Causes of pyelonephritis
Pyelonephritis is an inflammatory disease of one or both kidneys, which is provoked by microorganisms: Proteus, Staphylococcus, Enterococcus and Escherichia - they are the cause of pyelonephritis. Microbes enter the kidneys in several ways:
- along the urethra
. This happens in the case of reverse reflux of urine, when fluid moves from the bladder into the ureters.
- hematogenously
, i.e. with blood. If there is some kind of inflammatory process in the body (bronchitis, otitis, caries, sinusitis), then the infection can “move” from one source with the blood to the kidneys. True, in order for the pathogen to linger there, the outflow of urine must be disrupted.
- along the wall of the urinary tract
: The infection first develops in the wall of the ureter, and then “rises” higher and affects the kidneys.
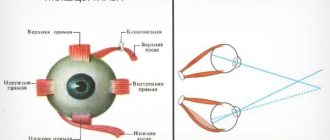
Once in the kidneys, the microbes trigger an inflammatory process in the collecting system (the area where blood is filtered) and the main tissue of the kidney. The infection can affect one kidney (unilateral pyelonephritis) or both (bilateral).
Fertile ground for pyelonephritis is created by some indirect causes, concomitant diseases and disorders: reduced immunity, hypothermia, cystitis, problems with the blood supply to the kidneys, urolithiasis (provokes calculous
or “stone” pyelonephritis), prostate adenoma and chronic prostatitis.
Sick leave
The risk group most often affected by pyelonephritis is the adult population, specialties whose work involves hypothermia, low temperatures, and outdoor work. Sick leave for pyelonephritis must be issued for the duration of treatment in the hospital. After discharge from the hospital, you are required to undergo an examination by a nephrologist or urologist at the clinic at your place of residence. He can also issue you a sick leave certificate for the duration of treatment, but the period of treatment at home is no more than 5-7 days. The kidneys recover from acute pyelonephritis after one month of effective treatment.
If the attending physician detects complications or worsening of the condition, he will recommend that you continue treatment in a hospital. With the chronic type of pyelonephritis, sick leave for incapacity for work is not given only if clinical tests and ultrasound show an exacerbation of the disease and incapacity for work is lost. And in this case, hospitalization will be recommended.
Pyelonephritis: symptoms
The main manifestations and symptoms of pyelonephritis: aching pain in the lower back and abdomen, high fever, weakness, chills, loss of appetite, cloudy urine (or urine with blood), nausea and vomiting. All these symptoms are nonspecific; they overlap with many other diseases. Therefore, you should not delay visiting a doctor: while you are treating your back or fighting a supposedly overcoming cold, the risk of complications of pyelonephritis increases - chronic and acute renal failure, purulent kidney damage.
How long are they in the hospital?
If you are interested specifically in how many days pyelonephritis is treated, then, for example, treatment of the acute form in adults takes place within 30 days. The course of therapy in a hospital under the supervision of a physician should be at least 7-14 days. After discharge, the patient receives consolidation therapy for half a month in the clinic at his place of residence. The most difficult thing for many patients after discharge from the hospital is to continue treatment at home. You must strictly follow the diet prescribed by your doctor.
Acute pyelonephritis is treated in most cases with a favorable outcome. Also, during the year you need to be observed by a nephrologist or urologist at the clinic at your place of residence and comply with all prescribed standards of treatment. In the chronic form of pyelonephritis, treatment in a hospital occurs only during exacerbation. The duration of hospitalization in this case depends on the level of exacerbation.
Phases of the disease: inflammation, latent, remission
Pyelonephritis has several stages, phases (inflammation, latent, remission):
- active inflammation phase: during this time the body fights infection
- the latent (hidden) phase can last up to six months. During this period, the patient’s condition and his test results gradually return to normal, and the inflammatory process subsides.
- remission is a phase in which there are no external manifestations of pyelonephritis and tests are normal, but under unfavorable conditions the disease returns again.
Diagnostic methods
In the acute form of the disease, hospitalization of the patient is required, so diagnosis takes place in a hospital setting. It includes examination with palpation and tapping of the lower back, taking temperature readings, laboratory and hardware tests.
Hardware diagnostic methods include ultrasound of the kidneys and x-rays with contrast. Carrying out MRI and CT allows you to study the features of the kidneys and blood vessels, identify developmental anomalies and obstructions. Laboratory tests include a complete blood count, which looks at ESR and white blood cell counts. Carrying out a biochemical analysis allows you to determine the content of potassium, creatinine, and urea. Serological tests help identify antibodies to the infectious agent. A bacteriological and general urine analysis, Zimnitsky test is required. Urinalysis according to Nechiporenko and Amburge allows you to see clearer values. If potassium levels deviate from normal, hemodialysis may be prescribed.
Stages: acute and chronic pyelonephritis
Inflammation of the kidneys (pyelonephritis) can be acute or chronic. For acute pyelonephritis
the entire parenchyma (ground tissue) of the kidney becomes inflamed. Sometimes paranephritis even develops: small purulent foci form in the kidney, which can merge into a large abscess - a carbuncle. If it bursts, pus will leak into the urine.
With improper or delayed treatment, acute pyelonephritis turns into chronic. The disease may not bother you for a long time, but if a person catches a cold, gets a sore throat or otitis media, or becomes hypothermic, pyelonephritis will worsen again. Such relapses usually occur a couple of times a year.
However, chronic pyelonephritis
– not always a consequence of undertreatment. There are other reasons: diseases that reduce immunity (diabetes mellitus, diseases of the gastrointestinal tract, prostate adenoma, urolithiasis), “addiction” of microbes to medications, etc.
Herbal medicine and diet
1. In the treatment of pyelonephritis, plant-based products are actively used. Taking them reduces the toxic load on the liver. Preparations containing chamomile, dill, yarrow, orthosiphon, bearberry, and string are used. Taking herbal remedies is especially effective during remission.
2. Nutritional correction is necessary throughout the entire period of treatment until complete recovery. This reduces the load on the kidneys and relieves inflammation. Basic dietary requirements:
- exclude salty, spicy foods;
- give up energy drinks, alcoholic drinks, coffee and tea;
- reduce the consumption of acidic foods, giving preference to slightly acidic ones;
- significantly reduce protein intake, in particular meat products;
- drink at least 2.5-3 liters of liquid per day to remove toxins.
3. It is necessary to strictly adhere to the doctor’s recommendations regarding treatment and nutrition. The main difficulty is the preservation of foci of inflammation, which cause relapses of the disease.
Development of pyelonephritis during pregnancy (gestational)
The uterus of a pregnant woman gradually enlarges, due to which neighboring organs (including the ureters that remove urine) are compressed, making it difficult to drain urine. Another “pregnant” factor of pyelonephritis leads to this – hormonal changes in the body. When urine stagnates in the renal pelvis, a favorable environment arises for the proliferation of pathogenic microorganisms and the development of inflammation, pyelonephritis.
Most often, pregnant women who have already had this disease or cystitis suffer from gestational pyelonephritis. In this case, the symptoms of pyelonephritis will be mild. If the disease attacked a woman for the first time, pyelonephritis will show itself “in all its glory.” The pregnant woman's temperature will rise sharply, severe headaches and muscle pains, chills, nausea, etc. will begin.
Is it possible to die
The disease pyelonephritis itself is not fatal, but if not treated on time, you can die from any disease. I want to live as long as possible, follow the diet, doctor’s prescriptions and supportive therapy, undergo scheduled examinations and tests on time.
In case of non-compliance with treatment standards, possible complications and pathologies are inevitable, which result in renal failure and can lead to death.
“How to live now with such a diagnosis?” you ask. Yes, in this case you need to be patient and persistent if you want a complete cure or long-term remission.
“People, how do you live?” is a desperate question from many sick people. Yes, of course, a complete cure may take more than one year. We must not forget about the required volume of water that you need. Nowadays there are a lot of fashionable thermoses and accessories for water, you can combine the useful and the pleasant. Avoid hypothermia, strengthen your immune system to reduce the risk of contracting viral diseases. Get scheduled check-ups with your doctor on time. Select herbal medicines in consultation with your doctor, taking into account their action and effect on your body. Drink herbal teas that help your kidneys.
Life does not end with a diagnosis of chronic pyelonephritis, it is curable. Live as you lived before, but taking precautions. Remember the catchphrase: “Water does not flow under a lying stone!” The duration of your life is in your hands.
In case of mild exacerbation and no signs of urinary tract obstruction, treatment is carried out in a “hospital at home”. In this case, doctors go to the patient’s home. Another option is day hospital therapy. In case of acute and obstructive pyelonephritis and exacerbation of its chronic form, treatment is carried out only in a hospital setting.
Pyelonephritis in children
Pyelonephritis in children often occurs due to dysbacteriosis or is a consequence of a previous illness - sore throat, flu, cystitis. In this case, we are talking about primary pyelonephritis, and secondary occurs due to congenital anomalies of the urinary system, for example, underdevelopment of the kidneys.
In addition to the symptoms common to all, kidney inflammation in children can manifest itself in urinary retention or incontinence, restless sleep, stool disturbances, changes in the color and smell of urine (it becomes dark, acquires a pungent odor). If your child experiences any of the above, you should consult a doctor.
Etiology and pathogenesis
With the development of acute inflammation, some people prefer to self-medicate, which is fraught with the development of purulent pyelonephritis. There are a number of provoking factors that contribute to the development of the disease:
- Escherichia coli is one of the most common pathogens;
- reduced body resistance, in which pathogenic mycobacteria rapidly develop (anemia, diabetes, autoimmune diseases);
- inflammation of the reproductive and urinary system;
- urolithiasis disease;
- abnormal arrangement of organs and vessels of the urinary system;
- oncological formations;
- the presence of blood clots in the renal vessels.
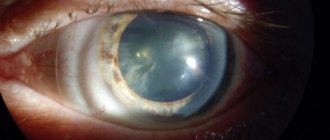
Possible renal pathologies
The disease may appear as a carbuncle on the organ. Acute purulent disease manifests itself in the following form:
- Apostematous pyelonephritis. Changes occur in the calyx and pelvis, small pustules begin to form.
- Abscess of a paired organ. The kidney is enlarged in size, and small ulcers merge with each other.
- Kidney carbuncle. It is a large abscess.
Treatment regimen for pyelonephritis in a hospital setting
There is a difference between outpatient and inpatient treatment. In the latter case, the patient is provided with rest, his nutrition is monitored, and his blood pressure is periodically measured. Antibiotics in a hospital can be administered using droppers, which cannot be done independently at home. In addition, doctors, if necessary, take tests from the patient to monitor the progress of treatment. The general treatment regimen includes:
- taking antibiotics for 4-6 weeks;
- strict bed rest;
- diet;
- drinking at least 2 liters of liquid in small portions.
After discharge, the patient continues to take antibiotics, but in tablets, and receives maintenance therapy in the clinic at his place of residence.
Patient mode
When a person first encounters acute pyelonephritis or its exacerbation, bed rest must be observed for 3-5 days. The motor mode is built taking into account the following principles:
- Activity increases if low back pain has decreased, dysuria has improved, and the temperature has decreased.
- Throughout the entire period of exacerbation, the patient needs to spend at least 3-4 hours in bed during the day and 10 hours at night.
- After the end of the relapse, a day's rest of 1.5-2 hours is recommended.
Drug therapy
For acute pyelonephritis, etiotropic and symptomatic therapy is carried out. The first is taking antibiotics to suppress the growth of bacteria, which cause kidney inflammation. Symptomatic treatment helps eliminate the signs of pyelonephritis. The main groups of medications prescribed by a doctor:
Average duration of use
Broad-spectrum antibiotics
Therapeutic diet
The diet for acute pyelonephritis should include a sufficient amount of proteins, fats and carbohydrates. The menu is built primarily from easily digestible products. Basic principles of the diet:
- Limit spicy, sour foods, alcohol, preservatives, fried foods, rich broths.
- For seasonings, use only red bell pepper or tomato puree.
- For arterial hypertension, reduce the daily amount of salt to 3-4 g.
- In addition to water, use a decoction of horsetail, cranberry juice, infusion of black currant leaves, birch, rose hips or strawberries.
- Consume fermented milk products: kefir, cottage cheese, sour cream.
- Include fruits and vegetables, cereals, and boiled meat in the menu.
- Stick to a daily caloric intake of 2500 kcal.
Physiotherapy
The indication for physiotherapy is to relieve the inflammatory process. They are not performed in case of active pyelonephritis, at the terminal stage of inflammation, or polycystic kidney disease. Basic methods of physiotherapy:
- ultrasound therapy;
- diathermy of the renal area;
- paraffin, mud and ozokerite applications to the kidney area;
- sodium chloride and carbon dioxide therapeutic baths;
- ultra-high frequency therapy;
- magnetic therapy;
- ultrasound procedures;
- laser therapy for each kidney;
- electrophoresis of antimicrobial drugs.
Additional treatments
For some individual manifestations of acute pyelonephritis, doctors resort to additional treatment methods. Their list includes the following procedures:
- Functional passive stimulation of the kidneys. Indication: deterioration of the process of urinary excretion. In the morning on an empty stomach, the patient takes 1-2 tablets of Furosemide. The procedure is performed 1-2 times a week.
- Taking non-steroidal anti-inflammatory drugs (NSAIDs). Indications: persistent leukocyturia, bacteriuria. The patient is prescribed 25 mg of Voltaren or Indomethacin 3 times a day for 6-8 weeks.
Surgical intervention
The main indication for surgery is secondary pyelonephritis. It occurs as an acute nonspecific inflammatory process against the background of other pathologies of the urinary system. Main types of surgical intervention:
- Catheterization of the ureter. This is the installation of an external or internal stent to restore urine passage.
- Percutaneous puncture nephrostomy. It is carried out for relatively long-term drainage of the kidneys, helps to avoid open surgery and, after 3-4 weeks, remove the stone using minimally invasive methods.
For some patients with acute pyelonephritis, doctors prescribe open surgery. Main indications for endoscopic operations:
- acute purulent pyelonephritis;
- negative dynamics of adequate antibiotic therapy;
- impossibility of draining the kidney using minimally invasive methods.
If other methods have failed, treatment for acute pyelonephritis is nephrectomy. This is an operation to remove a kidney, which is performed in the following cases:
- with signs of renal vessel thrombosis;
- with purulent inflammation of a non-functioning kidney;
- with multiple confluent carbuncles of the kidney;
- with purulent destruction of more than 2/3 of the kidney;
- purulent intoxication, toxic shock, decompensation of concomitant diseases.