Strabismus is mainly a childhood disease. But adults can also suffer from it. And yet it is treatable. Strabismus should be treated to normalize visual functions and to prevent the development of dangerous complications that can lead to decreased vision.
Sometimes conventional treatment for strabismus does not have the desired effect. Then it would be advisable to prescribe surgical intervention to the patient. The choice of treatment methods is made exclusively by the doctor and depends on the indicators of the patient’s visual system.
Surgical treatment is a reliable method of treating strabismus. It allows you to restore the symmetrical position of the eyes by changing the muscle balance. Let's talk about the benefits of surgical treatment, how strabismus surgery is performed. Let's consider the types of operations and possible complications.
How does strabismus manifest?
Strabismus is an ophthalmological disease that is characterized by the inability, under certain circumstances, to focus the gaze on an object. In adults, this occurs as a result of dysfunction, including paralysis of some eye muscles.
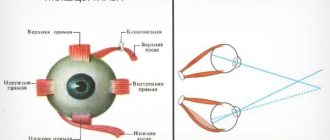
The classification of the disease is determined not only by the location of the eyeball, but also by the reasons why such pathology occurs. The movement of the eyeball is carried out through the work of six muscles that are attached to it.
The synchronization of the movements of both eyes is ensured by a complex system of nerve impulses in the brain.
Partially, it is traumatic brain injuries that also cause the development of the disease in an adult. One eyeball begins to move to the side.
Classification according to the location of the eyes and the angle of strabismus distinguishes the following types of disease: descending (the eyes are directed towards the middle); vertical strabismus (the apple of the eye is directed upward); divergent (eyes directed to the temples).
The main signs of strabismus are the visual deviation of one of the eyes or both eyeballs from the bridge of the nose.
Ophthalmologists also call such clinical manifestations of the disease that help the patient independently determine the presence or progression of the disease:
- the appearance of a dual image, the person’s vision has become worse (glasses are not able to correct it);
- squinting your eyes to improve focusing;
- third
- fourth
- fifth approximation of head movements in an attempt to improve image clarity.
Such symptoms of strabismus in adults occur quite often, and one thing can be said, they are the main ones at the first manifestations of the disease.
Strabismus in children: causes
The reasons why strabismus occurs in children can be divided into congenital and acquired. The former provoke the development of pathology in infancy, the latter - at any age.
Causes of strabismus in children under one year of age
Strabismus in infants is usually associated with congenital problems.
The main reasons why children are born with strabismus:
- infections suffered by the mother during pregnancy;
- hereditary diseases;
- insufficient development of the ocular apparatus due to prematurity;
- congenital eye defects;
- Cerebral palsy.
Causes of strabismus in children after one year
Strabismus can also develop in older children under the influence of external factors and previous diseases. The occurrence of strabismus is provoked by:
- myopia;
- cataract;
- neurological and mental disorders;
- past infections;
- excessive strain on the eyes;
- heredity;
- injuries to the head and eyes.
Known forms
Known forms.
Source: uglaznogo.ru Strabismus can be congenital or acquired. In the first case, it develops during the embryonic period, or within six months after the birth of the child. In the second case, strabismus can appear at any stage of a person’s life.
Strabismus can be convergent (horizontal), divergent and vertical. Vertical strabismus occurs when one or both eyes look down or up, but it is not common.
Monocular strabismus is a disorder of one eye. At the same time, it loses its functionality over time due to the brain adapting to the work of the only healthy eye. Alternating strabismus is a disorder of both eyes.
It is less dangerous than monocular, as it does not lead to loss of vision, since both eyes work, albeit alternately.
Convergent strabismus is characterized by a movement of the eyes towards the bridge of the nose, and divergent strabismus - by a movement towards the temples. Strabismus can also manifest itself in different ways.
Based on the causes of occurrence, strabismus is divided into concomitant and paralytic. The first form develops in children. Eye mobility is preserved, there is no double vision.
The second form of strabismus develops after damage to the eye muscles or paralysis; it can appear due to problems with the brain or nervous system. Paralytic strabismus is characterized by the fact that the eyes are not limited in movement.
Diagnosis of strabismus in children
External signs: how to understand that a child may have strabismus
The following reasons are considered the first reasons for concern:
- eyes do not move synchronously;
- the movement of the pupils is too fast or, conversely, imperceptible;
- the child bumps into objects directly in front of him;
- there are complaints of sore eyes and bright light;
- There is dizziness that goes away if you close one eye.
Each of these symptoms is an alarm bell that requires contacting an ophthalmologist.
Professional diagnostic methods: how to accurately determine strabismus in a child
Only a doctor can make an accurate diagnosis. The ophthalmologist not only conducts a visual examination, but also uses special equipment to clarify the details:
- level of visual acuity;
- angle of deviation of eye axes;
- fundus conditions;
- binocularity;
- concomitant diseases.
During the diagnosis, the following examinations are carried out:
- refractometry (including in conditions of drug-induced mydriasis);
- ophthalmoscopy;
- perimetry,
- Ultrasound of the eyeball.
- Determination of the subjective and objective angle of strabismus using a synoptophore
Possible treatment options
Possible treatment options.
Source: belmed.by Treatment of strabismus in adults is based on the same principles as treatment in children. But there are also differences. They are related to the cause of the disease.
- Correction of vision with glasses or contact lenses if strabismus is caused by nearsightedness or farsightedness of one of the eyes. Normalizing vision allows you to eliminate strabismus.
- Occlusion - stickers on the eyes. This is an additional treatment. The healthy eye is covered with a bandage or sticker to help the muscles in the affected eye become stronger.
- Hardware treatment is a program of exercises aimed at coordinating eye movements. Such exercises train the eyes and brain, teaching the muscles of both eyes to act in parallel.
- A surgical operation during which not only the external defect is eliminated, but also the length or location of the eye muscles is corrected.
In adults, strabismus often occurs as a complication of other diseases, therefore, treatment of strabismus should begin with identifying the cause and treating the underlying disease. If the underlying disease is not cured, then getting rid of strabismus may be useless - it will come back again.
Strabismus
Strabismus (strabismus, heterotropia) is a defect associated with incoordination of the activity of the eye muscles. One or more muscles are weaker than others, and this causes misalignment of focus. Normally, both eyes focus on one point, and the brain receives an image from each eye. With strabismus, the picture from one eye does not correspond to the picture from the other.
Treatment of strabismus in children and adults at the Euromed clinic
What is the danger of strabismus?
As a result of the discrepancy between the pictures, the visual analyzer ignores the image received from the squinting eye. As a result, this eye stops working and its vision decreases. In children, this is called “amblyopia” or “lazy myopia.”
Diagnosis of strabismus
When diagnosing strabismus, it is necessary to examine both the sensitive (sensory) and motor (motor) functions of the eye.
- When studying sensory functions, the acuity and degree of stability of binocular vision, depth (stereoscopic) vision and other functions are determined.
- When studying sensory functions, the mobility of the eyeballs, the magnitude of the deviation, and the degree of damage to the extraocular muscles are determined.
In addition to a general examination, diagnosing strabismus also requires special studies, which are carried out by an ophthalmologist using special techniques and instruments.
In particular, different types of haploscopy (separation of visual fields) are used, which make it possible to identify the degree of participation of the squinting eye in binocular vision.
To determine the angle of strabismus, the Hirschberg method is used, in which the position of the light reflex on the cornea is assessed.
The ophthalmologist collects a detailed medical history - finds out when strabismus occurred, its possible cause and characteristics, learns about the treatment already performed, as well as concomitant diseases.
A little about us
Eurpomed Kids are two children's clinics (in the north and south of the city), each of which has all the necessary specialists, including pediatric dentists, as well as its own laboratories and on-site pediatric service. To ensure that children grow up healthy, we work seven days a week from 9 to 22:00! We tell you more about why Euromed Kids clinics are the best here
Source: https://Deti-euromed.ru/glossary/kosoglazie/
Indications for surgery
Indications for surgery.
Source: medceh.ru The points that determine the need for surgical intervention in the treatment of the disease in question are:
- failure of complex non-surgical treatment, which took place for 1-2 years;
- non-accommodative strabismus;
- paralytic strabismus;
- with a very strong degree of strabismus. This requires several operations on one organ. If strabismus affects both eyes, the break in operations on the left/right eye should be at least 6 months.
The fundamental point of the operation is the revival of symmetry in terms of the placement of the organs of vision. This is done by regulating muscle balancing. The abilities of weak muscles are increased, and those of strong muscles are decreased.
Treatment of strabismus with synoptophore
In 1838, Sir Charles Whetstone created the first stereoscope, which subsequently underwent many changes before, at the beginning of the 20th century, Claude Worth introduced an amblyoscope based on it, intended to improve and stimulate binocular vision.
It was this apparatus that was the platform for the creation in 1929 of the first synoptophore, which allows for both diagnostic and therapeutic manipulations for strabismus.
A synoptophore is a device used for the diagnosis and treatment of disorders of motor and binocular functions of the eye. With its help, you can determine the angle of deviation of the eyes from the norm and obtain information about fusion reserves and the condition of the retina, as well as treat these changes.
Types of operations
Types of operations.
Source: eyepress.ru There are a large number of methods of surgical intervention on the extraocular muscles for concomitant strabismus. All of them can be divided into two groups:
- operations that weaken muscle action;
- operations that enhance their effect.
Of the operations that weaken the action of muscles, the most common are muscle recession (transplantation back) and partial myotomy (at small angles).
Of the operations that enhance the action of muscles, most ophthalmic surgeons use shortening of the muscle by partial resection and suturing it to the anatomical attachment site. The width of the palpebral fissure and the effect of surgery on it should also be taken into account.
Operations that strengthen the action of the muscle slightly narrow the palpebral fissure, and those that weaken it slightly widen it. With monolateral strabismus, surgery is performed only on the squinting eye; more often it is a combination of recession and resection. For alternating strabismus, symmetrical operations on both eyes are preferred.
Important
When there is a combination of horizontal and vertical deviation of the eyes, it is advisable to first perform surgery on the horizontal muscles with their vertical transposition. This often eliminates vertical deviation or significantly reduces it.
If necessary, the second stage corrects the vertical deviation by intervention on the vertical muscles.
In A-V syndrome, most ophthalmic surgeons perform symmetrical operations on two internal or two external rectus muscles.
Even with significant strabismus angles, it is not recommended to simultaneously operate on more than two muscles. If after the operation the residual angle of strabismus remains, then after 6-8 months the second stage of the operation is performed.
The child’s parents should be warned about this possibility so that the first operation is not regarded as a failure.
After strabismus surgery, a revision of optical correction is required. In case of convergent strabismus and hypermetropic refraction, in case of hypoeffect of the operation, the previous correction should be left or a light penalization should be prescribed with decentration of the glasses outward; when a symmetrical position of the eyes is established, the correction should be weakened.
If the eyes are symmetrical at distance vision, but there is a deviation towards the nose at near, bifocal glasses with stronger lenses in the lower part should be prescribed. If there is a tendency towards a hyper-effect, then spherical plus glasses should not be prescribed; for hypermetropic astigmatism, leave only cylindrical correction.
If there are vertical deviations after surgery, the appointment of elastic Fresnel prisms or decentration of spectacle lenses according to the method described above may be beneficial. In case of myopic refraction after surgery, glasses are prescribed according to the general rules for correcting this type of refraction, regardless of the type of strabismus and the position of the eyes (E.S. Avetisov, 1977).
A child operated on for concomitant strabismus must be regularly observed by an ophthalmologist and must receive orthopto-diploptic treatment. The microangles remaining after surgery must be eliminated during the treatment process. Hardware treatment should ensure the development of binocular and stereoscopic vision.
Often, during surgery to correct strabismus, a combination of the above types of surgical intervention (recession + resection) is used.
If, after surgery, there is residual strabismus that is not leveled by self-correction, repeated surgery may be required, which is usually performed after 6 to 8 months.
To achieve maximum effectiveness when performing surgery to correct strabismus, you must adhere to several basic principles.
- Excessive acceleration of the process of surgical correction of strabismus often leads to unsatisfactory results. Therefore, all manipulations should be carried out in doses (if necessary, in several stages).
- If it is necessary to weaken or strengthen individual muscles, dosed surgical intervention should be distributed evenly.
- When performing surgery on a specific muscle, it is necessary to maintain its connection with the eyeball.
Operations to correct strabismus
The goal of extraocular muscle surgery for strabismus is to achieve correct eye position and, if possible, restore binocular vision.
However, the first step in the treatment of childhood strabismus is the correction of any significant refractive errors and/or amblyopia.
Once the maximum possible visual function has been achieved in both eyes, any residual deviation must be corrected surgically.
There are 3 main types of operations for strabismus: (a) weakening, reducing the traction force, (b) strengthening, increasing the traction force, (c) changing the direction of action of the muscle.
surgeries that weaken muscle action
There are 3 types of interventions that weaken the action of the muscle: (a) recession, (b) myectomy, (c) posterior fixation sutures.
Recession This is the weakening of a muscle by moving its insertion posteriorly towards the origin of the muscle. Recession can be performed on any muscle except the superior oblique.
1. Recession of the rectus muscle
a) after exposure of the muscle, two absorbable sutures are placed on the outer quarter of the width of the tendon; b) the tendon is cut off from the sclera, the amount of recession is measured and marked on the sclera with a compass; c) the stump is sutured to the sclera posterior to the original site of attachment
2. Recession of the inferior oblique muscle a) exposure of the muscle belly is achieved through the inferotemporal arcuate incision;
b) one or two absorbable sutures are placed on the muscle near the place of its attachment; p) the muscle is cut off, and the stump is sutured to the sclera 2 mm from the temporal edge (the place of attachment of the inferior rectus muscle).
Myectomy The procedure involves cutting off a muscle at its insertion without rejoining it. This technique is most often used to relieve hyperfunction of the inferior oblique muscle. On the rectus muscles, this intervention is performed very rarely with large contracted muscles.
Posterior fixation sutures The principle of this intervention (Faden operation) is to reduce the strength of the muscles in the direction of their action without changing the place of attachment.
The Faden procedure can be used to treat VDD and also to weaken the horizontal rectus muscles. When correcting VDD, recession of the superior rectus muscle is usually performed first.
The muscle belly is then sutured to the sclera with a non-absorbable suture at a distance of 12 mm posterior to its insertion.
surgeries that enhance muscle action
1. Resection of the muscle increases its effective traction.
This procedure is suitable only for rectus muscles and includes the following interventions: a) after exposure of the muscle, two absorbable sutures are passed through the muscle at marked points posterior to its insertion; b) part of the muscle anterior to the sutures is excised and the stump is sutured to the original insertion site
3. Formation of a muscle or tendon fold is usually used to enhance the action of the superior oblique muscle in congenital fourth cranial nerve palsy.
2. Translation (suturing the muscle closer to the limbus) may provide increased action after previous rectus recession.
Treatment of paralytic strabismus
Paralysis of the external rectus muscle Surgical intervention for palsy of the sixth CN should be performed only if spontaneous improvement does not occur, which can be expected no earlier than after 6 months. There are 2 main interventions that improve abduction:
1. Operation Hummelshelm
a) recession of the internal rectus muscle; b) the lateral halves of the superior and inferior rectus muscles are cut off and sutured to the upper and lower edges of the paretic lateral rectus muscles. Since during this intervention all three muscles are separated from the eyeball, there is a risk of postoperative ischemia of the anterior segment. To avoid this complication, recession of the internal rectus muscle can be replaced by chemodenervation.
2. Jensen's operation improves abduction and is combined with recession or CI toxin injection. bolulinum into the external rectus muscle.
a) the superior, external and inferior rectus muscles are split along their length; b) using non-absorbable threads, the outer half of the superior rectus muscle is fixed to the upper half of the external rectus muscle, and the lower half of the external rectus muscle is fixed to the outer half of the inferior rectus muscle.
Paralysis of the superior oblique muscle. Surgical intervention is indicated for forced position of the head and diplopia that cannot be eliminated with the help of prisms.
1. Congenital hypertropia with a large angle in the primary position. In this case, a fold of the superior oblique muscle is performed.
2. Acquired a) small hypertropia is corrected by ipsilateral weakening of the inferior oblique muscle; b) acquired hypertropia with a medium and large angle is eliminated by ipsilateral weakening of the inferior oblique muscle, combined with ipsilateral weakening of the superior rectus muscle and/or contralateral weakening of the superior rectus muscle. It must be taken into account that weakening of the inferior oblique and superior rectus muscles of the same eye can lead to hyperelevation; c) excyclotropia without hypertropia is eliminated by the Nagada-Ito operation, which includes splitting and anterolateral transposition of the outer half of the superior oblique tendon.
Adjustable seams
Indications In some cases, the best results of surgical treatment for strabismus are obtained with the technique of adjustable sutures. Special indications include the need for correct eye position and cases where the results of traditional interventions are difficult to predict.
For example, acquired vertical deviations due to endocrine myopathy or the consequences of an impacted fracture of the orbital floor. Other relative indications include palsy of the sixth pair of cranial nerves (CN), exotropia in adults, and repeated operations for scarring of surrounding tissues, when the result of the operation may be unpredictable.
The main contraindication is the patient’s young age or the inability to postoperatively adjust the sutures.
First stage
1. Exposure of the muscle, sutures are applied, the tendon is separated from the sclera (as in case of rectus muscle recession). 2. The two ends of the thread are passed close to each other together through the stump at the site of attachment.3. The second suture is tied and pulled tightly around the muscle suture in front to secure it from the stump 4. One end of the suture is cut and the two ends are tied together to form a loop.5. The conjunctiva remains open.
Postoperative regulation
1. Assess the position of the eyes.2. If the position of the eyes is satisfactory, then the muscle suture is tied and the long ends of the thread are shortened.3. If more recession is required, the knot is pulled anteriorly along the suture of the muscle, providing additional relaxation of the recessioned muscle, and pushed posteriorly.4. If less recession is required, the muscle suture is pulled anteriorly and the knot is pulled in the direction opposite to the muscle stump.5. The conjunctiva is sutured.
A similar technique is used for resection of the rectus muscle.
Chemodenervation with botulinum toxin for strabismus
Temporary paralysis of the extraocular muscle can be created in addition to the transposition described previously, or in isolation.
The main indications for chemodenervation: • To determine the function of the external rectus muscle in CN VI palsy, in which contracture of the internal rectus muscle interferes with abduction. A small dose of CI toxin. bolulinum is injected into the belly of the antagonist in the hyperfunction (internal rectus muscle) under electromyographic control.
Temporary paralysis of the muscle causes it to relax, and the action of the horizontal muscles of the eye is balanced, allowing the function of the external rectus muscle to be assessed.• To determine the risk of postoperative diplopia and assess the potential of the BZ. For example, an adult patient with left divergent strabismus and high visual acuity in both eyes receives an injection of CI toxin.
bolulinum into the left external rectus muscle will result in either eye alignment or convergence.• However, placing a corrective prism in front of the deviated eye is often a simpler and more accurate method of assessing the risk of postoperative diplopia. If one of the methods indicates the possibility of diplopia, the patient can be informed about this. However, such a dilopia.
usually disappears spontaneously.
Source: https://zrenue.com/operacii/88-operacii-kosoglazija.html
Read more about surgical treatment of strabismus
Features of this method
Early surgical treatment is also recommended for children with vertical strabismus. It is usually congenital and cannot be treated with orthoptic treatment due to the limited vertical fusion reserves.
The surgical operation often takes place in 2-3 stages, if necessary, pleoptic treatment is carried out, after restoration of the correct position of the eyes - orthoptic-diploptic treatment.
You should not rush into surgery in children with partial accommodative strabismus and a small angle of deviation - up to 10 degrees - and a clear tendency to decrease it.
In these cases, it is necessary to extend active conservative treatment using all indicated and available methods, and the decision on surgical treatment should be postponed to a later date. In some of these children, strabismus treatment was successfully completed without surgery.
The question remains debatable about the need for surgical treatment of children with convergent strabismus in cases where with glasses there is a symmetrical position of the eyes and binocular vision, and without glasses there is a deviation to the nose and binocular vision is impaired.
Many ophthalmologists believe that in such cases it is necessary to surgically weaken the internal rectus muscles (their recession) and achieve the correct position of the eyes without glasses.
The experience of observing such children after operations does not confirm the correctness of this position, since in some children with similar data the appearance of secondary divergent strabismus was noted.
After analyzing cases of this unpleasant complication, we identified the reasons for its occurrence.
- The binocular vision that existed before the operation was destroyed during surgery on the extraocular muscles, and after the operation no vigorous measures were taken to restore it, to develop strong fusion reserves that could prevent secondary deviation of the eyeball.
- In some children, there was a change in the configuration of the orbits due to the growth of the bones of the facial skull, which, with instability or absence of binocular vision, led to the appearance of divergent strabismus.
- In some children, the optical plus spherical correction was not weakened in a timely manner, which could have prevented the appearance of outward deviation.
If a child has established a symmetrical position of the eyes and has developed binocular vision with glasses, then there is a chance of achieving this without glasses. This requires time and persistent treatment.
In such cases, the extraocular muscles are trained on a muscle trainer, we strengthen the external rectus muscles with electrical stimulation, we develop and train negative fusional reserves, we carry out exercises to dissociate between accommodation and convergence, and we strengthen binocular vision with orthopto-diploptic exercises.
Symmetrical eye position and binocular vision are gradually established without glasses.
If for some reason the patient cannot receive such treatment, then he cannot be operated on. Having destroyed his binocular vision through the operation and not being able to restore it, we increase the risk of developing secondary divergent strabismus.
Patients with asymmetric binocular vision should not be operated on. If there is a deviation, when examined on a color test and with the help of striped Bagolini glasses, binocular vision is determined, and on a synoptophore in the zero position of the optical heads, a fusion of objects is determined.
After surgical restoration of the symmetrical position of the eyes, these patients develop persistent diplopia, which disappears only after the eyes return to their previous oblique position (relapse of strabismus).
Children with such an anomaly are subject to long-term vigorous treatment to destroy and weaken the abnormal functional connections formed in the higher parts of the visual analyzer and only after treatment can they be operated on.
Main stages of surgery
Surgical intervention in the treatment of concomitant strabismus is used in cases where conservative methods fail to achieve symmetrical eye position. All children with non-accommodative strabismus and 35-40% with partially accommodative strabismus are subject to surgical treatment.
Most ophthalmologists consider the most favorable age for surgery to be 4-6 years (before entering school), when the effect of glasses on the angle of strabismus has already been clearly determined and it is already possible to carry out orthoptic exercises in the pre- and postoperative periods.
The exception is children with congenital and early-onset strabismus with a large angle of deviation - 45° or more. Correcting such a large deviation with a one-time operation is impossible, so surgical treatment is carried out in two and sometimes three stages.
The first stage - reducing the angle of strabismus - should be carried out, if possible, earlier, in the first or second year of life, as soon as the general condition of the child allows the use of anesthesia and the operation. The second stage - correction of strabismus - can be carried out at 4 - 5 years.
The entire period between the first and second operations, the child should receive the treatment indicated in each specific case: optical and therapeutic correction, direct or alternating occlusion, penalization, training of the extraocular muscles, and, if possible, hardware pleoptic and orthoptic treatment.
Concomitant strabismus
Concomitant strabismus, according to the modern concept, is characterized by unlimited eye mobility, equality of deviation angles (primary and secondary) in all directions of gaze (or their difference not exceeding 5 ave. D).
Traditionally, this type of strabismus is divided into partially accommodative, accommodative and non-accommodative. According to the new classification, accommodative strabismus is divided into refractive, non-refractive, combined (or mixed), and decompensated.
Accommodative strabismus
Refractive accommodative strabismus is characterized by the presence of high ametropia (above 4-10 diopters), the same magnitude of deviation angles without correction near and far, which is completely eliminated by spectacle correction of ametropia. AK/A is the ratio of the normal value. Treatment of the pathology is conservative, with optical correction sufficient to eliminate deviation and develop binocular vision. In this case, the strength of optical correction, during the treatment process, must be gradually reduced under the control of hardware data from the synoptophore and color test to stimulate the physiological processes of emmetropization.
With non-refractive accommodative strabismus (usually convergent), there is no ametropia, or it is very insignificant, and the angle of deviation of fixation near exceeds the angle of deviation into the distance. Complete correction of ametropia is not able to eliminate the deviation and it appears every time accommodation stress appears. AK/A - high ratio. Deviation is eliminated by hypercorrection convex sphere, usually + 3.0 diopters. As a treatment, convex sphere is prescribed for close range and development of binocular vision. This type of strabismus corrects spontaneously in children over 10 years of age.
With combined accommodative strabismus, a combination of non-refractive and refractive accommodative esotropia is observed. It is characterized by the presence of hypermetropia, which exceeds the age norm and a high AA/A ratio. The angle of esotropia without correction for near exceeds the angle of esotropia for distance. Orthoptic therapy is recommended as treatment. Deviation is eliminated with bifocal glasses, which correct ametropia in the upper part, and have 2-3 diopters more in the lower part. When binocular vision improves to normal, the strength of optical correction is gradually reduced. If the distance deviation angle remains the same even after 10 years, the child is indicated for surgery to correct the deviation angle that arose during distance fixation in order to cancel the constant wearing of glasses.
Decompensated accommodative strabismus has a non-accommodative component, which occurs secondary to accommodative strabismus that has existed for a long time. This distinguishes it from partially accommodative strabismus, which is initially characterized by the presence of a non-accommodative component. In the absence of treatment for accommodative strabismus, its treatment is unsystematic, or with the use of optical correction, which is insufficient to correct the angle of deviation, accommodative strabismus often turns into partially accommodative or even non-accommodative.
To treat it, it is recommended to correct the angle of the non-accommodative component surgically and further orthoptic therapy after surgery. Once normal binocular vision is achieved, the power of optical correction is gradually reduced.
Non-accommodative strabismus
In ophthalmology, it is customary to distinguish three forms of non-accommodative strabismus: horizontal, vertical and mixed. Horizontal non-accommodative concomitant strabismus is the main form and the most common type of this pathology. It occurs due to a violation of the equilibrium innervation of divergence and convergence. Ametropia, with this form of strabismus, is absent or has a mild degree (in rare cases, a high degree). The AK/A ratio is normal. Accommodation does not affect the deviation angle and it is the same for distance and near with or without correction. Non-permanent strabismus in preschool children is treated conservatively using prismatic correction. If there is no significant effect of orthoptic treatment, surgery and subsequent orthoptics are recommended.
Essential infantile (congenital) tropia (usually esotropia), which occurs from birth or in the first six months of a child’s life, is characterized by the absence of ametropia and preserved eye mobility. This type of strabismus is characterized by the presence of large (over 30 diopters) constant angles of deviation, as well as cross fixation and varying degrees of severity of latent nystagmus. In addition, it is accompanied by disturbances in pursuit and saccadic eye movements, asymmetry of optokinetic nystagmus, the presence of A, V, X phenomena, and a vertical component. Surgical treatment of infantile strabismus should be early (before the age of two years), however, even in this case, normal binocular vision may not be achieved in everyone. In half of the patients, orthotropia is established with the presence of peripheral fusion without stereopsis or with its insignificant value.
The symptoms of blocked nystagmus syndrome are known: esotropia of the eyes with a fairly large angle of deviation, forced rotation of the head, development of horizontal jerky nystagmus in a straight position of the head and in the primary position of the eyes. It requires early surgical treatment, in the first year and a half of a child’s life with recession of the medial rectus muscle (increased dosage of 6-7 mm).
Sensory derivation strabismus, or sensory strabismus, is a non-accommodative concomitant strabismus, which occurs due to a decrease in visual acuity in case of clouding of the refractive media of the eye. This happens with diseases of the retina or optic nerve. In preschool children, as a rule, convergent sensory strabismus is detected. Schoolchildren and adults usually develop divergent sensory strabismus. The functional cure of sensory strabismus is associated with the possibility of restoring visual acuity. If this is not possible, cosmetic surgery is indicated, which is most effective in children 14-16 years old or older. Convergent strabismus in people with a high degree of myopia is sensory. Such strabismus is treated by correction of myopia, which is due to a significant increase in visual acuity.
Microtropia (microstrabismus) is a unique type of strabismus with fairly highly developed binocularity and reduced or completely absent stereoscopic vision. Microtropia is characterized by the presence of a deviation angle below 5 degrees. (up to 10 diopters), often combined with anisometropia. As a rule, convergent microtropia (esomicrotropia) occurs. It is customary to distinguish between primary and secondary microtropia. In essence, primary microtropia (monofixation syndrome) is a sensory strabismus and is the result of an adaptation of the visual system to abnormal binocular fixation. This pathology often accompanies amblyopia with eccentric fixation and is characterized by abnormal retinal correspondence of the harmonic type. With primary microstrabismus, it is possible to cure amblyopia, although the angle of strabismus is often irremediable and surgical treatment is impractical. Secondary microtropia is a consequence of motor disorders. It often occurs during the treatment of large deviation angles, therefore, in addition to microdeviation, it is characterized by the substitution of binocular vision and non-harmonic correspondence of the retinas. Secondary microtropia is curable.
Swan syndrome or blind spot and its symptom are characterized by the existing stable angle of esotropia, with a value corresponding to the angle of projection of this blind spot in the field of view (about 10-15 degrees and 20-30 diopters). Blind spot syndrome is characterized by normal retinal correspondence and high visual acuity in both eyes. The blind spot symptom develops against the background of abnormal retinal correspondence and is accompanied by amblyopia. The blind spot, in both conditions, acts as a scotoma and, with binocular fixation, is used to eliminate diplopia. The blind spot symptom is not amenable to either orthoptic or surgical treatment, unlike blind spot syndrome.
Excess of divergence is the name given to divergent strabismus, which occurs when fixating into the distance. Fixation close, however, does not cause deviation. Convergence is normal. Binocular vision may be normal near, but completely absent at a distance. Excess of divergence can only be treated surgically. The operation of choice is recession of the rectus lateralis muscle within 6-10 mm (unilateral or bilateral for deviation, respectively, up to 10 degrees, and more than 15 degrees)
Acute strabismus is a sudden deviation that is accompanied by diplopia and has all the signs of concordance. This strabismus is caused by decompensation of heterophoria, which occurs due to mental trauma, nervous strain, and severe fatigue. Consultation with a neurologist is required. Treatment – orthoptic and prismatic correction. If there is no effect, surgery may be scheduled after 6 months.
Cyclic strabismus is friendly and appears at regular intervals. In the absence of strabismus, binocular vision is not impaired. The etiology of this type of disease has not been precisely established. There is a hypothesis about its neurological origin, and therefore the treatment is neurological.
Secondary concomitant non-accommodative strabismus is a strabismus in the opposite direction to the original one, resulting from spectacle or surgical overcorrection. To eliminate it, reduce or cancel the spectacle correction altogether and switch to contact correction. In addition, prismatic correction is prescribed, with repeated surgery to correct the resulting hypereffect.
Vertical strabismus has two main forms: hypotropia - downward deviation of the eye and hypertropia - upward deviation of the eye. At the same time, all signs of friendship are observed. Diplopia, ptosis and forced head rotation are absent. Treatment is only surgical.
Manifestations of dissociated vertical deviation (DVD) are alternating deviations to the top of one or the other eye. Treatment is surgery.
Divergent vertical concomitant non-accommodative strabismus is manifested by upward deviation of one eye. And if you fixate with this eye, the paired one begins to deviate downwards. Often, pseudoptosis can be observed in an eye that deviates to the bottom, which disappears when fixed with that eye. Treatment is surgical, which also leads to the disappearance of pseudoptosis.
The mixed form of concomitant non-accommodative strabismus, depending on the vertical and horizontal angles of deviation, is divided into horizontal strabismus (convergent/divergent) with a vertical component and vertical (hypotropia/hypertropia) strabismus with a horizontal component. Treatment is surgical.
A special form of mixed strabismus is Avetisov syndrome, a vertical-horizontal moving deviation. With this type of disease, one of the eyes deviates inwards, with a vertical upward deviation of the other, when fixed first. It is treated surgically.
A “heavy, drooping eye” against the background of a high degree of myopia is hypotropia, accompanied by slight esotropia. Treatment is surgical resection of the muscle that has insufficient action.
Should you decide to have surgery?
When deciding to undergo surgery for strabismus, you need to know that such a surgical intervention allows you to get rid of the external manifestations of strabismus, but does not always return the ability to see well.
In the ophthalmology clinic, operations for strabismus are performed on patients who, for one reason or another, were not treated in childhood or who developed strabismus in adulthood, for example, as a result of injury. There are two types of operations for strabismus: strengthening and weakening.
During weakening surgery, the attachment site of the muscle is changed and it is transplanted further from the cornea. That is, the action of a strong muscle (the one towards which the eye is deviated) weakens.
During augmentation surgery, the muscle is shortened by removing part of it, but the attachment site of the muscle to the eyeball remains the same.
That is, the action of the weak, opposite muscle is enhanced. As a result, such surgical intervention allows you to restore the correct muscle balance, strengthen or weaken one of the muscles that move the eyeball.
The type of operation is determined by the surgeon directly on the operating table, since with such a surgical intervention it is necessary to take into account many features: the angle of strabismus, the location of the muscles in a particular person, the condition of the oculomotor system, the patient’s age, and others.
Typically, several muscles are operated on. Sometimes both eyes are operated on at once; in some types of strabismus, only one eye is operated on. There are cases when an ophthalmic surgeon performs a combined operation on both eyes, both on strong and weak muscles. This operation is performed in several stages.
Chemodenervation with botulinum toxin for strabismus
Temporary paralysis of the extraocular muscle can be created in addition to the transposition described previously, or in isolation.
The main indications for chemodenervation: • To determine the function of the external rectus muscle in CN VI palsy, in which contracture of the internal rectus muscle interferes with abduction. A small dose of CI toxin. bolulinum is injected into the belly of the antagonist in the hyperfunction (internal rectus muscle) under electromyographic control. Temporary paralysis of the muscle causes it to relax, and the action of the horizontal muscles of the eye is balanced, allowing the function of the external rectus muscle to be assessed. • To determine the risk of postoperative diplopia and assess the potential of BZ. For example, an adult patient with left divergent strabismus and high visual acuity in both eyes receives an injection of CI toxin. bolulinum into the external rectus muscle of the left eye will result in either eye alignment or convergence. • However, placing a corrective prism in front of the deviated eye is often a simpler and more accurate method of assessing the risk of postoperative diplopia. If one of the methods indicates the possibility of diplopia, the patient can be informed about this. However, such a dilopia. usually disappears spontaneously.
Preparing for surgery
Preparing for surgery.
Source: simptom.org Surgical treatment is an important stage in the treatment of concomitant strabismus. The course of further treatment of strabismus and its outcome depend on the results of the operation. In addition, the operation is a great psychological and emotional burden on the child and his parents.
To obtain the desired results of the operation, good preoperative preparation is necessary. It includes: psychological preparation of the child, a full examination of his physical condition and timely correction of identified deviations. Sanitation of the oral cavity and ENT organs is mandatory.
Ophthalmic preparation is very important. In case of monolateral strabismus, amblyopia must be eliminated in the preoperative period in order to develop binocular vision after surgery, and not to carry out occlusion.
In cases of alternating strabismus, it is necessary to alternately turn off both eyes for 3-6 months to weaken abnormal functional nerve connections in the higher parts of the visual analyzer, formed as a result of the asymmetric position of the eyes. Training of the oculomotor muscles is also necessary.
Treatment on the synoptophore is highly desirable in order to achieve bifoveal fusion at an objective angle of strabismus and the development of fusional reserves. In complex cases of damage to the oculomotor system when combining horizontal strabismus (convergent and divergent) with vertical deviation, it is recommended to conduct a coordimetric study.
Analysis of coordiograms allows us to identify affected and weakened muscles, as well as muscles in a state of hyperfunction, and plan surgical intervention in the most rational way.
Treatment of strabismus in children without surgery
Glasses for strabismus
In addition to regular glasses that correct refractive pathologies that can cause strabismus, special glasses and lenses are used to correct strabismus in children without surgery.
Glasses with occluder
What they look like: glasses with a darkened or covered lens or a patch applied to the healthy eye.
The essence of the method: blocking vision in the healthy eye creates conditions for fixation with the squinting eye and connecting it to active activity.
When useful: for strabismus associated with amblyopia (“lazy eye”)
Nuances:
- the healthy eye should be closed from 1 hour a day until the entire period of active activity of the child. The occlusion mode is prescribed by an ophthalmologist.
- Duration of therapy is 2-3 years.
Prismatic lenses
What they look like: lenses for glasses of a special shape, thickened on the side opposite to the slant of the eye.
The essence of the method: the lens corrects the angle of view, promoting the formation of binocular vision.
When useful: when binocular vision is impaired.
Nuances:
- Only an ophthalmologist can choose the right lens;
- The method is effective for both hidden and obvious strabismus.
Fresnel prisms
What they look like: thin prismatic plates that are attached to the main lenses of glasses from the inside.
The essence of the method: promotes the development of binocular vision.
When useful: when binocular vision is impaired.
Nuances:
- usually prescribed as adjunctive therapy;
- Only a doctor can install prisms on glasses.
Hardware treatment of strabismus
Treatment using hardware techniques is aimed at:
- strengthening the muscles of the sore eye;
- relaxation of the healthy eye;
- development of binocular vision.
This treatment is carried out in courses of 10-20 days with daily procedures.
Chemodenervation with botulinum toxin for strabismus
Botulinum toxin is used to treat paralytic strabismus caused by paralysis or muscle weakness. A Botox injection paralyzes the muscles, preventing them from pulling the eyeball to the side. As a result, the position of the eye is leveled. The effect of the injection lasts about 6 months. After six months, the muscles either return to normal and the strabismus disappears, or they return to their original state and the next stabilizing injection is required.
Contraindications to treatment of strabismus with Botox:
- poor blood clotting;
- oncology;
- high degree of myopia;
- eyelid ptosis;
- hernias on the eyelids;
- hemophilia;
- individual intolerance to the drug;
- pathologies of the organs of the excretory system.
results
Preparing for surgery.
Source: glazatochka.ru Surgical treatment of strabismus allows you to correct a cosmetic defect, which is a strong traumatic factor for patients of any age.
However, to restore visual functions (i.e., binocular vision) after surgery, an integrated approach is required, which includes pleoptic therapy (it is aimed at treating amblyopia accompanying strabismus) and orthoptodiploptic therapy (restoration of depth vision and binocular functions).
A one-stage operation to correct strabismus in adults can be performed on an outpatient basis; when treating children, hospitalization is necessary in most cases.
The approximate recovery time after surgery is 1 week, but to recreate full binocular vision, i.e. The ability to see a three-dimensional image with both eyes at the same time is not enough.
During the time that a person had strabismus, the brain, figuratively speaking, “forgot how” to combine images from both eyes into a single image, and it will take quite a long time and significant effort to “teach” the brain this again.
It should be mentioned that, like any operation, surgical correction of strabismus may be accompanied by the development of certain complications. One of the most common complications of strabismus surgery is excessive correction (so-called hypercorrection), caused by errors in calculations.
Overcorrection may occur immediately after surgery, or may develop after some time. For example, if the operation was performed in childhood, then in adolescence, when the eye grows, the child may experience strabismus again. This complication is not irreparable and can be easily corrected with surgery.
When choosing a clinic for an operation to correct strabismus, it is important to study the clinic’s capabilities, living conditions, whether the clinic is equipped with modern equipment and other important points. It is equally important to choose the right doctor to perform the operation. After all, the prognosis of treatment will fully depend on his professionalism.
If you or your relatives have already undergone surgery to correct strabismus, we will be grateful if you leave feedback about the intervention and the clinic where the procedure was performed, as well as the results obtained.
Strabismus correction
Despite the fact that modern surgical techniques are very effective, it is impossible to completely guarantee the success of strabismus correction surgery.
In cases where slight strabismus is still observed after surgery, it is usually not a functional or cosmetic hindrance.
On the other hand, in cases where a significant degree of strabismus persists, repeat surgery may be required.
Laser correction of strabismus
Our eyes are an organ that must be protected. There are many eye diseases, including strabismus.
Strabismus is a disease in which the ocular muscles responsible for the functioning of the eyes do not work properly, resulting in a visual defect.
In simple terms, strabismus is when the eyes look in different directions. Let's look at what treatment methods for strabismus exist.
Laser surgery
Often patients are interested in whether there is a laser treatment for strabismus. We'll have to disappoint you. No, you won’t be able to return your eyes to their proper position; such a technique does not exist yet.
The fact is that during surgery, the doctor either cuts the muscle to weaken it or, on the contrary, hems or tightens the weakened muscle, or both, depending on the type and type of strabismus.
Unfortunately, such a procedure cannot be done using a laser.
As you can see, no matter how popular the laser method is, laser correction will not help at all in the treatment of this disease.
Treatment of strabismus
Strabismus is a disease that should not be neglected, otherwise it will be difficult to correct the position of the eyes later.
Therapeutic methods
Treatment of strabismus is recommended to be carried out comprehensively, but, nevertheless, several treatment methods are distinguished.
- The diploptic method is a method in which stereoscopic and binocular vision is restored in natural conditions.
- Orthoptic treatment is the restoration of binocular vision (i.e., restoration of the ability of the eyes to connect two pictures together) is carried out using special computer programs and synoptic devices.
- The pleoptic method is when the diseased squinting eye is subjected to strong visual stress. In this case, a variety of therapeutic computer programs are used.
- Method of using convergence trainer for eye training. This improves the functioning of the muscles that are responsible for the movement of the eyeball.
If we consider the individual path of treatment and correction of strabismus, it will look something like this:
- First, amblyopia is treated to improve the quality of vision. In this case, the method of gluing the eye and parallel treatment with the help of devices are used.
- As soon as the quality of vision improves, they begin to work on restoring binocular vision, i.e. restore connection between the eyes.
- The next point is to restore the balance between the muscles. The fact is that strabismus is caused by improper muscle function. It can be restored surgically, but this method is not always used.
- At the end of treatment, stereoscopic vision is restored.
The best way to treat strabismus is decided by the doctor after a thorough examination.
Surgical intervention
Surgical intervention is used to straighten the eyes cosmetically and only if nothing else helps to “put the eyes back in place.” The fact is that the operation practically does not help restore binocular vision. The operation is performed on an outpatient basis, and local anesthesia is given. The patient can go home on the same day.
What kind of surgery will need to be performed is decided by the doctor on the operating table. The choice of surgery depends on which muscles do not work and what needs to be corrected and how, since each person has an individual strabismus, which means the dysfunction of the muscles and their location are also individual. Most often, operations are performed on only one eye, but it is not uncommon for both eyes to be operated on.
The essence of the operations is that the doctor needs to weaken or strengthen the eye muscles that are responsible for eye movement. As for postoperative rehabilitation, it lasts about a week. But, nevertheless, despite the surgical intervention, doctors strongly advise not to stop treatment at this stage and continue treatment using training on the devices.
This will restore vision partially or completely.
Whatever method of treating strabismus is chosen, remember that strabismus is best treated in the early stages.
Principles of surgical treatment
The goal of extraocular muscle surgery for strabismus is to achieve correct eye position and, if possible, restore binocular vision.
However, the first step in the treatment of childhood strabismus is the correction of any significant refractive errors and/or amblyopia.
Once the maximum possible visual function has been achieved in both eyes, any residual deviation must be corrected surgically.
There are 3 main types of operations for strabismus: (a) weakening, reducing the traction force, (b) strengthening, increasing the traction force, (c) changing the direction of action of the muscle.