Cutaneous staphylococcus (Staphylococcus epidermidis) is a potentially fatal bacterium that is commonly found on the skin, oral mucosa, and genitourinary tract. Who is at risk of contracting cutaneous staphylococcus? What diseases does cutaneous staphylococcus cause? How to treat Staphylococcus epidermidis infection?
E. coli and methicillin-resistant Staphylococcus aureus (MRSA bacteria) are dangerous and very fast-spreading bacteria. Staphylococcus aureus infection can cause diseases such as pneumonia, myocarditis, phlebitis and meningitis. In turn, the bacterium Escherichia coli (Escherichia coli), the cause of urinary tract infections, urethritis, and cystitis. The consequences of E.coli infection largely depend on the strain of bacteria.
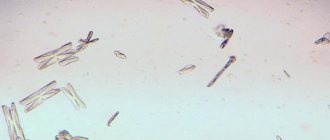
Escherichia coli bacterium
Meanwhile, it turns out that Staphylococcus epidermidis, that is, cutaneous staphylococcus, is a much more dangerous bacterium. This bacterium becomes increasingly resistant to antibiotics and causes life-threatening infections after surgery.
What is cutaneous staphylococcus?
The content of the article
Staphylococcus epidermidis, a close relative of MRSA bacteria. It is so common that it is found on almost every person's skin. Cutaneous staphylococcus is part of the natural bacterial flora and is not dangerous when you are healthy - it is a deadly microorganism that is found throughout the world and remains dormant in most cases.
This type of staph is often ignored in clinical trials, and due to its ubiquity, it can evolve and genetically mutate between bacteria very quickly.
The problem with cutaneous staphylococcus occurs when immunity is reduced - then infection with Staphylococcus epidermidis can cause a number of complications and become a risk factor for many diseases. Cutaneous staphylococcus is especially dangerous for people who have undergone invasive procedures.
Staphylococcal diseases in young people and children
Pustular skin diseases are called pyodermatitis, which, depending on the cause of occurrence, are divided into strepto and staphyloderma. Their mixed form is often observed - streptostaphyloderma.
Streptoderma most often affects children and young men and is usually localized around natural openings - the nose, mouth, ears, that is, in areas subject to irritation by the discharge of these cavities (saliva, mucus). These lesions are very contagious and quickly spread to healthy areas of the skin. Streptoderma is transmitted through toys, diapers, clothes, and underwear.
A fairly common streptococcal skin lesion in newborns is impetigo (from the Latin “impetus” - sudden, attacking). With this disease, flat cavities with a flabby folded covering are formed, filled with serous-purulent contents - phlyctenas.
Merging, they form continuous foci with tortuous inflammatory outlines. Exposed parts of the body are predominantly affected, especially the skin of the face. Nearby lymph nodes often swell, and as the infection spreads, phenomena of general intoxication are observed.
Another form of purulent lesions is neonatal pemphigus. This type of pyoderma is characterized by the formation of large blisters that reach the pigeon egg and are filled with purulent contents. When they rupture, a bare bright red surface (erosion) is formed, which is easily subject to additional infection, resulting in a sharp deterioration in the child’s condition.
Streptococcal pemphigus is extremely contagious, contagious and, in the absence of proper preventive measures, can cause massive outbreaks of pyoderma in maternity hospitals and children's hospitals.
When a child moves home from the maternity hospital, a vesiculopustular form of pyoderma often occurs in places that are most often irritated by sweat (on the back of the head, neck, forehead, groin). Small bubbles with transparent contents (vesicles) the size of a pinhead appear. Then the contents of the vesicles become purulent (pustule) and are surrounded by a halo of hyperemia.
After two to three days, the pustules burst or undergo reverse development and superficial crusts form in their place. Despite the relative ease of this infection, its complications can be very insidious. They are expressed in widespread and severe phlegmon, occurring with significant swelling and subsequent necrosis (melting) of the subcutaneous tissue.
In infants with low nutrition, in improperly bottle-fed children, as well as in older children with weak protective reactions (due to tuberculosis or other types of intoxication), streptococcal infection is not limited to superficial skin lesions, but invades deeper tissues, forming deep ulcers - ecthyma .
They occur on the most frequently injured parts of the body (lower back, lower legs) and are characterized by a sluggish, long-lasting course. After they are healed, scars remain.
Speaking about streptococcal pyoderma in children, we cannot ignore erysipelas, which especially often affects the face (hence the name “erysipelas”). The skin of the face becomes red and swollen. The disease is accompanied by an increase in temperature and sometimes a severe general condition requiring emergency treatment measures.
The so-called “zaeda” is also known - streptococcal phlyctena (a type of impetigo) in the corners of the mouth, which opens and forms a long-term non-healing wound, constantly renewed in connection with facial movements of the facial muscles and food intake. With insufficient sanitary control, seizures can cause real outbreaks in children's groups.
Pemphigus of newborns can also be caused by staphylococci. In the most severe form of this disease, serous fluid accumulates in large areas under the stratum corneum of the skin and detachment of the skin occurs to such an extent that the child gives the impression of being “scalded.”
With staphyloderma, hair follicles are often affected, for example on the head, which leads to a small pustular rash, which disappears without a trace after treatment.
Staphylococci cause not only local, limited skin lesions, but also sore throat, severe pneumonia, inflammatory foci in various organs and tissues (liver, spleen, kidneys), resulting from the spread of microbes through the blood and lymphatic tracts. A generalized staphyloccal infection - sepsis - poses a mortal threat.
Staphylococci can cause real epidemic outbreaks in maternity hospitals and children's hospitals. Due to them, the vast majority of skin and septic lesions in newborns and purulent diseases in mothers occur. Postpartum sepsis, mastitis, pneumonia, meningitis, inflammation of the birth canal, conjunctivitis are a real disaster. Of course, they are especially dangerous for women in labor and newborns.
Cutaneous staphylococcus - symptoms
Symptoms of activation of staphylococcal infection:
- skin changes;
- boils and skin rashes;
- pain at the site of a staph infection;
- ulcer formation.
Staph Infection
Symptoms of cutaneous staph are nonspecific—each case of cutaneous staph may have slightly different symptoms depending on what part of the body is affected. People undergoing surgery should pay attention to the symptoms of cutaneous staphylococcus.
Cutaneous staphylococcus in a child
A child's immune system is more sensitive than an adult's, so cutaneous staphylococcus can be dangerous even for the youngest. If a child has skin lesions, he should be carefully treated, dressed and protected from external factors to avoid infection. If your child has skin changes for no reason, consult a doctor.
Staphylococci in a child can cause folliculitis, staphylococcal sycosis, and multiple abscesses. Conditions such as bullous impetigo, bullous inflammation and peeling skin can occur as a result of staph infection in newborns.
Why is staphylococcal infection dangerous?
Staphylococcus is especially dangerous in association with viruses and fungi, as well as with concomitant childhood droplet infections that reduce the overall reactivity of the body. It is not without reason that in many diseases local or general complications caused by staphylococci are observed.
Thus, during influenza epidemics, staphylococcal pneumonia is not uncommon, which most often turns out to be the cause of a child’s long-term illness and is the most common prerequisite for death.
Staphylococcal and streptococcal toxins have pronounced sensitizing properties, causing allergies and toxic damage to the heart muscle, kidneys and other important organs. Unlike a number of pathogens of childhood infections, the site of action of which is limited to certain areas of body tissue, staphylococcus and streptococcus are “omnivorous”.
They can cause inflammation of the gallbladder (cholecystitis), toxic dyspepsia and gastroenteritis, inflammation of the joints (arthritis), and genitourinary tract (urethritis and endometritis). In newborns, staphylococcal and other purulent inflammatory phenomena begin with the umbilical wound or other skin lesions that are invisible at first glance (scratches, abrasions).
It must be emphasized that up to 90% of cases of sepsis in young children are associated with staphylococcus.
Cutaneous staphylococcus - treatment
Scientists from the Milner Center for Evolution at the University of Bath have identified 61 genes in staphylococcal skin bacteria that can cause deadly diseases. The samples were taken from patients who had infections following hip or knee replacement surgery and fracture fixation, and were compared with skin swab samples from healthy volunteers.
Surprisingly, even more deadly forms of the bacteria were found in some of the healthy people who took part in the study. Staphylococcus epidermidis has also been found to form biofilms, which increase the body's resistance to antibiotics.
Treatment of cutaneous staphylococcus involves the use of antibiotics. Unfortunately, some antibiotics do not work against some types of cutaneous staphylococcus - the drug resistance of cutaneous staphylococcus is similar to that of Staphylococcus aureus.
For highly drug-resistant strains, vancomycin or teicoplanin are used, which are effective against staphylococci, including methicillin-resistant strains.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Patient preparation rules
U/g fence
.
Standard conditions:
During the working day of ML "DILA".
Important
: • During the day before collecting the material, do not use topical medications. • Refrain from urinating for 2 hours.
• For 3 days, abstain from sexual intercourse and drinking alcohol. • Take it before or not earlier than 14 days after the end of the course of antibacterial, antimycotic therapy (unless otherwise determined by the attending physician). Another BM
(BM from a wound, from an ear, the contents of a nail pocket, from an eye).
Standard conditions
: During the working day of ML "DILA".
The material is accepted at any branch of ML "DILA". Important:
• Do not use topical medications for 24 hours before collecting material.
• Take before or no earlier than 14 days after the end of the course of antibacterial, antimycotic therapy (unless otherwise determined by the attending physician). • Paired cultures are taken with different swabs (ears, eyes) and are registered as 2 cultures. Attention
: it is possible to deliver the biomaterial to the laboratory within 48 hours at a temperature of +20-25°C in a special transport tube (swab with transport medium).
Feces: collected after spontaneous bowel movements in a sterile container in an amount of at least 5 grams (half a teaspoon). Deliver the material after collection within: 2 hours - ML "DILA" No. 1 (6A Podvysotskogo St.) Mon-Sat, 30-40 minutes - other ML "DILA" in Kiev - Mon-Fri Material from the tonsils .
Standard conditions: BM is taken on an empty stomach or 2 hours after a meal.
Important
: • During the day before collecting the material, do not use drugs of local significance. • Donate before or no earlier than 14 days after the end of the course of antibacterial, antimycotic therapy (unless otherwise determined by the attending physician). Material from the tongue.
Standard conditions: BM collection is performed on an empty stomach, do not brush your teeth!!! Important: • During the day before collecting the material, do not use drugs of local significance. • Donate before or not earlier than 14 days after the end of the course of antibacterial, antimycotic therapy (unless otherwise determined by the attending physician). Mother's milk
.
Standard conditions: The material is handed over to the first department of ML "DILA" LLC "ML "Dila" at the address: st. Podvysotsky, 6A. During the working day ML "DILA". Important:
A separate sterile container is used for material from each breast.
Morning sputum
.
Standard conditions: During the working day of ML "DILA". The material is delivered to the first branch of ML "DILA" LLC "ML "Dila" at the address: st. Podvysotsky, 6A. for 2 hours at room temperature, at +4+8°C for up to 6 hours. BM is delivered in a sterile plastic container with a screw cap. Important
: Sputum collection is carried out in the morning on an empty stomach.
Before coughing, the client brushes his teeth and rinses his mouth with boiled water. It is advisable to examine the biomaterial from the first morning portion. Take before or no earlier than 14 days after the end of the course of antibacterial, antimycotic therapy (unless otherwise determined by the attending physician). Washing from the bronchi during bronchoscopy
.
Standard conditions: During the working day of ML "DILA". The material is delivered to the first branch of ML "DILA" LLC "ML "Dila" at the address: st. Podvysotsky, 6A. for 2 hours at room temperature, at +4+8°C for up to 6 hours. BM is delivered in a sterile plastic container with a screw cap. Important:
Take before or not earlier than 14 days after the end of the course of antibacterial, antimycotic therapy (unless otherwise determined by the attending physician).
Attention: The material is collected by the doctor during bronchoscopy. Bile
.
Standard conditions
: During the working day of ML "DILA".
The material is accepted in the first department of ML "DILA" LLC "ML "Dila" at the address: st. Podvysotsky, 6A. within 2 hours after collecting the material at a temperature of +20-25° C. Important:
Each portion
You can add this study to your cart on this page