Description
Divine squint.
This is an oculomotor disorder in which the eyeball deviates outward. Clinical signs of pathology include constant or periodic displacement of the eye, complaints of diplopia, and impaired binocular vision. To make a diagnosis, visometry, autorefractometry, closure-opening test, synoptophore study, and Worth test are performed. Conservative therapy is limited to the correction of refractive errors, pleoptic and orthoptic treatment. If there is no corresponding effect, an operation is performed - external recession and resection of the internal rectus muscle.
Exotropia
Causes
The etiology of strabismus is not fully understood. A genetic predisposition has been noted, while patients inherit many factors (myopia, farsightedness) that contribute to the development of the disease. The negative impact of teratogenic factors (intrauterine infections, ionizing radiation, occupational risks) on the position of the eyeballs has been confirmed. The main causes of divergent strabismus are taken into account: Exotrophy is observed in children with refractive errors, among which hypermetropia and high myopia are more common. The most significant risk factor is unilateral axial hyperopia of moderate or severe severity. • Trauma.
Reduced mobility of the eyeball is observed with injuries affecting the extraocular muscles, bony walls of the orbit, or nerves.
Post-traumatic strabismus requires early surgical treatment. • Neurological diseases.
Difficulty in converging-divergent movements occurs in response to damage to the occipital lobes of the brain, the lateral geniculate body and the superior colliculus of the quadruple.
The angle of strabismus is controversial. There is a correlation with the level of intracranial pressure. • Fogging of the optical media of the eye.
Diseases of divergent strabismus can be caused by diseases such as corneal cornea, cataracts, and vitreous fibrosis. The worst vision deviates from the temple. The sensory form of strabismus occurs when visual acuity decreases below 0.1 diopters.
Convergent strabismus code according to ICD 10 in children
ICD-10 category: H50.0
ICD-10 / H00-H59 CLASS VII Diseases of the eye and its adnexa / H49-H52 Diseases of the muscles of the eye, disorders of concomitant eye movement, accommodation and refraction / H50 Other forms of strabismus
Definition and general information[edit]
Strabismus (strabismus, heterotropia) is a deviation of the visual line of one of the eyes from the common point of fixation, accompanied by impaired binocular vision.
Classification
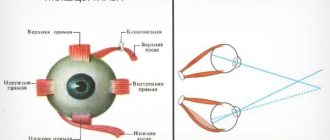
• Based on the direction of deviation of the squinting eye, they are distinguished: convergent strabismus (esotropia) - deviation of the eye towards the nose, divergent (exotropia) - deviation of the eye towards the temple, vertical - deviation of one eye up or down (hyper- and hypotropia). With torsional displacements of the eye (deviation of the upper end of the vertical meridian of the cornea towards the temple or nose) they speak of cyclotropia (ex- and incyclotropia).
• According to the involvement of the eye, strabismus can be unilateral, i.e. monolateral (constantly squints one eye), and alternating (alternately squints one eye or the other).
• According to the degree of participation of accommodation in the occurrence of strabismus, they are distinguished: accommodative, partially accommodative and non-accommodative strabismus.
• According to the stability of the deviation (deviation of the eye), strabismus can be constant, unstable, periodic
Etiology and pathogenesis[edit]
Concomitant strabismus is a pathology primarily in early childhood, since the binocular visual system is not yet stable enough and is easily destroyed under the influence of unfavorable factors in the external and internal environment of the body. The cause of concomitant strabismus can be congenital or acquired diseases of the central nervous system, as well as ametropia, a sharp decrease or loss of vision in one eye (even in adults).
Pathogenesis
As a result of damage to various parts of the visual analyzer, its normal sensorimotor connections are disrupted, which leads to a disorder of the bifixation reflex and binocular vision or prevents their formation. When vision is poor or one eye is blind, strabismus develops due to a lack of stimulus for fusion (merging images), which causes the eye to deviate.
Clinical manifestations[edit]
Signs of concomitant strabismus:
• equal magnitude of the squint angle in different directions of gaze;
• full range of movements of the eyeballs;
• equality of the primary (when fixing with a non-squinting eye) and secondary (when fixing with a squinting eye) strabismus angles;
• absence of diplopia (double vision).
Amblyopia
is a functional decrease in vision.
Amblyopia is classified according to the degree of visual acuity reduction:
• low degree - with visual acuity of the squinting eye 0.4-0.8;
• moderate degree - with visual acuity 0.2-0.3;
• high degree - with visual acuity 0.05-0.1;
• very high degree - with visual acuity below 0.05.
Visual fixation
- this is a relatively motionless gaze on the object in question.
Types of Amblyopia
: disbinocular (occurs as a result of impaired binocular vision), refractive (in the presence of refractive errors - ametropia and untimely or inconsistent correction), anisometropic (in the presence of uncorrected anisometropia - differences in refraction between the right and left eyes), obscuration (with clouding of the ocular media) .
Convergent concomitant strabismus: Diagnosis[edit]
Anamnesis
When collecting anamnesis, it is necessary to consider:
• time of occurrence of strabismus and the duration of its existence (at what age did it appear, suddenly or gradually);
• whether there is diplopia, whether there was diplopia at the beginning of the development of strabismus;
• what can the occurrence of strabismus be associated with (general diseases, mental trauma, eye diseases, pathology of pregnancy and childbirth in the mother);
• is strabismus constant or periodic;
• at what age does the patient wear glasses constantly or periodically;
• previous treatment (surgical, functional);
• general health of the patient.
Physical examination
• Visual acuity with and without correction.
• Refractometry.
• Degree of deviation according to Hirschberg.
• Study of the magnitude of the squint angle and eye mobility in gaze positions: to the right, left, up and in diagonal positions.
Instrumental studies
1. Synoptophore
Research on synoptophore: objective angle, subjective angle, positive fusion reserves, negative fusion reserves, vertical fusion reserves, cycloreserves.
The synoptophore is one of the main haploscopic instruments. The separation of the visual fields of the right and left eyes is carried out mechanically in this device, using two separate movable optical tubes for each eye, in each of which paired test objects are presented to the subject for combination and fusion.
There are three pairs of test objects: for combining, merging and stereoscopy, which can move (horizontally, vertically, torsionally, i.e. when tilted to the sides).
2. Study of visual fixation
Fixation is checked using a large non-reflex ophthalmoscope or monobinoscope, determining which part of the patient’s fundus the shadow of the fixation needle falls on. Normally, fixation is foveal, or central, i.e. the image is recorded precisely by the central fovea of the retina. Non-central fixation can be parafoveal (the image is fixed close to the fovea), macular (closer to the periphery of the macula), paramacular (outside the macula), peripheral (peridiscal - in the optic disc).
Pathogenesis
The mechanism of development of divergent strabismus is based on a violation of the supply of nerve impulses to the visual cortex of the brain. Damage can be located at the level of the receptor apparatus, pathways, cortical and subcortical centers. The separation process becomes impossible. As a result, the patient is unable to simultaneously look at an object with both eyes and focus on it. On the outside, both eyes are slanted or one with less vision. With the intermittent type of the disease, there is a sequential deviation of the left and right eyeballs.
Classification
There are congenital (infantile) and acquired forms of divergent strabismus. Based on the deviation scores, it is customary to classify primary exorropia as kurtosis discrepancy (deviation at a distance is 7° greater than near), basic exotropic (deviation at a stable level), convergence insufficiency (deviation at a distance 7° less than near), and pseudo-exorropia. discrepancy discrepancy. The main clinical forms of divergent strabismus: • Persistent exotropia.
Early onset is typical.
The first signs of the disease are usually detected at birth. The deflection angle is stable. One eye is involved in the pathological process. • Intermittent exothermic reaction.
The first symptoms appear before the age of 5 years.
The development of pathology is preceded by exophoria, which, in the absence of timely treatment, replaces tropia. • Secondary exotropics.
Detected in patients with monocular vision.
As a rule, this is a consequence of the opacity of the optical center of the eyeball. This can happen at any age. An eye with a weak field of vision deviates outward. • Persistent exotropia.
Forms spontaneously in the amblyopic eye. A prerequisite may be surgical treatment of esotropia in the past. The Hirschberg strabismus angle subjected to surgical techniques does not exceed 5-7 degrees.
Accommodative convergent strabismus
Accommodation and convergence are two essential elements of the act of vision at close range. At the same time, accommodation is the process of focusing the eye on a nearby object with a change in the curvature of the lenses. To achieve bifoveal fixation of an object, the eyes converge simultaneously. Both the process of accommodation and the process of convergence are related quantitatively to the distance to the visible object with a very constant ratio relative to each other. Therefore, the cause of some types of strabismus is a change in the AK/A index.
Refractive accommodative convergent strabismus
With it, the AK/A index does not change, and strabismus occurs in response to severe hypermetropia, ranging from +4.0D. The accommodation tension required in this case for focusing even distant objects occurs with an increase in convergence, which is much higher than the negative reserves of fusion. At the same time, a loss of control occurs and convergent strabismus occurs, often in manifest form. It appears between the ages of 6 months and 7 years. When fixing the gaze on near and far objects, the difference in the squint angle is small and is less than 10 D.
In the process of optical correction of existing farsightedness, such strabismus is completely eliminated. In the case of partial convergent strabismus, optical correction of hypermetropia can reduce it, but will not completely eliminate it.
Non-refractive accommodative convergent strabismus
It is explained by a high AC/L index in the absence of serious hypermetropia, which is why increased accommodation occurs with a disproportionately large increase in convergence. There are 2 types of non-refractive accommodative convergent strabismus:
Kurtosis of convergence. In this case, a high AC/A index is noted due to an increase in AC (i.e., normal accommodation with increased convergence).
- Norm of the nearest point of accommodation.
- When fixating an object at a far distance, the eye position is normal; convergent strabismus occurs when fixing an object at a close distance.
With impaired accommodation. Low accommodation is explained by a high AK/A index, which occurs with a decrease in A, since the weakening of accommodation requires serious efforts, which arise with increased convergence.
Removing the nearest point of accommodation. Additional accommodative effort is required when fixating a close object, which leads to convergence excess.
Mixed accommodative convergent strabismus
It is characterized by a combination of hypermetropia with a high AC/A index, when when fixing an object at a far distance, the angle of deviation significantly increases (over 10 D) to fix an object at a close distance. When fixating a distant object, deviation is usually corrected with glasses. If there is no correction with bifocal glasses, convergent strabismus will persist even when fixing an object at a close distance.
Symptoms
Persistent esotropia is characterized by a stable outward deviation of one eye. The squint angle is wide and constant, there are no refractive errors. Visual acuity on the affected side is usually sharply reduced. Dissociated vertical deviation is often observed. This form of divergent strabismus is often combined with neurological disorders. Clinical symptoms of intermittent esotropia are most pronounced against the background of visual overload, general weakness or stress. Parents often notice signs of strabismus in the afternoon. Symptoms of the outcome are most obvious when viewing the patient from a distance. It should be noted that the intermittent form of divergent strabismus is often replaced by a permanent one. Patients with divergent strabismus experience asthenopic complaints. Worrying about increased fatigue against the background of visual tension, burning in the eyes, pain, pain, the appearance of a veil in the eyes. Attempting to merge the images of the right and left eyes results in double vision. Friendly movements become difficult, keeping your eyes in the correct position requires considerable effort.
Variable convergent strabismus code according to ICD 10 Tdfarm
Esotropia (alternating) (monocular), except intermittent
Exotropia (alternating) (monocular), except intermittent
Intermittent:
- esotropia (alternating) (monocular)
- exotropia (alternating) (monocular)
Concomitant strabismus NOS
Brown's capsule syndrome
Strabismus due to adhesions
Traumatic limitation of the elasticity of the eye muscle
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997. No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Sources used: mkb-10.com
SEE ALSO: Kaluga strabismus Recovery after strabismus Conjunctivitis by folk Nagiyev strabismus
Convergent concomitant strabismus
Esotropia (alternating) (monocular), except intermittent
Divergent concomitant strabismus
Exotropia (alternating) (monocular), except intermittent
Intermittent heterotropia
Intermittent:
- esotropia (alternating) (monocular)
- exotropia (alternating) (monocular)
Other and unspecified heterotropies
Concomitant strabismus NOS
Mechanical strabismus
Brown's capsule syndrome
Strabismus due to adhesions
Traumatic limitation of the elasticity of the eye muscle
ICD-10 disease classes
hide all | reveal everything
International statistical classification of diseases and related health problems. 10th revision.
With changes and additions published by WHO in 1996-2018.
Sources used: xn—10-9cd8bl.com
YOU MAY BE INTERESTED in: Displacement of the cervical vertebra, strabismus The best doctors for the treatment of strabismus Can torticollis cause strabismus Weak eye muscles or strabismus Encyclopedia of strabismus Convergent concomitant alternating strabismus
What codes does strabismus have according to ICD-10?
In the modern world, such a problem as strabismus is often encountered; ICD-10 has a special code designating this pathology.
In medicine, the abbreviation ICD-10 stands for International Classification of Diseases. This document is revised once every decade. Now the normative document of the 10th review (ICD-10) is in force.
In the modern world, such a problem as strabismus is often encountered; ICD-10 has a special code designating this pathology.
In medicine, the abbreviation ICD-10 stands for International Classification of Diseases. This document is revised once every decade. Now the normative document of the 10th review (ICD-10) is in force.
Classifier of eye diseases
Ophthalmological diseases and diseases of the adnexa belong to class 7. Each pathology has its own code.
Strabismus is characterized by codes located in the range from H49 to H52, and they are called “Diseases of the muscles of the eye, disorders of concomitant eye movement, accommodation and refraction.”
It is necessary to consider in more detail the types of violations and the corresponding digital designations in the classifier.
Types of pathology according to the international classification of the disease
H49 refers to the designation of paralytic strabismus. Each type also has its own codes and ranges from 49 to 49.9. This disease is associated with deviation of the eye from general fixation at one point. This occurs as a result of damage, paralysis or paresis of the extraocular muscle. The qualifying list includes the following diseases:
- paralytic condition 3 (49), 4 nerves (49.1), 6 abducens (49.2);
- complete ophthalmoplegia (49.3);
- progressive ophthalmoplegia (49.4);
- other species (49.8);
- unspecified type of optic nerve palsy (49.9).
H50 refers to other types of strabismus:
- joint convergent (50) occurs against the background of binocular vision disorder, is congenital or acquired;
- divergent, joint (50.1) often develops in utero and has differences in visual acuity in each eye;
- vertical (H50.2) is characterized by deviations of the eyes either up or down when looking to the side;
- with intermittent heterotropia (H50.3), the non-parallel arrangement of the corneas is clearly expressed;
- unspecified forms of heterotropy have code H50.4;
- heterophoria (H50.5), in which the direction of gaze is not coordinated by the eyes;
- the form of mechanical strabismus has code H50.6;
- H50.8 - other types of disease.
Impairment of joint eye movement (H51):
- with gaze paralysis (51), there is a neurological impairment of the movement of both eyes in the same direction (can develop horizontally or vertically);
- Convergence disorder (51.1) is associated with a neuromuscular abnormality that is characterized by convergence of the eyes;
- H51.2 refers to intranuclear ophthalmoplegia;
- the remaining known joint eye movement disorders are coded 51.8;
- uncertain diagnoses of joint eye movement lesions - 51.9;
Damage to refraction and accommodation - from 52 to 52.7:
- hyperopia (H52), or farsightedness, is a type of vision impairment in which images of distant objects are focused behind the retina;
- myopia (H52.1), or myopia, is considered a refractive error, images are focused from the front.
- astigmatism (H52.2) is an abnormal violation of the shape of the lens, cornea, as a result, a person’s eyes perceive images in a cloudy form;
- aniseikonia (H52.3) - abnormal development of the eyes, in which the perception of the size of objects has a significant difference in individual meridians;
- presbyopia (point 4) is a refractive error in which it is impossible to clearly see small letters or objects when viewed closely;
- disorders associated with eye accommodation (point 5);
- Items 6 and 7 are assigned to the remaining refractive errors and unspecified defects, respectively.
The task of the International Classification of Diseases is to systematize and analyze diseases in different countries.
Sources used: saymigren.net
Diagnostics
The examination of a patient with strabismus begins with a detailed medical history. The ophthalmologist uses a physical examination to draw attention to the movement of the eyeballs. The position of the eyes is assessed by fixing vision at near and far distances with and without the corrective lenses included in the kit. Mandatory studies include the following procedures: With constant exotropia, vision on the affected side is reduced. With the intermittent form, visual function can be maintained at a high level for a long time. The examination is carried out without correction and with glasses. • Autorefractometry.
Divergent strabismus is often combined with refractive errors.
According to statistics, hypermetropia predominates in patients, and myopia is very rare. The study is carried out for cycloplegia. • Coverage test.
With alternating overlap, eye movements are visualized from outside to inside.
Test results may vary depending on how far the patient's vision is set. When properly corrected, the range of motion in glasses is usually less. • Four-point Worth test.
The study allows us to determine the nature of vision.
With a small angle of strabismus, vision is binocular or simultaneous. A constant and large angle is associated with the monocular nature of vision. • Survey in the synoptoforum.
This allows you to accurately determine the angle of deviation with and without eyepiece correction. In the case of continuous exotrophy, the ability to bipolar connection is lost.
Operated convergent strabismus code according to ICD 10
ICD-10 category: H50.0
ICD-10 / H00-H59 CLASS VII Diseases of the eye and its adnexa / H49-H52 Diseases of the muscles of the eye, disorders of concomitant eye movement, accommodation and refraction / H50 Other forms of strabismus
Definition and general information[edit]
Strabismus (strabismus, heterotropia) is a deviation of the visual line of one of the eyes from the common point of fixation, accompanied by impaired binocular vision.
Classification
• Based on the direction of deviation of the squinting eye, they are distinguished: convergent strabismus (esotropia) - deviation of the eye towards the nose, divergent (exotropia) - deviation of the eye towards the temple, vertical - deviation of one eye up or down (hyper- and hypotropia). With torsional displacements of the eye (deviation of the upper end of the vertical meridian of the cornea towards the temple or nose) they speak of cyclotropia (ex- and incyclotropia).
• According to the involvement of the eye, strabismus can be unilateral, i.e. monolateral (constantly squints one eye), and alternating (alternately squints one eye or the other).
• According to the degree of participation of accommodation in the occurrence of strabismus, they are distinguished: accommodative, partially accommodative and non-accommodative strabismus.
• According to the stability of the deviation (deviation of the eye), strabismus can be constant, unstable, periodic
Etiology and pathogenesis[edit]
Concomitant strabismus is a pathology primarily in early childhood, since the binocular visual system is not yet stable enough and is easily destroyed under the influence of unfavorable factors in the external and internal environment of the body. The cause of concomitant strabismus can be congenital or acquired diseases of the central nervous system, as well as ametropia, a sharp decrease or loss of vision in one eye (even in adults).
Pathogenesis
As a result of damage to various parts of the visual analyzer, its normal sensorimotor connections are disrupted, which leads to a disorder of the bifixation reflex and binocular vision or prevents their formation. When vision is poor or one eye is blind, strabismus develops due to a lack of stimulus for fusion (merging images), which causes the eye to deviate.
Clinical manifestations[edit]
Signs of concomitant strabismus:
• equal magnitude of the squint angle in different directions of gaze;
• full range of movements of the eyeballs;
• equality of the primary (when fixing with a non-squinting eye) and secondary (when fixing with a squinting eye) strabismus angles;
• absence of diplopia (double vision).
Amblyopia
is a functional decrease in vision.
Amblyopia is classified according to the degree of visual acuity reduction:
• low degree - with visual acuity of the squinting eye 0.4-0.8;
• moderate degree - with visual acuity 0.2-0.3;
• high degree - with visual acuity 0.05-0.1;
• very high degree - with visual acuity below 0.05.
Visual fixation
- this is a relatively motionless gaze on the object in question.
Types of Amblyopia
: disbinocular (occurs as a result of impaired binocular vision), refractive (in the presence of refractive errors - ametropia and untimely or inconsistent correction), anisometropic (in the presence of uncorrected anisometropia - differences in refraction between the right and left eyes), obscuration (with clouding of the ocular media) .
Convergent concomitant strabismus: Diagnosis[edit]
Anamnesis
When collecting anamnesis, it is necessary to consider:
• time of occurrence of strabismus and the duration of its existence (at what age did it appear, suddenly or gradually);
• whether there is diplopia, whether there was diplopia at the beginning of the development of strabismus;
• what can the occurrence of strabismus be associated with (general diseases, mental trauma, eye diseases, pathology of pregnancy and childbirth in the mother);
• is strabismus constant or periodic;
• at what age does the patient wear glasses constantly or periodically;
• previous treatment (surgical, functional);
• general health of the patient.
Physical examination
• Visual acuity with and without correction.
• Refractometry.
• Degree of deviation according to Hirschberg.
• Study of the magnitude of the squint angle and eye mobility in gaze positions: to the right, left, up and in diagonal positions.
Instrumental studies
1. Synoptophore
Research on synoptophore: objective angle, subjective angle, positive fusion reserves, negative fusion reserves, vertical fusion reserves, cycloreserves.
The synoptophore is one of the main haploscopic instruments. The separation of the visual fields of the right and left eyes is carried out mechanically in this device, using two separate movable optical tubes for each eye, in each of which paired test objects are presented to the subject for combination and fusion.
There are three pairs of test objects: for combining, merging and stereoscopy, which can move (horizontally, vertically, torsionally, i.e. when tilted to the sides).
2. Study of visual fixation
Fixation is checked using a large non-reflex ophthalmoscope or monobinoscope, determining which part of the patient’s fundus the shadow of the fixation needle falls on. Normally, fixation is foveal, or central, i.e. the image is recorded precisely by the central fovea of the retina. Non-central fixation can be parafoveal (the image is fixed close to the fovea), macular (closer to the periphery of the macula), paramacular (outside the macula), peripheral (peridiscal - in the optic disc).
Treatment
Conservative treatment of strabismus is aimed at achieving a symmetrical position of the eyes and the highest possible visual acuity, and correction of the forced position of the head. The course of hardware treatment includes exercises to develop binocular and stereoscopic vision. The approach to therapy is complex. The following non-drug methods are used: • Correction of refractive errors.
Correcting myopia can have a positive effect on eye position.
For mild farsightedness, the glasses designation is not shown. For medium and high farsightedness, optical correction helps improve visual acuity and allows better control of eye position. These measures are temporary. In the case of divergent strabismus, closing the eye, which does not tilt to the side, using a special occluder is indicated. For alternating strabismus, alternating occlusion is recommended to prevent amblyopia. • Orthopedic treatment.
It aims to develop and train bifoveal fusion reserves in the synoptophore. Special computer programs make it possible to increase the volume of synthesis and develop stereoscopic vision in vivo. Surgical treatment is used for divergent strabismus if orthophoria cannot be achieved conservatively. Indications for surgery are a constant angle of deviation, diplopia and forced head position. For stable exotropia with early onset, the main treatment is recession of the external rectum and resection of the internal rectus muscle. In the intermittent version, recession of the external rectus muscles of both eyes is performed first. If necessary, the intrinsic rectal muscles are then resected.