosions appear on the cornea of the eye, through which infection penetrates into the cavity of the eyeball.
Inflammation of the nasolacrimal duct develops quickly and, if left untreated, can spread to neighboring tissues and organs. To prevent the need for surgery, consult a doctor in a timely manner. Do not let the course of the disease take its course - dacryocystitis can lead to loss of vision.
Loading…
Symptoms of phlegmon of the lacrimal sac
Phlegmon of the lacrimal sac is externally manifested in redness of the skin around the eye, eyelid, cheek, nose and significant swelling, so strong that it can completely close the palpebral fissure. A painful, hot lump is felt above the lacrimal sac. In this case, the patient’s temperature rises, weakness and headache occur. Sometimes a feverish state occurs.
After two or three days, pus accumulates in the lump and it becomes soft to the touch. The surrounding skin turns yellow. The process progresses and opens through the surface of the skin; after the complete outpouring of pus, the inflammation subsides. In some cases, a fistula appears at the site of the lesion, secreting pus and tear fluid. It is possible to open the abscess into the nasal cavity through the nasolacrimal canal. In this case, a new artificial opening appears that drains fluid from the eye into the nasal cavity.
Diagnostics
To understand whether the tear duct is clogged in an adult or child, it is necessary to collect a medical history and complaints. Next, the doctor conducts an external examination, determines the severity, stage, and form of the disease.
To diagnose dacryocystitis, the following types of studies are used:
- Stenosis can be detected using the West nasolacrimal test. Special colored drops (“Collargol” or “Protargol”) are instilled into the conjunctival sac, and a cotton swab is inserted into the nose. After the time has passed, look at the amount of dye on the tampon.
- Dacryocystography - shows the level at which blockage (complete or partial) of the lacrimal canal occurs. To do this, a contrast agent is injected into the duct and radiography is periodically taken.
- Rhinoscopy is a complete examination of the upper respiratory tract, sinuses and passages using an endoscope.
- Test probing and rinsing with a sterile solution.
- Biomicroscopy of the eye.
- MRI of the orbits, as well as the facial skull.
- If necessary, a smear from the mucous membranes for bacterial microflora, laboratory tests, and consultations with related specialists are added.
Consequences of phlegmon of the lacrimal sac and prevention of the disease
The most common complication of the disease is the penetration of pus into the paranasal sinuses. A more dangerous consequence is the spread of a purulent-inflammatory process, which leads to the formation of orbital phlegmon, which affects the membranes of the eye and the optic nerve, which can result in blindness or death of the patient.
Considering the danger of phlegmon of the lacrimal sac for the life and health of the patient, it is important to strive to prevent the development of this disease. To do this, all inflammatory diseases of the nasal sinuses and purulent skin lesions in the facial area should be promptly identified and treated.
It is equally important to carefully observe the rules of personal hygiene, which helps prevent pathogenic microorganisms from entering the eye tissue. For example, if you wear contact lenses, then perform all manipulations with them only with thoroughly washed hands, and regularly disinfect them using special solutions.
Prevention
Unfortunately, due to the fact that there is no specific etiological picture, specific preventive measures have also not been developed. Therefore, it is advisable to adhere to general recommendations:
- eat right, namely include in your diet foods that provide all the necessary vitamins and minerals;
- stop smoking and excessive alcohol consumption;
- promptly and correctly treat all diseases in order to prevent their chronicity;
- if there is a family history of cancer, you should regularly visit an oncologist for a preventive examination;
- If you feel unwell, do not self-medicate.
These recommendations do not guarantee the elimination of the occurrence of this type of pathology, however, they make it possible to reduce the risk of its development or diagnose the disease in a timely manner.
Treatment
When treating phlegmon of the lacrimal sac, anti-inflammatory drugs and intramuscular antibiotics are used. The dosage of drugs and the timing of treatment depend on the patient’s condition.
Local treatment is also indicated. To do this, antibacterial solutions and corticosteroids are instilled into the eyes four times a day. Blue light and UHF are effective measures to influence phlegmon during the infiltration stage.
When an abscess has formed, surgical intervention is performed, during which the doctor removes pus and necrotic tissue, followed by washing the wound with antiseptic solutions.
Subsequently, reconstructive surgery is performed, the main goal of which is to create a new tear path. It is called dacryocystorhinostomy. This procedure is performed to avoid relapse.
How to treat dacryocystitis
Treatment of pathology in a child involves watchful waiting. It takes time for the nasolacrimal ducts to mature, strengthen and develop. In this case, massage of the lacrimal ducts and lacrimal sac is used during each feeding of the child. This will help break the uterine membrane that blocks the outflow tract at birth, as well as the adhesions that have formed, without surgical intervention.
If the baby's eye becomes very sour or inflammation occurs, it is necessary to use antibacterial eye drops. The ophthalmologist will tell you which drug is right for you and in what dosage after examining the child and taking the necessary tests.
Treatment of dacryocystitis in adults combines conservative means, traditional medicine, home methods and surgery. Therapy depends on the patient’s age, form, stage, severity of dacryocystitis, as well as its underlying cause.
If there is a large accumulation of pus in the lacrimal sac, as soon as the plug begins to come out, all the contents are evacuated into the nose, and the swelling also disappears. If the process is not complicated, then the disappearance of the symptoms of dacryocystitis, tearing when dropping drops into the eye, and the appearance of a bitter taste in the mouth will be a sure sign of recovery.
Dacryocystitis can go away on its own with the use of massage exercises. This is especially true in childhood; with the help of massage, the tear outflow pathways that have not yet fully opened are broken through.
Conservative treatment
Conservative treatment is used for the chronic form of the disease, narrowing or stenosis of the lacrimal system. If there is an obstruction or blockage, acute dacryocystitis will not be cured by drops or ointments. In this case, specialist intervention is necessary, including surgery.
Treatment begins with washing the lacrimal canals with a bactericidal agent, this can be Chlorhexidine, Furacilin, peroxide, Dioxidin, or simply saline sodium chloride solution. Next, to prevent the spread and multiplication of the infection, antibacterial agents are prescribed.
Ointments and drops for dacryocystitis:
- "Ciprofloxacin";
- "Miramistin";
- "Dexamethasone";
- "Tobrex";
- "Floxal";
- tetracycline ointment;
- gentamicin ointment;
- Vishnevsky ointment.
Along with medications, it is recommended to perform a special massage for dacryocystitis.
In case of an acute attack, treatment occurs exclusively in a hospital. Intramuscular antibiotics (tetracycline, benzylpenicillin, sulfadimezin), physiotherapeutic procedures, UHF, massage, eye drops and ointments are prescribed.
Watch a video about shock wave therapy:
If the process is not resolved, surgical intervention is resorted to.
Surgery
If there is no effect from conservative therapy for dacryocystitis in adults, surgical treatment is prescribed. For adults, surgical procedures are performed under local anesthesia, while for children only under general anesthesia.
Surgical intervention is divided into several options:
- Bougienage - this technique helps to expand narrowed or stenotic tear outflow channels.
- Dacryocystorhinostomy - using this method, the surgeon creates an artificial connection between the conjunctival cavity and the nasal sinus.
- Probing - using this procedure, a small thin probe is used to break the films and adhesions that interfere with the normal outflow of tears.
Folk remedies
Treatment of dacryocystitis at home is possible only after examination by an ophthalmologist and his permission. Folk recipes use eye drops, compresses, and lotions to wash the tear duct in adults. Alternative medicine is strictly contraindicated for children.
What to do if the eye canal becomes inflamed:
- Use aloe juice diluted 50 to 50 with boiled water for eye drops or lotions.
- An aqueous solution of honey is a natural antiseptic; it is used in the eyes for inflammation.
- Eyebright juice, thyme tincture, and calendula are used for compresses.
- Wash your face with a decoction of chamomile, sage, and birch leaves and wash out the tear ducts.
- Black tea bags are applied as warm compresses.