Svetlana Shcherbakova
Cardiologist
Higher education:
Cardiologist
Kabardino-Balkarian State University named after. HM. Berbekova, Faculty of Medicine (KBSU) Level of education – Specialist 1994-2000
Additional education:
“Cardiology”
State Educational Institution “Institute for Advanced Training of Physicians” of the Ministry of Health and Social Development of Chuvashia
Contacts
Eye stroke is a fairly common pathology. 80% of people who have had an attack experience it. Vision loss can be partial or complete. Problems with the eyes arise in cases where the lesion is located in the segments responsible for feeding the visual centers of the brain. The severity of the patient’s condition directly depends on how much tissue was damaged during the attack. If a small segment is damaged, a person may develop a black spot in both eyes. Next, we'll talk about what to do if you have vision loss due to a stroke.
Causes
Occlusion of the vessels of the eye rarely occurs as an independent nosology. The condition is often a manifestation or complication of another, general somatic, pathology. Diseases and conditions that provoke occlusion of retinal vessels:
- atherosclerosis;
- increased blood pressure;
- carbohydrate metabolism disorder (diabetes mellitus);
- autoimmune inflammatory vascular diseases (giant cell arteritis);
- increased blood viscosity (polycythemia, myeloma);
- thrombophilia – congenital or acquired;
- endocarditis;
- viral and bacterial vascular diseases;
- congenital vascular anomalies;
- pathologies of heart valves (rheumatism, heart defects);
- heart rhythm disturbances;
- myocardial infarction, acute coronary syndrome;
- extensive and chronic blood loss;
- acute cerebrovascular accidents (stroke, transient ischemic attack);
- hyperthyroidism;
- long-term use of diuretics, oral contraceptives, blood clotting agents;
- invasive diagnostic methods associated with the administration of contrast agents (angiography).
Main causes of the disease:
All of the above factors provoke the formation of emboli or blood clots (blood clots interspersed with bacteria, calcium crystals, cholesterol). At one point, these structures break away from the arterial walls and, together with blood, enter the vascular network of the eye (disrupting the blood flow to the retina and cutting off the blood supply to the organ of vision).
Basically, blood clots (emboli), which pose a danger to the organ of vision, form in the carotid or coronary arteries. Under favorable conditions (CVS pathologies, infections, allergic reactions, eye injuries, blood clotting disorders), formations break away from the arterial walls and clog the central vessel of the visual organ.
Other reasons that provoke the symptoms of an ocular stroke include:
rupture (blockage) of the vertebral arteries (this phenomenon occurs with disc hernias, injuries, osteochondrosis);
- a sharp change in intracranial pressure (the nutrition of the visual organ is disrupted).
Depending on what type of ischemic disorder occurred in the retina, several types of pathology are distinguished:
- Central artery occlusion. The disease progresses at lightning speed, causing unilateral visual impairment. The patient does not distinguish colors. Timely laser treatment helps eliminate the consequences of the problem (impaired visual function).
Retinal vein division. White spots flash before the patient’s eyes (outwardly similar to glare of light). This form of stroke is unilateral. Timely diagnosis and treatment allow us to talk about a favorable prognosis.
- Arterial occlusion and retinal detachment. The most severe form of stroke. Peripheral vision is completely lost. The course of the disease is asymptomatic. In a number of clinical cases, retinal detachment is accompanied by spastic pain, and the carotid artery may narrow.
Often, partial or complete occlusion is caused by blockage of blood vessels with blood plaques (emboli). In one hundred percent of cases, occlusion of the central retinal artery manifests itself as a consequence of acute hypertensive abnormalities. The underlying factors in the development of occlusion of the central artery or retinal veins are diseases such as arrhythmia, diabetes mellitus, and antiphospholipid syndrome. Also provoking factors are hematomas and drusen of the optic disc, as well as the consequences of possible eye injuries.
Symptoms of ocular stroke due to occlusion of the central retinal artery:
- Partial or complete loss of peripheral vision, gradually developing into partial or complete blindness.
- Distorted image perception or the appearance of blind spots.
Such a deviation from the norm is considered one of the most dangerous, as it develops against the background of other spasmodic processes in the body - heart defects, hypertensive complications, defects of the spinal arteries. Often this disease is not accompanied by pain, and therefore a person does not pay attention to the symptoms that appear; however, prolonged occlusion of the central retinal artery (CRA) entails irreparable visual impairment.
How to restore vision
Restoration of vision after a stroke occurs when therapeutic measures are taken to eliminate or mitigate the symptoms of visual impairment. Complex treatment necessarily includes medications, eye exercises, and may require surgical intervention. Folk remedies used with the permission of the attending physician will provide good help.
Medications
Visual impairment during a stroke occurs due to damage to an area of the brain, so the prescription of drugs will depend on the type of stroke, the size and location of the damaged area of the brain. The following drugs are used:
- improve blood circulation;
- relieve swelling of brain tissue;
- increase the resistance of neurons to oxygen starvation;
- lower blood pressure;
- moisturize the mucous membranes of the eyes, etc.
Drugs and dosage are prescribed by the doctor individually, based on the patient’s condition, age and examination results.
Folk remedies
The course of rehabilitation after a stroke at home begins when the patient returns home, and can last for a period of up to two to three years. Some functions are restored faster than others, depending on the location of the vascular accident and the degree of brain damage. Although this is a long process, many patients, thanks to their perseverance and the help of loved ones, return to a full life.
Restoring vision at home is more effective using various folk methods, which are confirmed by many years of practice among those who have recovered.
It is important to remember that the choice of traditional medicine must be agreed with the general practitioner or neurologist observing the patient. Mainly used are decoctions and infusions of medicinal herbs, honey baths, tincture of pine cones, treatment with citrus fruits and other effective recipes that thin the blood and improve nutrition and restoration of brain structures
It is useful to eat nuts and dried fruits rich in microelements and potassium, as well as foods containing omega-3-polyunsaturated fatty acids necessary for normal brain function (sea fish, flaxseed oil, nuts, seeds, whole grains).
Gymnastics for the eyes
Therapeutic exercises are needed primarily for the eye muscles affected by the consequences of a stroke. Simple but constant exercise will strengthen the eye muscles, increase blood circulation, and help restore control over the movements of the eye muscles. You will need to do gymnastics for a long time and regularly, devoting 20-25 minutes to it every day. An approximate set of exercises to restore vision after a stroke:
- Eye movements left and right all the way, slowly and calmly. At the extreme point of the turn, try to stay for a second.
- Eye movements up and down, at the extreme point fix your gaze for a second.
- With maximum amplitude, make circular movements with your eyes clockwise, and then counterclockwise.
- Close your eyes tightly and count to 5 (slowly).
- Place three fingers on closed upper eyelids with light pressure and hold for a count of 5.
- Place the palms of your hands on your closed eyes, pressing lightly, and make rotational movements clockwise and counterclockwise (slowly).
- Select a point in front of you on an object, then look at the tip of your nose. Repeat 6-8 times.
- Blink your eyes frequently, counting to 5.
The number of repetitions can be increased over time from 6 to 30 times, avoiding the feeling of fatigue and discomfort in the visual organs.
Surgical intervention
Surgical treatment after a stroke is rarely used, in special cases, for example, when it is necessary to replace a clouded lens with an artificial one, which replaces the functions of the victim and vision is restored. Also, with severe strabismus, surgical correction of overly tense and, conversely, relaxed eye muscles may be required. Not in all cases, surgery helps to completely restore lost eye functions, but the possibility of achieving partial improvement of vision is quite high.
Treatment methods
The prognosis of the disease and the success of treatment depend primarily on the timeliness of providing medical care to the patient. The degree of spread of the lesion, the type of eye stroke, and the reason why it occurred also play a role. Therefore, treatment begins with the diagnosis of the underlying disease, then the affected vessel is identified and the type of occlusion is established.
Timely laser therapy, medications, and a healthy lifestyle can completely restore vision after an eye stroke.
To do this, a visual examination of the eyeball and fundus examination are performed. If required, an additional electronic scan of the vessels is performed, and the patient is referred for a consultation with a neurologist.
In modern medicine, the method of laser coagulation is mainly used. A targeted laser beam breaks up the blood clot in the eye and then removes it. The integrity of the veins and arteries is not impaired, blood supply and vision are restored. Also, with the help of such an operation, you can fix the retina in case of its detachment and remove degenerative changes in the fundus of the eye.
In some cases, it is more appropriate to carry out hyperbaric oxygen therapy. The patient is placed in a special pressure chamber, after which he is exposed to oxygen at high pressure.
It is impossible to cure a stroke of the visual organ using a non-surgical method, using only medications. But medications are necessary in the postoperative period.
The following groups of drugs are used:
- Antispasmodics.
- Medicines that thin the blood and prevent the formation of blood clots.
- Medicines that stimulate blood circulation.
- Angioprotectors are medications that strengthen and protect blood vessels from damage.
- If blood pressure increases, use hypertensive drugs.
- Antibacterial drugs in case of infection.
- Medicines for the treatment of concomitant chronic diseases.
After an eye stroke, only an integrated approach, including the use of eye drops and vitamins, as well as special exercises, will help restore and maintain vision.
The drug therapy regimen is drawn up only by a doctor. He determines the combination of drugs needed and their dosage. Self-medication in this case will not give a positive result and will only worsen the patient’s condition. The earlier treatment is started, the better the prognosis. It is important to restore normal blood supply to the visual organs in the first hours after occlusion.
If therapy is carried out on time and correctly, vision can be completely restored. It is possible that small defects will remain in the form of flies and spots, but the quality of life will not be affected. If the symptoms are ignored, treatment does not begin or is carried out incorrectly, degenerative changes in the retina will progress, which will ultimately lead to loss of vision.
Cortical blindness
Cortical blindness
is a complete lack of vision caused by damage to the occipital lobes of the brain. It manifests itself as a violation of visual perception with intact reaction of the pupils to light. With the congenital variant of the disease, difficulties are observed in the development of speech and motor activity in the child.
For diagnosis, visometry, perimetry, ophthalmoscopy, head CT, electroencephalography, echoencephalography are used. Etiotropic therapy is reduced to eliminating the underlying disease. Drug treatment is indicated for malignant hypertension and encephalopathy.
Surgery is used for arteriovenous malformations.
Cortical blindness was first described by the Spanish ophthalmologist Marquis in 1934. The prevalence of pathology in the general structure of blindness is 5-7%. In 48% of patients, the etiology of the disease is associated with prenatal damage to the central nervous system.
In children under 3 years of age, the most common cause is postgeniculate visual lesions. With encephalopathy, damage to the organ of vision is observed in 15-20% of cases. In 63% of patients, the paroxysmal type occurs, while the permanent type occurs in 37%. Pathology can develop at any age.
Men and women get sick with the same frequency. Geographical distribution features have not been described.
Cortical blindness
The disease often occurs sporadically. The development of the congenital form is potentiated by intrauterine hypoxia, toxemia of pregnant women, and brain damage by viral agents when the fetus is infected during pregnancy. The etiology of the acquired form is due to:
- Hypoxic-ischemic encephalopathy
. An insufficient number of anastomoses between the cortical branches of the middle and posterior cerebral arteries in the region of the occipital cortex leads to ischemia of this area. Hypoxic changes lead to impairment of central (macular) vision. - Malignant arterial hypertension
. When blood pressure rises above 220/130 mm. Hg Art. swelling of the optic disc occurs with the formation of multiple zones of hemorrhage and exudation in the fundus, however, blindness of central origin can occur only with an increase in the clinical picture of hypertensive encephalopathy. - Progressive multifocal leukoencephalopathy (PML)
. PML is a rapidly progressive demyelinating pathology of the central nervous system, in which asymmetric damage to the cortex is observed. This disease often causes the development of hemianopsia, less often - complete cortical blindness. - Arteriovenous malformations (AVMs)
. Against the background of pathological changes in blood vessels, hemorrhages occur in the brain tissue. The organization of a blood clot entails irreversible changes in the affected area. When the bleeding area spreads to the occipital lobe, vision loss occurs. - Pathological neoplasms
. When space-occupying lesions are localized in the occipital lobe, destruction of the neural network occurs with irreversible visual dysfunction. - Head injury
. Cortical blindness develops from traumatic injuries in the visual cortex. - A sharp increase in intracranial pressure
. Intracranial hypertension leads to compression of brain structures and temporary visual dysfunction.
Cortical blindness occurs only in the case of total damage to the occipital region of the cerebral cortex. Additionally, Graziole optic radiance may be involved in the pathological process. With unilateral damage to the occipital lobe, a congruent central scotoma appears.
Color agnosia is characteristic of an isolated pathology localized in the occipital lobe of the left hemisphere. The function of the macular areas is not impaired. Bilateral damage leads to complete blindness, which is often accompanied by achromatopsia, apraxia of conjugate eye movements.
With concomitant damage to the speech centers, dysphasia develops.
In most cases, cerebral blindness is an acquired pathology. Congenital cases are extremely rare. Clinical classification includes the following forms of the disease:
- Permanent
. The most common option. Develops with irreversible damage to brain structures due to hemorrhagic stroke. - Paroxysmal
. This is a reversible blindness that occurs more often at a young age. Occurs against the background of metabolic disorders, hypertensive crisis, hydrocephalus.
The first manifestations of pathology are the loss of certain areas from the field of view. Patients complain of the appearance of cloudiness, “veils” before the eyes, and impaired orientation in space.
Patients cannot direct their gaze towards an object that is located in the peripheral regions. The progression of the pathological process leads to a total impairment of visual perception.
Pupillary response to light is preserved because the nerve pathways from the retina to the brainstem are functioning normally. Patients note that when looking at a light source, there is no reflexive closing of the eyelids.
Patients react to loud sounds by turning their heads and moving their eyes towards the source of irritation. In children with congenital cortical blindness, a common concomitant manifestation is dysphasia (impaired speech production).
If visual dysfunction is combined with an inability to distinguish colors and shades, this indicates a unilateral lesion. As the disease develops against the background of functional lesions of the cortex, the symptoms regress on their own.
Visual acuity is restored after 3-4 days. First, light perception occurs, then object vision occurs, then patients note regeneration of the color perception function. The disease is isolated.
In rare cases, concomitant cortical disorders are observed in the form of alexia (inability to understand written text), hemichromatopsia (loss of color sensitivity in one half of the visual field).
Patients also complain of memory impairment and unilateral muscle weakness (hemiparesis). With extensive damage to brain tissue, concomitant neurological symptoms are detected.
The congenital variant of the disease is complicated by a delay in the formation of motor skills and spoken language. When pathology occurs in adulthood, the patient’s adaptation to the social environment is greatly complicated. Patients with cortical blindness are at high risk of developing vestibulopathy.
Complications of blindness of cerebral origin are largely determined by the nature of the underlying disease. With the hypertensive etiology of the disease, there is a high probability of hemorrhages in the anterior chamber of the eye or the vitreous body.
With multifocal leukoencephalopathy, the spread of infection to nearby areas leads to memory loss, speech impairment, and movement disorders.
The diagnosis is based on medical history and the results of specific examination methods. Cortical blindness is supported by such anamnestic information as the connection between the first manifestations of the disease and traumatic injuries, brain infections, and increased blood pressure. Instrumental diagnostics is based on:
- Ophthalmoscopy
. When examining the fundus, pathological changes are revealed only if the disease is hypertensive. Swelling of the optic disc and local areas of hemorrhage on the inner membrane are visually determined. - Visometry
. In the initial stages, visual acuity is slightly reduced. The progression of the pathology leads to amaurosis. - Perimetry
. Allows you to identify visual field defects in the form of concentric narrowing or loss of individual halves at the initial stages of pathogenesis. In the terminal stage, peripheral vision is absent. - CT scan of the head
. Computed tomography is used to visualize organic damage to the cortical brain centers and pathological neoplasms. - Electrophysiological study (EEG)
. In hypoxic encephalopathy or multifocal leukoencephalopathy, the EEG reveals diffuse disorganization of bioelectrical activity. Epiactivity is uncharacteristic. - Echoencephalography (Echo-EG)
. With the development of visual dysfunction in individuals with intracranial hypertension or hypertensive encephalopathy, it is possible to diagnose signs of increased intracranial pressure.
Etiotropic therapy is based on eliminating the underlying disease. Symptomatic treatment is effective only in the early stages. All patients with a history of hypertension should have their blood pressure monitored. If the disease is malignant, antihypertensive therapy is indicated.
For ischemic encephalopathy, it is advisable to use pentoxifylline, vinpocetine, and nicergoline. Planned surgical intervention is performed for cerebral AVM, as well as for epidural hematoma in patients with traumatic brain injury.
Treatment tactics for cortical blindness in patients with multifocal leukoencephalopathy and congenital forms have not been developed.
The prognosis for life and work ability is determined by the nature of the damage to brain structures. Often visual dysfunction is irreversible, but in some cases spontaneous remission is observed. There are no specific methods of prevention.
Nonspecific preventive measures are reduced to the prevention of perinatal pathology and intrauterine hypoxia. Patients suffering from malignant hypertension need to monitor their blood pressure levels daily.
The development of visual dysfunction in the absence of objective signs of eye damage requires a detailed examination of the brain structures.
Source: https://www.KrasotaiMedicina.ru/diseases/ophthalmology/cortical-blindness
What is an ocular stroke?
When an eye stroke occurs, the veins or arteries in the retina stop working as expected. They are blocked by a blood clot or narrowing of a blood vessel.
Similar to a cerebral stroke, in which blood circulation to the brain is reduced or cut off, the retina of the eye loses blood supply. Blood and fluid can leak into the retina and cause swelling. Both the retina and a person's vision can be quickly damaged.
There are several different types of ocular strokes, depending on the blood vessel affected:
- Central retinal occlusion (CRVO): The main retinal vein is blocked.
- Central retinal artery occlusion (CRAO): The central retinal artery is blocked.
- Retinal occlusion (BRVO): The small veins of the retina are blocked.
- Branch retinal artery occlusion (ARAO): Small retinal arteries become blocked.
Some people may have a higher risk of stroke than others. The risk factors are similar to those for regular stroke.
The American Academy of Ophthalmology says people over age 60, especially men, may have the highest risk of eye stroke.
Impact of stroke on vision
Stroke is a systemic disorder of the blood circulation of the brain, which provokes the development of irreversible phenomena leading to the loss of important body functions. If the optic nerve is located closer to the brain structures, it suffers during hemorrhage. As a result, the patient develops blindness, strabismus, night blindness and vision diseases.
There are signs that determine the degree of brain damage:
- The appearance of a “blind spot”. If the brain is slightly damaged, then some fields of vision may fall out. The phenomenon is called a “blind spot”. A person sees normally, but some small area falls out of sight. There is pain in the eyes. If the disturbances are minimal, then vision after a stroke will recover on its own. Rehabilitation is necessary, then performing gymnastics for the eyes;
- Loss of peripheral vision. Severe damage affects visual functions, for which both halves of the brain are responsible. A large area of the brain is affected, causing loss of peripheral vision. Impaired lateral vision is restored with the help of intensive therapy;
- Atrophy of the optic nerve. Due to atrophic phenomena, paralysis of the oculomotor nerve may develop, due to which the patient cannot control eye movements. Strabismus, protrusion of the eyeball and other pathologies may develop.
Taking into account the statistics, we can say that men aged 45-60 years are susceptible to stroke accompanied by visual impairment. In addition to visual functions, harm is caused to the body. If the disease is discovered and treatment is started, then in one case out of three there is a chance of recovery and restoration of lost functions.
At-risk groups
Most patients who suffered an ocular stroke suffered from atherosclerosis and its manifestations (cardiac ischemia, angina, hypertension), and diabetes. The next position as a direct etiological factor is occupied by rheumatic pathologies, then temporal arteritis, vascular diseases.
Additional risk groups:
- people whose work activity involves working at a computer (eye strain);
- people exposed to frequent and prolonged stressful situations (doctors, lawyers, military personnel and emergency responders);
- age over 40 years;
- smokers;
- persons who abuse alcohol;
- frequently ill people (decreased immunity);
- family history of atherosclerosis, hypertension, diabetes, heart and vascular diseases.
Prevention
Prevention comes down to the treatment and prevention of affecting diseases. Regular visits to a therapist, vision and fundus examinations should be carried out at least once a year.
Precautionary measures:
- avoid eye strain, wear safety glasses when working with a computer and telephone;
- avoid smoking, drinking alcohol;
- dose physical and emotional stress;
- maintain a sleep-wake schedule;
- do not take any medications without first consulting your doctor;
- know and treat chronic and hereditary pathologies;
- take courses of vitamin complexes to improve immunity, especially in the spring and autumn.
Taking precautions and knowing the basic symptoms and methods of recognizing an eye stroke will help you avoid such a terrible condition. If this happens, react in time and correctly and maintain your health.
Eye stroke and its symptoms
The main “bells” when detecting an ocular stroke:
- increasing weakening of vision or its temporary loss;
- deterioration of peripheral vision;
- violation of color perception;
- “glares” in the eye, white spots, hemorrhages;
- Dropping areas appear in the field of view.
It should be understood that if at least one of these symptoms appears, you should immediately make an appointment with an ophthalmologist - diagnosing a possible circulatory disorder and its timely treatment will help save or minimize the consequences of an eye stroke.
General symptoms of ocular stroke development include:
- in short-term or progressive loss of visual abilities;
- in a gradual decrease in peripheral vision;
- in the appearance of spots that are white or light in color;
- there are glare effects;
- in the spread of other interference that interferes with vision, the most common is the “curtain” effect;
- unexpected disappearance of areas of the visual field;
- decreased color sensitivity.
It is necessary to carefully monitor your well-being; if any of the listed signs, or a group of them, appear, you should immediately go to see an ophthalmologist. This need is due to the fact that timely detection of pathology of the ocular circulation and its further correct treatment will help you preserve your vision, as well as restore your visual abilities as much as possible after an attack.
If the central retinal artery becomes blocked, causing an ocular stroke, the following symptoms will occur:
- peripheral vision will be completely or partially lost;
- the previous symptom gradually develops into loss of central vision, which is partial or complete. This pathology occurs due to retinal detachment;
- Blind spots are increasingly emerging;
- the outlines of objects are distorted;
- the holistic perception of visual material is distorted.
This pathology, which develops as a consequence of an ocular stroke, is a most dangerous human condition. It often develops as a result of a strong spasm, and can also be caused by a narrowing of the carotid artery, disorders in the arteries of the spine, dangerous cardiac pathologies, and low-grade hypertension.
Usually this condition does not cause pain, so people pay little attention to the alarming symptoms that appear. However, prolonged blockage of the artery can cause the development of irreversible damage to the retina and also cause blindness.
This type of pathology develops due to failures of the venous outflow from the ocular vessels located in the retinal area. In other words, there is a blockage of its central vein. The cause of this pathological process is blood clotting failures in people who suffer from diabetes, atherosclerosis or other unhealthy vascular conditions. Typically, patients experience the following symptoms:
- vision noticeably deteriorates;
- first, peripheral vision decreases and is lost, and then the same changes occur with central vision;
- the outlines of objects lose their clarity and color saturation;
- glare appears, characterized by floating movement;
- regular cloudiness is felt;
- some areas of vision are lost;
- Mostly unilateral ocular involvement is noticed.
It is worth considering that the symptoms develop in close relationship with the degree of obstruction, they are unforeseen in nature and continue to develop more and more in the future. Typically, the path of its development takes a period of time from a couple of hours to a couple of days.
This pathology is a consequence of the formation of a cerebral infarction or the onset of hemorrhage in the part of the brain responsible for the center of gaze, as well as in the centers responsible for eye movements, optic chiasm and lobes of the brain.
Usually accompanied by the following symptoms:
- the appearance of unexpected blindness, an active decrease in visual ability in the area of one eyeball;
- disturbances in the motor abilities of the eye occur;
- numbness appears in one-sided limbs (opposite to the affected eye);
- visual fields begin to fall out, but the sense of color and visual acuity remain;
- severe pain develops, which is acute;
- the pupil narrows;
- there is a splitting of objects;
- blindness appears in half of the eye (on the side opposite to the pathology);
- strabismus may develop.
Ocular strokes are usually painless. A sudden change in a person's vision or loss of vision in one eye is often the first symptom of a stroke.
Vision loss may affect the entire eye or be less noticeable. Some people experience only loss of peripheral vision or have blind spots or floaters. Blurred or distorted vision may also occur. Vision changes may start out mild and then get worse over a few hours or days.
A brain stroke, which affects blood flow to the brain, can also cause sudden vision loss or changes in vision. For this reason, any sudden changes in vision require emergency medical attention.
The longer any stroke goes untreated, the more likely it is that the affected organs will be permanently damaged.
The main symptom of retinal artery occlusion is loss of visual fields. The sign is disturbing either in one or both eyes. The symptom develops suddenly. Sometimes the first signs of the disease are the appearance of glare, sparks, flickering, and mild pain in the orbit. Rapidly passing blindness is rarely a concern.
As with arterial occlusion, with venous thrombosis, symptoms develop suddenly, against the background of good health. Before the main symptom, patients are often bothered by fog before the eyes, a dark spot, image distortion, and dull pain in the depths of the orbit.
Symptoms of an eye stroke are painless and can be mistaken for a minor temporary deterioration due to fatigue or stress. This is a misconception. If the above symptoms appear, you should immediately call for medical help.
Recovery from vision loss after stroke
A stroke is an acute sudden disruption in the blood supply to the brain. A blood vessel ruptures, followed by bleeding in the brain (hemorrhagic stroke), or it is blocked by a blood clot or plaque (ischemic stroke).
The flow of blood to parts of the brain becomes difficult or stops. This dangerous disease leads to serious complications. Sometimes vision loss may occur. To restore vision after a stroke, complex and serious rehabilitation is necessary.
Causes of vision loss after stroke
A stroke can leave a person disabled, blind and dependent on others for help. The development of the disease is fraught with loss of skills and functions. The most common conditions are:
- speech disorder;
- weakening or complete absence of sensitivity in the limbs;
- problems with the ability to see (thirty percent of patients);
- disorder of thinking and memory.
Further prognosis for the course of the disease and the recovery process depend on the affected part of the brain and how strong the negative changes in it were.
Clogged blood vessels that supply blood to the brain compromise the body's recovery. A person will need a lot of time to recover, because the active course of the process threatens to deplete areas of the brain.
Vision may return if a small area of the brain is affected. For this, it is important to start treatment measures as soon as possible.
Other visual impairments after stroke
When a person is hospitalized, accompanying symptoms can tell about the extent of his brain damage due to a stroke.
Interesting: Acupuncture after a stroke: helps or not
The following eye pathologies are observed:
- loss of parts of the visual field;
- peripheral vision disappears;
- oculomotor nerve palsy.
When a person does not see a small segment and this is accompanied by pain in the eyes, this indicates a violation of the anatomical integrity of a small part of the brain. In this state of affairs, a series of special exercises that restore eye function will help restore visual ability.
In case of paralysis of the ocular nerve process, the situation is complicated by damage to the fibers and muscles that cause the movement of the eyeball. It is often accompanied by:
- a veil over the eyes;
- turning apples in different directions;
- alternate deviation of one or both eyes when looking straight;
- the appearance of hallucinations;
- bulging eyeballs;
- inability to look straight.
All these phenomena are often reversible, but only if diagnosed in a timely manner and undergo the prescribed intensive therapy.
In some cases, the eyes do not open or close if the nerve close to the brain is affected; Due to the drying of the cornea, tear production increases. If you do not take action, you may experience complete loss of vision after a stroke, and then it will be impossible to return it.
Let's look at common types of visual impairment after a stroke.
Ghosting
Disorders of the cranial nerves cause double vision (diplopia) - a deviation in which one object appears as two images displaced horizontally, diagonally, vertically (or horizontally and vertically at the same time) or rotated away from each other.
This pathology is often caused by problems in the work of the extraocular muscles, in which the eyes function, but do not converge on a specific object. This causes problems with movement, balance and affects reading.
Strabismus
Strabismus is a violation of the coordinated functioning of the eyes, which occurs as a result of deviation of the visual axes from the line of movement towards the object in question. With strabismus, it is difficult to fix both eyes on an object.
Interesting: Drugs that improve blood circulation in the brain
There are concomitant and paralytic strabismus.
In the first case, the entire range of movements of the apples is preserved, there is no double vision and binocular vision is not impaired (both eyes simultaneously see a clear image of the object).
Paralytic strabismus is the result of paralysis or damage to one or more extraocular muscles. It is caused by pathological processes in which the brain, muscles or nerves themselves are affected.
Foggy eyes
Blocked blood vessels during a stroke reduce the flow of oxygen to the eyes. This causes a feeling of blurred vision.
How to restore vision after a stroke?
There are three ways to restore vision lost due to a stroke:
- drug treatment;
- a set of rehabilitation exercises for eye gymnastics;
- surgical intervention.
Doctors prescribe medications after analyzing the overall picture of the onset and course of the disease. Their goal is to improve blood supply to the brain and metabolic processes in nerve cells. It is not necessary to use special ophthalmic preparations, except for moisturizing drops.
Ophthalmologists add medications to restore blood supply and stabilize metabolic processes in nerve cells if optic nerve atrophy is diagnosed.
Homeopathic remedies are also used to treat patients with impaired vision.
In difficult cases, ophthalmological surgeons perform operations after which vision functions are restored.
Restoring vision after a stroke at home
Restoring vision after a stroke is a serious and difficult job, especially if it is carried out not in a hospital, but at home. It will take strength and patience. So, let's list the available recommendations.
- Doing eye exercises regularly.
- Special floor covering. Massage mats placed in the places where the patient most often moves will stimulate the nerve endings located on the toes, positively affecting brain function.
- Photos. Viewing pictures depicting family members, close acquaintances, pleasant fragments from the past will force a person to activate thought processes and memory.
- Bright spots. Equip your living space with a variety of brightly colored items. They will be a good option for an eye trainer.
- You need to include foods high in vitamin A in your diet.
- Massage and compresses for the eyes. Has a calming effect on the eyes.
Interesting: Consequences and prognosis for life with ischemic stroke
When can peripheral vision recover after a stroke?
Peripheral vision is the part of viewing space with the gaze in a stationary position, which occurs outside the center of gaze. In other words, it is non-central vision. When it is impaired due to illness, a person does not see objects located on his right and left sides. To see them, he turns his head.
Failures in peripheral vision indicate profound painful changes in the brain. But when necrosis of the affected tissues occurs, the remaining healthy ones are able to perform the functions of the dead sections. Together with medication and physical rehabilitation, this makes it possible to restore vision after a stroke.
Can vision be fully restored after a stroke?
There are many factors and circumstances that influence how vision is restored after a stroke.
It depends on how soon the person was brought to a medical facility, how severely the part of the brain was affected, how accurately and carefully the doctor analyzed the data of the admitted patient and prescribed treatment accordingly. It is important to begin rehabilitation on the first day of illness. This will give you a chance to regain full vision.
Source: //golovaibolit.ru/insult/vosstanovlenie-zrenija-posle-insulta
Classification of apoplexy
There are two forms of stroke:
- Ischemic;
- Hemorrhagic.
Ischemic stroke is caused by an acute decrease in blood flow (ischemia), usually due to a blood clot that blocks a blood vessel in the brain. This form of apoplexy is the most common type of stroke, accounting for 80 to 85% of all strokes.
An ischemic stroke in the brain stem has especially serious consequences, because vital centers that are responsible for breathing control and consciousness are located there. An example of a brainstem infarction is thrombosis of the basilar artery: in severe cases, this causes complete paralysis of all limbs (tetraparesis) and coma or immediate death.
Ischemia
Hemorrhagic stroke
Hemorrhagic stroke occurs when abnormalities in the coagulation system, high blood pressure, or pathological changes in the vessel wall lead to bleeding in the brain. Between 15 and 20 percent of all apoplexies fall into this category.
Almost a million people in Russia suffer from apoplexy every year. 900,000 of them have their first stroke. Apoplexy occurs mainly in older people. As their proportion of the population steadily increases, the number of stroke patients is likely to increase as well.
Brain strokes mainly affect older people, but can also occur at a young age. Even newborn children in the mother's body can already have apoplexy. Possible causes include coagulation disorders and cardiovascular pathologies. Sometimes an infectious disease causes bleeding in the brain tissue in children.
In Russia, apoplexy is diagnosed every year in about 1,000 children and adolescents. However, experts believe the actual number is much higher because diagnosing stroke in children is more difficult. The reason is that brain maturation has not yet been completed, so apoplexy in children is often detected only after several months or years. For example, partial paralysis does not appear in infants until six months later.
Types of eye stroke
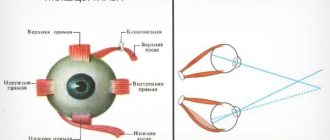
An ocular stroke can be localized in the venous or arterial bed of the retinal circulatory system. If the accident occurred in a venous vessel, they speak of retinal vein thrombosis. The blockage can occur in the central retinal vein (CRV) or in its branches (the superior temporal branch is affected in 82% of cases). A major role in retinal vein occlusion is played by disruption of the internal vascular epithelium, which predisposes to the formation of blood clots.
Obstruction of outflow leads to stagnation of blood and increased intravenous pressure. In this case, the liquid begins to seep through the walls of the vessel. Their rupture may also occur. Blood fills the eye space, swelling increases, and intraocular pressure increases even more. This is fraught with compression of small capillaries, which further limits the outflow of fluid and aggravates retinal hypoxia. This cycle of mechanisms of the pathological process is called a “vicious circle”.
Closure of the lumen of an arterial vessel is called arterial occlusion. There are occlusions of the central retinal artery (CRA), its branches and the cilioretinal artery. Often the blockage occurs in the CAS; the branches are affected with less frequency. The cause of artery blockage in most cases is cholesterol, fibrin thrombus or calcification embolism.
The embolus blocks the access of nutrition to the retina - ischemia develops. Clinical symptoms of visual impairment develop quickly. If medical assistance is provided within the first 40 minutes from the onset of symptoms, vision can still be fully restored. Delaying therapy threatens irreversible consequences.
Therapeutic measures
Only constant monitoring of vision will allow you to identify vision disorders and promptly contact an ophthalmologist and neurologist. The method of treating the pathological process depends on the type of stroke, the severity of the symptoms that occur, the severity of the course, causes and concomitant diseases. Timely medical care is also of great importance in successful treatment.
Read also: Exercises after a stroke
The most commonly used and effective treatment for eye stroke is laser correction. During the procedure, laser radiation is applied to the clot that has formed and blocked the lumen of the vessel. As a result, the blood clot is destroyed and the blood supply to the organ of vision is restored.
In addition, laser treatment is performed for retinal detachment, as well as as a result of degenerative changes in the visual organ.
The use of laser therapy together with the timely elimination of the main cause of the pathology in a short time allows for restoration of vision without the development of negative consequences.
Less commonly used is the treatment of hyperbaric oxygenation (HBO), which is a unique technique for supersaturating the blood with oxygen. The therapy is carried out in specialized hyperbaric pressure chambers, which use oxygen under high pressure.
To eliminate spasms, improve blood circulation, and lower blood pressure, drug therapy is prescribed. It is carried out under the supervision of an ophthalmologist at home or in an inpatient department.
Drug treatment consists of:
- drugs to prevent blood clots;
- antispasmodics;
- vascular drugs to improve blood circulation;
- angioprotective agents;
- in cases of the addition of an infectious pathogen, antibacterial drugs are prescribed;
- medications to normalize blood pressure and eye pressure.
You can learn about taking vasodilator drugs for various diseases, their benefits and possible harm from this article.
To increase the effectiveness of treatment, patients are advised to adhere to certain rules:
- adjust your diet: give up fatty and fried foods, reduce salt intake, include a large amount of vegetables and fruits in your daily diet;
- perform eye exercises;
- spend enough time outdoors, reduce television viewing;
- adhere to proper rest and sleep;
- exclude alcoholic drinks and smoking.
diagnosing
Sudden vision loss is a medical emergency.
To diagnose an eye stroke, doctors may need to perform tests on the retina. These may include
- Eye dilation with drops for easier vision on the retina.
- Using a dye and camera to take photographs of the retina, known as fluorescein angiography. The dye is injected through the arm and allows the doctor to better see the veins and arteries of the retina.
- Checking the pressure in the eyes using air flow.
- A slit lamp examination, which uses eye drops, a special light, and a microscope to examine the inside of the eyes.
- Vision tests, such as reading eye charts and testing side or peripheral vision.
These tests are painless and are performed by an eye doctor known as an ophthalmologist.
Diagnostics
Methods for diagnosing ocular stroke As a rule, diagnosis of the abnormality is carried out in a hospital. As soon as a person develops the first symptoms of pathology, he urgently needs to be examined by a neurologist. The doctor will evaluate the patient's reflexes, speech, vision and spatial orientation. If the suspicion of an ocular stroke is confirmed, a consultation with an ophthalmologist is scheduled.
The following methods can be used in the diagnostic process:
- CT angiography (visualization of blood vessels).
These instrumental methods help identify the location and degree of occlusion, and also help determine the course of treatment. To detect malformations, vascular aneurysms and other pathologies, radiography is often also prescribed, and ultrasound and ECG can be used to identify the causes of eye stroke. Laboratory tests also play an equally important role in diagnosis: urine and blood tests help determine the concentration of glucose, as well as the presence of electrolytes and kidney metabolites.
Prevention
Testing for cardiovascular disease is key to preventing ocular strokes. This may include regular cholesterol and blood pressure checks, as well as discussion of other risk factors for heart disease, such as family history, diet and lifestyle.
Heart disease risk factors play a role in the risk of ocular strokes. An article in the journal Eyes found that 64% of people had at least one new, undiagnosed risk factor for heart disease that was discovered after a stroke. The biggest factor for these people was high cholesterol.
In general, to maintain healthy blood vessels and prevent eye stroke, people should do the following:
- exercise regularly; The Physical Activity Guidelines for Americans recommend 2.5 hours per week.
- Eat a healthy diet including plenty of fruits, vegetables, whole grains and unsaturated fats.
- work with a nutritionist, as recommended for some people.
- avoid smoking or quit smoking
- work with your doctor to treat other conditions, such as diabetes.
Folk remedies
The following recipes are effective for restoring vision after a stroke:
- Take young pine cones and pour warm water (half a glass per cone). Boil for 10 minutes, strain after cooling. Take the product three times a day, 50 ml.
- Grind the parsley roots, add honey and lemon juice. You should take the product one teaspoon one and a half hours before meals.
- Pour mountain arnica with water (2 cups of liquid per 1 tablespoon of raw material). Boil for 15 minutes over low heat. When the broth has cooled, strain it. Drink 1 tbsp. l. three times a day.
- Pour 3 tbsp. l. creeping wheatgrass with a liter of water, cook for an hour. Take the product 5-6 times a day, 1 tbsp. l.
- Take cornflower petals and medicinal eyebright, 1 tbsp. l., pour half a liter of water and cook until the volume is halved. When the broth has cooled, strain it. Drink in 3 doses before meals.
- Grind the elderberries in a meat grinder, place the resulting mass in a jar and keep in the sun for 2 days. The juice should be squeezed out and taken a teaspoon half an hour before meals three times a day.
Read also: Legs fail after a stroke
It is important to enrich your diet. The following products are useful for restoring vision:
- carrots and fresh juice from them;
- blueberry;
- black currant;
- spinach;
- apricots, fresh juice from them, dried apricots;
- cottage cheese;
- fish and fish oil;
- sprouted wheat;
- onion.
Complications and consequences
Treatment is based on identifying the type of ocular stroke. If you feel the primary symptoms, you need to urgently contact an ophthalmologist, so that the doctor examines the eyeballs and fundus of the eye, prescribes an electronic analysis of blood vessels, and sends you to an appointment with a neurologist. Diagnostic results determine treatment methods for ocular stroke.
Therapy and consequences depend on the severity of the obstruction, as well as the time of progression of the pathology. In the early stages, treatment is effective and allows you to fully or maximally restore all impaired functions. In the later stages, laser surgery is actively used to treat ocular stroke, which helps to partially restore most visual functions.
There are times when problems still remain. Usually this is a distortion of objective perception, the appearance of blind spots, and loss of visual fields. The rehabilitation period consists of proper nutrition, taking vitamins and undergoing a course of therapeutic eye gymnastics under the supervision of an experienced trainer-doctor.
Visual impairment can become irreversible after a stroke, even leading to blindness, if timely assistance is not provided to the patient. This is the main and most dangerous complication of the disease. An equally serious consequence is retinal detachment and macular defects, which also leads to vision loss. The transition of the pathological process to the second eye and optic nerve atrophy occur less frequently.
When the retina lacks nutrition, the body begins to come up with workarounds. This is how new blood vessels form – neovascularization. This is not a healing process - the new vessels are too brittle and tortuous, and the risk of rupture is high. There are known cases of neovascularization of the optic nerve head and neovascular glaucoma.
Why does vision loss occur?
In case of vascular diseases, there is a disturbance in the activity of the brain, because The blood supply to this organ is not complete, which leads to damage to brain tissue. Some cells responsible for visual function die. Restoring vision is a long process. It is impossible to regenerate dead cells, so other healthy neurocells must begin to perform their tasks.
Visual impairment due to stroke can vary in severity. It depends on how badly the brain cells were damaged and which areas were affected by the devastating effects of the disease.
Loss of vision due to stroke is common. In this case, the pathology is often expressed in different ways. There may be loss of vision in both eyes or just one, and sometimes visual hallucinations or oculomotor disorders occur. However, with properly organized treatment, which is prescribed only by a specialist, there is a high probability of restoring visual function partially or even completely.
- Diplopia - double vision occurs, which cannot be focused on one point. Pathology develops due to deviation of the eye axis from the correct position. The patient feels severe dizziness and cannot concentrate when moving the body. Therefore, he walks with his eyes closed until he fully recovers.
- Exophthalmos is a characteristic sign of oculomotor nerve atrophy. One or both eyeballs move forward. As a result, the motor function of the organ is disrupted, the eyelids do not close and the cornea dries out, which aggravates the disease with inflammatory processes. In this case, the upper and lower eyelids are partially or completely stitched together for a certain period of time to prevent serious complications.
- Optic nerve atrophy is the partial or complete destruction of the structure of the nerve fibers that transmit visual stimuli from the retina to the brain. The pathology leads to impaired color rendering, narrowing of visibility, decreased or complete loss of vision. And if a muscle disorder occurs, then drooping eyelids and trembling of the apples occur. The prognosis in most cases is unfavorable, and the patient is assigned a disability group.
Treatment
Therapy and the likely consequences of the pathology largely depend on the degree of damage to the organ, the duration of the disease and how timely premedical care was provided to the person. Early diagnosis of the phenomenon allows us to talk about good treatment effectiveness and complete restoration of visual function. Experts prefer to treat such pathologies using laser correction, a nonspecific technique, or drug therapy.
Non-specific technique
In certain cases, the symptoms and causes of ocular stroke require specific therapeutic treatment. In such circumstances, the patient is prescribed hyperbaric oxygen therapy. During this procedure, the patient is in a hermetic pressure chamber. Treatment is carried out in it using oxygen, which is under pressure.
Drug therapy
Drug therapy for ocular stroke Drug treatment for ocular stroke involves taking medications aimed at eliminating a blood clot, eliminating spasms, normalizing blood circulation and blood pressure. The following may also be prescribed:
- angioprotectors;
- antibiotics (in case of infection);
- agents that prevent the formation of blood clots;
- medications to eliminate concomitant ailments that can aggravate the pathology.
All medications are selected by a specialist, taking into account the characteristics of the patient and the symptoms of the disease.
Operation
At the moment, the use of laser coagulation is the most effective and widespread method of treating pathology. This procedure contributes to the complete destruction and removal of the blood clot, as a result of which blood circulation in the problem area is normalized again. In addition, laser correction is also recommended in cases of retinal detachment or to correct degenerative changes in the fundus of the eyeball.
Damage to visual function after stroke and its recovery
Patients who have suffered a cerebral hemorrhage often experience a complication during the recovery period such as loss of vision.
It can be complete or partial, it all depends on the degree of necrotic changes in brain tissue, the affected area and the volume of dead neurons.
Doctors say that vision loss after a stroke occurs in 30% of patients; during the rehabilitation period, such patients require long-term medication and auxiliary therapy to restore lost functions at least partially.
Symptoms of optic nerve damage due to stroke
As a result of a stroke, which occurs due to blockage of brain capillaries or insufficient oxygen supply to the brain, some neurons die. Atrophy and necrosis of large areas of tissue occurs.
Those areas that are damaged cease to perform the functions for which they were responsible. If the parts responsible for visual function are affected, vision disappears and temporary blindness develops.
If the damage was reversible, the foci of dysfunction are restored over time; with irreversible changes, disastrous consequences arise in the form of complete loss of vision.
Symptoms of visual impairment may indicate which parts of the brain were affected first and the extent of necrotic damage to neurons:
- loss of visual fields - the lesion had a small localization. This type of pathology is called a “blind spot” because a separate area disappears from the field of view. The syndrome is accompanied by pain in the eye sockets. Minor brain damage leads to the fact that vision is restored independently during the rehabilitation period;
- loss of peripheral vision - full visual function is provided by two brain lobes - left and right. Information from the retina of both eyes is processed by the opposite lobe (the left-sided area is responsible for the right side of the retina and vice versa). If peripheral (side) vision is lost, it means that the brain tissue has suffered extensive damage due to hemorrhage. Restoring lateral vision after a stroke is a difficult and lengthy process, requiring intensive medication and auxiliary therapy. Intact brain structures can take over some lost functions;
- paralysis of the nerve responsible for the motor function of the eyes - such an atrophic disorder that occurs in the muscle fibers responsible for the movement of the eyeballs leads to protrusion of the eyes outward. Another consequence is squint.
Successful treatment and reversibility of visual impairment depends on timely diagnosis of stroke and immediate therapeutic assistance.
Optic nerve damage due to stroke
Complete atrophy of the optic nerve during hemorrhage causes blindness. If the nerve is not atrophied, but has undergone extensive damage, this leads to the patient being unable to open his eyes on his own.
The optic nerve is located in close proximity to the main parts of the brain, in particular, in the area of the superior colliculus of the midbrain (in the middle of the large vessels), therefore, with a stroke, vision will be lost in a third of patients.
Damage to the optic nerve leads to the following consequences:
- diplopia – the eyeballs turn in different directions, the patient feels double vision and cannot fully visualize the world around them;
- spasms of the eyelids - while the eyeballs tremble and are in constant tension;
- bulging eyes - the condition is accompanied by dry cornea and constant lacrimation.
In order to prevent serious consequences in the form of complete atrophy of the optic nerve, intensive treatment must be started immediately after a stroke. Patients with severe necrotic changes in brain tissue are prescribed visual disability. If the consequences are reversible, the patient can achieve improvement by carrying out persistent therapy and following all medical recommendations.
Program to restore lost functions
Because the parts of the brain that control visual function are most sensitive to a lack of oxygen, they undergo changes within a minute after the onset of a stroke. This fact explains the complexity of therapy to restore vision after a stroke, not only at home, but also in a hospital during rehabilitation.
There are different approaches to restore visual functions:
- nonspecific treatment;
- drug therapy;
- therapeutic and preventive gymnastics for the eyes;
- surgical method.
The patient can combine all three approaches if the consequences are reversible and do not yet require surgical intervention. Relatives should support the patient, help and create all the conditions for full treatment.
Non-specific technique
Additional and initial measures that a doctor can recommend so that visual functions are restored faster will help speed up the recovery process and make life easier for the patient in the post-stroke period.
They are aimed at regular and simple eye training, which may seem useless, but in fact, constant concentration on objects and moving your gaze around the room helps train the visual analyzer:
- make changes to the floor covering - if it is covered with tiles or laminate, part of it needs to be covered with rugs or paths that are different in texture and color;
- make an original color scheme for the stairs - paint the steps in different shades, so that the patient, while climbing them, will train the retina of the eyes;
- place bright objects in the room - the patient will focus his gaze on them, training his eyes.
A good effect can be achieved by using various drawings with a three-dimensional image, with the help of which the focusing of the eyes alternately changes; such exercises are done to prevent double vision.
Drug therapy
At the moment, there are no special means that would be used during the rehabilitation period to restore visual functions. The action of drugs used after a stroke is aimed at the following results:
- normalize blood flow to the brain;
- restoration of rheological properties of blood;
- elimination of metabolic disorders;
- reducing the volume of necrotic tissue;
- normalizing oxygen delivery to the brain and reducing the sensitivity of cells to its lack.
Using an integrated approach, it is possible to reduce the number of necrotic neurons and help restore those parts that were minimally affected.
To restore blood supply to the brain, drugs against blockage of blood vessels are used. This pathology is represented by the main symptom - the formation of clots inside the capillaries. After they are eliminated, the patient’s focal signs disappear, but such drugs must be used urgently, in the first few hours after the hemorrhage.
To restore the rheological properties of the blood, medications are prescribed to improve microcirculation (Pentoxifylline, Trental) and anticoagulants (Heparin and its derivatives).
To reduce the volume of necrotic tissue, vasoactive drugs are used - Cavinton and Eufillin.
If cells are highly sensitive to hypoxia, it is recommended to take vitamin E, which has antioxidant properties, Cerebrolysin (a hypoxia protector), Piracetam and Noopril.
Operation
Surgical intervention is used for severe visual impairment and cosmetic defects, such as strabismus.
The operation does not eliminate the cause and consequences of the disorders, but returns the eyes to their natural position and reduces the effect of diplopia (double vision).
The patient must give consent to the operation. When choosing a surgical method, the doctor weighs the pros and cons, makes a prognosis of the possible outcome and reveals to the patient the full clinical picture.
Many survivors of a brain catastrophe ask how to restore vision after a stroke - this is a long, labor-intensive process. Not every patient can achieve success on their own.
Only coordinated work between the patient and the doctor, monitoring the condition over time and a combination of different approaches will help minimize the negative consequences of a stroke and return visual function to a state close to the original one.
Source: //insultinform.ru/posledstviya-insulta/vosstanovlenie-zreniya
Perspective
The long-term outlook for people with eye stroke can vary greatly. This depends on the severity of the stroke, the success of treatment, and the arteries or veins affected.
An article in the journal Eye, as mentioned above, found that 80% of people who have a stroke have significant vision loss by 20400 or worse.
In some cases, a person's vision may be restored over time. A study in the American Journal of Ophthalmology found that vision loss may improve for many people, depending on the type of ocular stroke.
https://www.youtube.com/watch?v=p_BQonMqWcQ
The authors state that identifying the type of ocular stroke is an important factor in how well a person can see after it.
Conclusion
Living a healthy lifestyle isn't just good for your heart. It can improve overall health and reduce the risk of problems such as eye stroke and vision loss.
Key symptoms
The initial stages of the process are asymptomatic: there is no pain, the eyes do not water. Minor visual impairment does not bother the patient. The usual pathology develops only on one side, and there is no difference between the vision of the left and right eyes. With development, more clear symptoms of ocular stroke arise:
- Traces of pinpoint hemorrhages form on the surface of the white membrane.
- Vision is impaired: clear contours of figures are lost, double vision occurs.
- The “fly sight” effect appears after a sharp rise of the head.
- Cloudiness of the lens develops, and cataracts are diagnosed.
If an artery is occluded, the patient may go blind without any symptoms.
To stop the process and restore vision, urgent diagnosis and treatment are necessary. First of all, the ophthalmologist determines the type of disease depending on the location of the hemorrhage. With central occlusion, symptoms develop rapidly: the transition of a microstroke to the acute phase occurs in 2-3 days. With vein thrombosis, retinal separation may occur. This type is characterized by complete loss of vision. The most dangerous form is considered to be arterial occlusion. In this case, the patient does not feel anything, but there is a possibility of loss of central vision.
Semiotics of apoplexy
Stroke causes various neurological disorders and problems. The nature and extent of the damage depends primarily on the area of the brain affected by the injury.
Paralysis, numbness
A common symptom of apoplexy is the acute onset of weakness, paralysis or numbness on one side of the body. If the left side of the body is affected, this indicates a stroke in the right hemisphere. If the right side of the body shows symptoms of numbness or paralysis, this indicates damage to the left hemisphere.
Paralysis
If all four limbs are paralyzed (tetraparesis), this is basilar thrombosis - a closure of the basilar artery in the brain stem. This cerebral vessel is the result of the union of two vertebral arteries. Basilar thrombosis is a form of brainstem infarction.
Vision problems
Symptoms of apoplexy often affect the eyes: diplopia, blurred vision and temporary loss of vision in one eye can be symptoms of a stroke if they occur suddenly. Often there is a sudden loss of one or more parts of the visual field. The visual field is the part of the environment that the patient can see without moving the head or eyes. If part of this visual field—for example, the left side—suddenly disappears, it can easily lead to falls or accidents because the sufferer cannot see the vehicle on the left side.
Diplopia – double vision
Speech disorders
Sudden speech disturbances are other possible symptoms of apoplexy and vary depending on the severity of the brain damage. Thus, a moderate stroke can cause symptoms such as choppy and slurred speech. Some patients suddenly twist syllables, use incomprehensible word structures, or begin to cry. In severe cases, a patient with apoplexy cannot speak.
Important! A severe disorder in understanding language should also raise suspicion of a stroke. The patient may suddenly no longer understand what is being said to him.
Dizziness
One possible symptom of a stroke is sudden dizziness with gait disturbances. Some patients perceive this as a turn, so it seems to them that they are spinning, like on a carousel. Others feel vibrations - for them the earth vibrates, as if they are on a ship. In addition, the feeling of "bouncing in the elevator" is a possible sign of a stroke.
Balance problems and loss of coordination may be accompanied by dizziness, especially in women.
Very severe headaches
If very severe headaches suddenly appear, the intensity of which is completely new and unknown to the person, this may also be cerebral apoplexy. Nausea and vomiting are often associated with pain, as are other possible stroke symptoms.
Eye stroke: treatment, consequences and diagnosis
A severe or mild brain stroke is an emergency for the patient. Even with a slight suspicion of apoplexy, everything possible must be done to take the victim to the hospital. The doctor will check your blood pressure and heart rate. If the patient is conscious, the doctor may ask about signs and symptoms (visual disturbances, numbness, or paralysis).
Once admitted to the hospital, the neurologist will become the responsible specialist in the event of a suspected stroke. In a neurological examination, the doctor examines the patient's coordination, speech, vision, spatial orientation and reflexes. If your vision is severely impaired (in the case of an optic nerve stroke), an ophthalmologist may be required.
A computed tomography scan of the head (cranial computed tomography) is also performed immediately. The examination is often complemented by vascular imaging (CT angiography) or blood perfusion (CT perfusion). Images from the cranial nerve can show whether vascular occlusion or cerebral hemorrhage is responsible for the brain stroke. Its location and extent can be determined.
Sometimes magnetic resonance imaging (MRI) is used instead of computed tomography. It can also be combined with vascular imaging or blood flow measurement.
MRI
In some patients, a separate X-ray examination of the blood vessels (angiography) is performed. Vascular imaging is important to identify vascular malformations (aneurysms, cavernomas, etc.) or vascular lesions.
In a special ultrasound examination (duplex sonography) of the vessels supplying the brain, the doctor can identify atherosclerotic deposits on the walls of the artery.
Ultrasound examination of the heart cavities (echocardiography) can reveal hereditary diseases that contribute to the formation of heart valve dysplasia. Sometimes blood clots are found in the cavities of the heart. They can cause another stroke and therefore require treatment with anticoagulants.
Another important cardiac test after a stroke is electrocardiography (ECG), which is the measurement of electrical currents in the heart. Sometimes an ECG is performed over a long period of time (24-hour ECG or long-term). Based on the ECG, the doctor can diagnose cardiac arrhythmia. It is also considered an important risk factor for ischemic stroke.
A blood test is important in diagnosing a stroke. Biomaterial samples are examined for coagulation, glucose levels, electrolytes and renal metabolites.
The above studies serve to confirm suspicions of apoplexy and as tools for a more thorough study of the disease. They also help identify potential complications at an early stage: hypertensive crises, heart attacks, pneumonia caused by food particles (aspiration pneumonia) and kidney failure.
Recovery and treatment
Treatment after a stroke that affects the eyes is aimed at minimizing risk factors. Anticoagulants are prescribed only for ischemic cerebral stroke. For hemorrhagic, surgical treatment is indicated. An important component in the patient’s rehabilitation is lifestyle modification – diet, physical activity and stress.
Advice! Restoring vision after a stroke that affects the eyes can be quite difficult. If a small-focal (micro) stroke occurs, then it is possible to restore vision by following the doctor’s treatment recommendations. It is worth noting that cold laser for vision restoration is usually an ineffective and costly measure.
Methods of rehabilitation of patients with visual impairment after stroke
The clinical picture of a stroke depends on which area of the brain the lesion is located in.
Visual impairment is not the most common symptom among those observed in post-stroke patients, but it is very difficult to rehabilitate. Restoring vision after a stroke is a complex and lengthy process.
It begins from the first minutes of treatment of the underlying disease, and if properly organized can give very good results.
Often after a stroke, patients may experience vision problems
Types of visual impairment after stroke
All types of visual impairment in post-stroke patients can be divided into the following types:
- blurred vision in one or both eyes;
- loss of vision;
- visual hallucinations;
- oculomotor disorders.
Strabismus as a result of a stroke
Visual disturbance may be transient or permanent. The first type is more common in the case of transient ischemic attack. Loss of vision can be complete or partial. The latter is characterized by loss of certain fields of vision or one-sided blindness.
Oculomotor disorders occur when the nuclei of the oculomotor nerves are damaged. The first place in the clinical picture is squint and complaints of double vision.
Methods of vision restoration
The visual departments are very sensitive to lack of oxygen. Their defeat can be observed within one minute after the onset of hypoxia. This explains the difficulties that patients and doctors face during the treatment process.
The best results can only be achieved by following all medical recommendations as accurately as possible.
Today, when vision deteriorates, three complementary treatment areas are used:
- non-specific activities;
- drug treatment;
- gymnastics;
- surgical intervention.
Non-specific events
There are various rehabilitation measures that can help restore impaired vision after a stroke.
These measures are aimed at significantly making the patient’s life easier and speeding up his recovery.
At first glance, it may seem that they have nothing to do with restoring the normal functioning of the visual analyzer, but in fact this is not the case.
Essentially, these simple steps force the patient to pay attention to the objects around him, constantly moving his gaze from object to object, which is a good addition to therapeutic exercises. So:
- Use a variety of flooring materials. If the floor is covered, for example, with tiles in key areas of the home, lay small paths or rugs. They should differ significantly not only in texture, but also in color.
- Make the stairs more convenient for movement. This means not only the installation of railings, but also the color scheme - contrasting steps that alternate will be very useful.
- If possible, place bright accents - attracting the patient’s attention, they will not only help him orient himself, but will also play the role of a kind of eye simulator.
Drug treatment
Specific agents whose action is aimed at improving vision in patients after a stroke have not been developed to date. To help the patient recover faster, doctors use medications that serve the following purposes:
- restoration of blood flow in the brain area;
- normalization of rheological properties of blood;
- correction of metabolic disorders of the brain;
- reduction of the necrosis zone;
- decreased sensitivity of neurons to lack of oxygen.
Drug treatment of stroke consequences
This approach will help minimize the number of dead nerve cells, and those located in the ischemic penumbra zone will be able to fully recover.
Resuming blood flow in the affected area is the most effective method.
For this purpose, drugs are used that can dissolve blood clots formed in the vessels, after which the patient completely disappears all focal symptoms. A significant drawback of the method is its time limitation; it can only be used during the first three hours after a stroke.
Normalization of the rheological properties of blood is achieved by prescribing drugs that improve cerebral microcirculation and anticoagulants. From the first subgroup, pentoxifylline, trental, sermion are most often prescribed, from the second - heparin and its low molecular weight fractions.
The use of vasoactive drugs can reduce the area of necrosis - they improve blood flow in the ischemic penumbra zone and help neurons recover. The most popular of this group are Cavinton and aminophylline.
The sensitivity of brain tissue to hypoxia can be reduced with the help of antioxidants - vitamin E, and hypoxia protectors - Cerebrolysin, piracetam or nootropil.
Gymnastics
This is a very simple and affordable method of rehabilitation of patients after a stroke. It can easily be used at home. The only thing that is required from the patient is patience and careful implementation of the recommendations.
- Light pressure with the fingers of both hands on the upper, lateral, and then lower edge of the eye sockets.
- Slow and gentle pressure on the eyeballs.
- Massage of the bridge of the nose.
- Intense blinking of the eyes.
- Movement of the eyes in horizontal and vertical directions.
- Examination of an object located at different distances from the patient’s eyes.
Computer methods for restoring vision in patients after a stroke are of great interest.
Their task is to train brain neurons located in the vicinity of the affected ones. The program forces them to do the work that dead cells used to do. Despite its effectiveness, it is not widely used. However, there are clinics that actively use the technique in their vision restoration programs.
Surgery
Considering the pathogenesis of visual impairment, surgical intervention on the eye muscles will not eliminate the existing problem. However, surgery can return the eye to its normal position and reduce the phenomenon of diplopia, that is, double vision.
In some cases, the question arises about performing a surgical operation.
Before consenting to such treatment, the patient must weigh all the nuances. As a rule, the final decision is made jointly by the patient, the neurologist and the ophthalmologist.
Finally
Restoring vision after a stroke is quite difficult. Not every patient can achieve success, even if they diligently follow all medical recommendations. However, over time, his condition can improve significantly, since the loss of visual function is compensated by the increased work of other sensory analyzers.
In addition, several months after the stroke, the patient develops new habits. For example, when the lateral field of vision is lost, a person, without noticing it, begins to look to the side with central vision, as a result of which it seems to him that his peripheral vision has been restored.
The defect can be identified during an instrumental examination of the patient.
Source: //GolovaLab.ru/insulto/reabilitatsiya/vosstanovlenie-zreniya-posle-insulta.html