Kidney pyelonephritis is a nonspecific infectious inflammatory disease of the kidneys, which affects the renal parenchyma (mainly interstitial tissue), calyces and pelvis.
- Epidemiology
- Classification (types) of kidney pyelonephritis
- Etiology (causes and pathogens)
- Pathogenesis of kidney pyelonephritis
- Pathomorphology
- Symptoms of kidney pyelonephritis
- Diagnosis of kidney pyelonephritis
- Treatment of pyelonephritis
Epidemiology
In the CIS countries, according to statistics, there are 15-16 cases of acute pyelonephritis per 100,000 population. There are also 18 cases of chronic pyelonephritis per 1000 population.
The peak incidence of pyelonephritis occurs in three age periods. The first one is up to 3 years old. For every 8 sick girls there is 1 sick boy. The second peak of incidence occurs during active reproductive age - from 18 to 35 years. For every 7 sick women there is 1 sick male. Elderly and senile age is the third peak of incidence. Starting from the age of 60, the number of sick women and men becomes equal. Among patients over 70 years of age, the majority are men, since they develop tumor and hypertrophic processes in the prostate gland, which disrupts the dynamics of urine.
In the first two age periods, girls and women are more likely to get sick, which is explained by the peculiarities of the hormonal status, which changes during pregnancy and leads to dilatation, hypotension and dyskinesia of the urinary tract. Also another reason is the anatomical and physiological characteristics of the urethra (it is short, the rectum and genital tract are located nearby). The increase in female morbidity is also influenced by the use of oral contraceptives.
Pathogenesis of kidney pyelonephritis
Routes of entry of the pathogen into the body:
- hematogenous
- urogenic
- lymphogenous
Factors that influence the development of pyelonephritis:
- Neurogenic bladder dysfunction
- Urinary tract obstruction
- Pregnancy (the tone and peristalsis of the ureters decreases, functional insufficiency of the vesicoureteral valves develops, the dynamics of blood in the kidney changes, the enlarged uterus compresses the ureters)
- Sexual activity
- Vesicoureteropelvic reflux
In chronic pyelonephritis, arterial hypertension may be observed, which is associated with infiltration of interstitial tissue. As a result, the dynamics of blood inside the kidneys is disrupted and the production of renin increases. When the inflammatory process subsides, hypertension disappears. Prerequisites for the preservation of hypertension are created in the case of sclerotic processes in the kidneys, including in the area of the vascular pedicle.
Causes
The main reason that leads to the development of chronic pyelonephritis is infection of the kidney tissue, which can occur in various ways. We are talking about the following:
- ascending, in which microorganisms penetrate from the lower parts of the genitourinary organs;
- hematogenous - microbes are transferred through the bloodstream from foci of chronic infection (diseases of the ENT organs, dental diseases);
- lymphogenous – infection penetrates the renal parenchyma through the lymphatic tract. The main causative microorganisms leading to the development of this disease are the following: Escherichia coli, Proteus, Klebsiella, Enterobacter, Enterococcus, Staphylococcus, Streptococcus, Pseudomonas aeruginosa, some types of anaerobes and others.
Pathomorphology
The following morphological forms of acute pyelonephritis are distinguished:
- purulent
- serous
- purulent with mesenchymal reaction
In chronic pyelonephritis, the inflammatory process is focal and polymorphic. Histological changes can be different; a common morphological sign is lymphohistiocytic infiltration. The same changes can occur with endemic Balkan nephropathy, chronic tubulointerstitial nephritis while taking analgesic drugs, and primary changes in the vessels of the kidneys. Chronic pyelonephritis differs from other kidney diseases by the simultaneous involvement of the pyelocaliceal system of the organ. Changes in the kidneys as the process progresses are characterized as focal, uneven and asymmetrical.
Instrumental diagnosis of chronic pyelonephritis
Ultrasound and excretory urography are mainly used to diagnose chronic pyelonephritis.
Characteristic signs of the disease on sonography are the following changes:
- reduction in kidney size, asymmetry compared to the intact side;
- atrophy and thinning of the medulla;
- compensatory hypertrophy of a healthy kidney or intact areas on the affected side;
- thinning and expansion of the pyelocaliceal system.
Excretory urography reveals similar changes in addition to signs of impaired urinary outflow. With severe vesicoureteral reflux, they lead to significant dilation of the ureters, which is an unfavorable sign. The effectiveness of conservative treatment in such patients is significantly reduced.
Radioisotope scanning is a sensitive method for detecting damage to the kidney parenchyma and foci of sclerosis. Defects in radiopharmaceutical accumulation correspond to areas replaced by connective tissue. The method allows you to estimate the amount of damage.
Symptoms of kidney pyelonephritis
Acute pyelonephritis
Symptoms in the acute form of the disease are divided into local and general. There is constant or remitting fever and chills. Typical symptoms are:
- myalgia
- arthralgia
- weakness
- nausea and/or vomiting
In 10 cases out of 100, there is a picture of bacteremic shock with acute renal failure, arterial hypotension, and severe tachycardia. Among the local manifestations, most often there are lumbar pains, more or less intense. The pain mainly occurs when tapping in the lumbar region and pressing on the costovertebral angle. In frequent cases, dysuria occurs.
In elderly patients, the acute form of the disease with cachexia does not proceed violently, only anemia and intoxication syndrome appear. A mild course of the disease is observed in pregnant women. Rarely there are purulent forms of acute kidney pyelonephritis. Their course is severe. Very often they are complicated by bacteremic shock, in 1/4 of cases - acute renal failure. The expansion of the renal cavity system can be very large, up to a maximum of ureterohydronephrosis.
Necrotizing papillitis can develop when an acute urinary tract infection is combined with urinary tract obstruction or renal vascular disease. It often happens when:
- gout
- diabetes mellitus
- sickle cell anemia
- alcoholism
Symptoms of necrotizing papillitis are:
- pain in the side or stomach
- hematuria
- acute renal failure
- fever
- necrotic masses in urine
- ring-shaped shadow in the renal calyx (on a pyelogram)
Chronic pyelonephritis
This form (if we do not talk about the period of exacerbation) occurs without symptoms or with a mild clinical manifestation. The manifestations are the same as in acute pyelonephritis, but less obvious. Patients complain mainly of pain in the lumbar region. The pain may appear as a feeling of heaviness, and if it recurs, it can be severe. Pain with pyelonephritis can be strangely localized: in the coccyx area. Attacks of renal colic indicate occlusion of the ureter by a blood clot, stone, pus clot, tissue detritus in necrotizing papillitis.
As for dysuric phenomena, stranguria and pollakiuria are noted. The first symptom means pain when urinating, and the second means frequent urination. In the stage of renal dysfunction, the organ’s concentration ability decreases. With simultaneous damage to the lower parts of the urinary tract, dysuric phenomena have different shades:
- with acute anterior urethritis in men, pain and burning during urination, discharge from the urethra are observed
- For cystitis, which is often recorded in females, imperative urges, frequent urination, and pain in the area above the pubis are typical.
- in acute prostatitis and total urethritis, difficulty urinating, frequent painful urination, pain in the perineum are recorded
- chronic prostatitis is characterized by nocturia, frequent urination, sexual dysfunction, urgency
- The chronic form of pyelonephritis is characterized by fatigue, weakness, poor appetite, headache, various manifestations of intoxication syndrome, but these cannot be considered specific signs
At the beginning of the development of chronic pyelonephritis, hypertension occurs in 15-25% of cases, and in the later stages it occurs in approximately 70 cases out of 100.
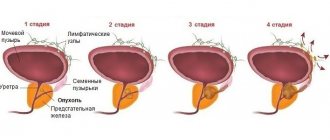
Classification of chronic pyelonephritis
The clinical classification of chronic pyelonephritis, adopted in the CIS countries, distinguishes the following forms of the disease:
- latent;
- recurrent;
- hypertensive;
- anemic;
- azotemic.
This division is conditional, since one patient may experience several leading syndromes. According to the course, chronic pyelonephritis is distinguished in the phase of exacerbation or remission. By localization - one-sided or two-sided.
The presence of complications - anemia, hypertension, chronic renal failure - suggests a complicated form of the disease. If there are disturbances in the outflow of urine from the diseased kidney during an exacerbation, abscesses may form. Renal shrinkage or total nephrosclerosis is the result of a long-term disease.
Diagnosis of kidney pyelonephritis
In typical cases, diagnosis is not difficult. Acute pyelonephritis allows one to suspect a number of signs:
- pain and muscle tension in the lumbar region
- fever
- laboratory findings indicating kidney damage
- intoxication syndrome
The diagnosis is clarified using the following methods:
- ultrasound examination of the kidneys
- chromocystoscopy
- MRI
- CT scan
- isotope dynamic scanning
The following factors are important in the medical history:
- Metabolic disorders (nephrolithiasis, diabetes mellitus, etc.)
- Recurrence of urinary tract infections
Other factors in the development of kidney pyelonephritis are:
- polycystic kidney disease
- neurogenic bladder
- long-term treatment with GC and cytostatics
- pregnancy
Laboratory research
A general blood test shows leukocytosis with a shift to the left. A general urine test reveals an alkaline reaction in urine. Urinalysis according to Nechiporenko reveals a large number of leukocytes, predominant over red blood cells. The Zimnitsky test shows a predominance of nocturnal diuresis and a decrease in the relative density of urine. Bacteriological examination of urine helps to identify infection. In such cases, 105 or more microorganisms are found in 1 ml of urine, which is collected in compliance with the rules of asepsis in the middle of urination. A cultural study is necessary to determine the type of microflora and find suitable antibiotics for treatment.
For latent pyelonephritis, a prednisolone test should be performed. The technology is as follows: 30 mg of prednisolone in 10 ml of 0.9% sodium chloride solution is injected intravenously over five minutes, then after 1, 2, 3 hours and a day later, urine is collected for examination. The test is considered positive if, during the administration of prednisolone, urine collected over 1 hour contains more than 400 thousand leukocytes.
Instrumental studies for kidney pyelonephritis:
- Ultrasound
- Excretory urography
- Cystography
- CT scan
- Isotonic dynamic renography
- Angiography of the renal arteries
- Urological studies
- Gynecological examination of women with urinary tract infections
Differential diagnosis
Infectious diseases of the lower urinary tract can be associated with pyelonephritis, but can also be independent. In the presence of anterior hypertension, chronic pyelonephritis is differentiated from hypertension, vasorenal and other forms of hypertension. Radiography is important here.
Renal tuberculosis can be excluded if isolated leukocyturia is detected. Urine is cultured on special media, which makes it possible to detect the presence or absence of Mycobacterium tuberculosis. At the onset of acute pyelonephritis, there may be dyspeptic symptoms, which confuses the disease with foodborne toxic infections.
A differential diagnosis of pyelonephritis and chronic glomerulonephritis is required. In the latter, the lesion is bilateral, and lymphocytes predominate among leukocytes in the urine sediment. A bacteriological examination of urine does not detect the pathogen.
A focal formation in the kidney can indicate not only pyelonephritis, but also a cyst, abscess or kidney tumor. The diagnosis can be clarified using computed tomography or angiography.
Treatment of pyelonephritis
It is important to correct anatomical abnormalities that cause urodynamic disturbances. This could be, for example, a bladder diverticulum. If correction is not possible, a drug prophylaxis regimen is selected.
The basis of drug therapy is the use of antibiotics. Also relevant are small doses of loop diuretics (furosemide), nonsteroidal anti-inflammatory drugs, and medications to improve blood circulation in the venous and capillary beds of the kidneys. Before starting antibacterial treatment of acute pyelonephritis, you should ensure that there is no obstruction of the urinary tract.
p-Lactam antibiotics are used if the pathogens are gram-negative and gram-positive cocci and gram-positive rods. The following drugs are effective:
- oxacillin
- benzylpenicillin
- ampicillin
- antipseudomonal penicillins
Cephalosporins have bactericidal properties. The doctor may prescribe the following drugs: cephalexin, cefazolin, cefepime, cefamandole, cefuroxime, cefoperazone, cefotaxime, ceftazidime, ceftriaxone.
Aminoglycosides are relevant mainly for the treatment of nosocomial infections; they kill gram-negative bacteria. Vancomycin is used at a dose of 2 g per day. It acts on gram-positive and gram-negative bacteria.
Fluoroquinolones currently used are:
- ofloxacin
- ciprofloxacin
- levofloxacin
- norfloxacin
Macrolides are reserve drugs for affecting gram-positive cocci. They have almost no effect on gram-negative microflora. Erythromycin should be used 0.5 g 4 times a day. For infections caused by mycoplasma and chlamydia, drugs such as roxithromycin and azithromycin are relevant. Nitroxoline and other 8-hydroxyquinoline derivatives act against gram-negative microflora. They should be taken in a dose of OD g 4 times a day, the course is from 10 to 14 days.
To treat kidney infections caused by staphylococci, a combination of penicillins and β-lactamase inhibitors is used: sultamicillin, amoxicillin + clavulanic acid. Pseudomonas infections are difficult to treat. Often, 2-3 antipseudomonal antibiotics are combined for their treatment - drugs of the third generation of cephalosporins, fourth generation of penicillins, ciprofloxacin and gentamicin.
In uncomplicated pyelonephritis, when it is impossible to conduct a urine test, an antibacterial drug must be selected empirically. The prevailing pathogens in a given region are taken into account. The drugs of choice are mainly fluoroquinolones: ciprofloxacin, norfloxacin and others.
When pyelonephritis develops as part of a hospital infection, even before receiving the results of a bacteriological study, doctors generally prescribe fluoroquinolones to the patient. If nosocomial urosepsis is suspected, benzylpenicillin with gentamicin or imipenem with cilastatin or a cephalosporin with gentamicin should be prescribed. Urosepsis develops mainly in acute forms of pyelonephritis.
When kidney tissue is infected, it is important that the drug accumulates in the organ in sufficient concentration. And for lower urinary tract infections, the medicine should concentrate in the urine. In order to sanitize the lower urinary tract, a course of antibiotics is prescribed for 5-7 days. And long courses of antibiotics are important for upper urinary tract infections. Treatment for 6-8 weeks is relevant for relapses of pyelonephritis.
The best water regimen for antibacterial therapy of pyelonephritis involves administering fluid in fractional doses and excreting urine in a volume of 1.5 l/day. Excessive diuresis reduces their effectiveness. When treating with antibiotics, urine pH needs to be monitored. For alkaline urine, erythromycin and aminoglycosides are effective. And for an acidic reaction: tetracyclines, nitroxoline, penicillins, nalidixic acid, nitrofurans. Chloramphenicol is effective in both acidic and alkaline reactions. Acidifies urine:
- ascorbic acid,
- meat food products,
- citrus,
- methionine
A combination of bacteriostatic and bactericidal drugs is not recommended, because the antibacterial effect will be weaker. If kidney function is impaired, the doctor should pay attention to the nephrotoxicity of the antibiotic. Chloramphenicol, erythromycin, and oxacillin have minimal nephrotoxic effects. Slight nephrotoxicity with nitrofurans, ampicillin, nalidixic acid. In case of chronic renal failure, their dosage is reduced by 1/3.
If the patient is pregnant, choose antibiotics that are safe for the fetus. In the first trimester of pregnancy it is better to prescribe the following drugs:
- oxacillin,
- benzylpenicillin,
- nitrofurantoin,
- ampicillin.
From the second trimester, kidney pyelonephritis can be treated with erythromycin, cephalosporin, nitroxoline. Pregnant women have contraindications to chloramphenicol, streptomycin, sulfonamides, and tetracyclines. In women who breastfeed, small amounts of cephalosporins, penicillins and nitrofurantoin may accumulate in milk. When breastfeeding, you should not take chloramphenicol, aminoglycosides, sulfonamides, tetracyclines, cotrimoxazole.