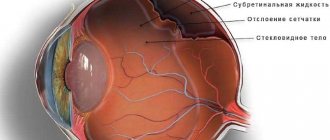
Retinal PPLC is a procedure aimed at strengthening and preventing retinal detachment, which performs the function of transmitting images to the visual parts of the brain. If retinal detachment develops, a person’s lateral vision disappears, a veil, spots, and floating spots appear before the eyes, and the quality of vision is significantly reduced. Progression of the disease can lead to blindness. The cause of its development may be retinal dystrophy, trauma, chronic inflammation of the iris or vascular membranes, etc.
The essence of the method
During preventive peripheral laser coagulation, a specialist treats thinned areas of the retina using a laser, soldering them in weak spots. This technique also allows you to improve blood circulation in the eye tissues, nutrition of the affected parts of the retina, and prevent fluid from penetrating under it.
The PPLC procedure cannot significantly improve vision. Its main goal is to reduce the risk of complications. The quality of a person’s visual perception after such an operation can improve in the absence of concomitant eye diseases that affect vision.
Advantages and disadvantages
Strengthening the retina with laser has a huge list of unconditional advantages:
- No need for general anesthesia.
- The risks of bleeding during manipulation are eliminated.
- The rehabilitation period lasts only one day.
- The procedure does not affect the fundus of the eye and does not cause infectious complications.
- Easy to carry out.
- Availability.
- Minimum side effects.
- No pain or bruising both during and after the procedure.
- Additional injuries are excluded.
- No need for the patient to stay in a medical facility after surgery.
- The manipulation takes a minimum of time and does not affect the patient’s usual rhythm of life.
- Possibility of carrying out the procedure during pregnancy.
As for the disadvantages, laser photocoagulation is not able to cope with age-related changes in the visual apparatus. The results of the operation may be unstable. There are age restrictions. There are risks of complications.
Laser coagulation is a non-contact, minimally invasive procedure
Indications for PPLC
Often this operation is performed on patients who have been prescribed laser vision correction. According to statistics, about 60% of all people with visual impairments have problems with the retina and need to strengthen it. Therefore, before performing laser correction, the ophthalmologist may recommend PPLC to the patient.
Indications for its implementation are:
- Diabetic retinopathy.
- Tumor processes in the fundus of the eye.
- Local retinal detachment.
- Retinal angiomatosis.
- Retinal vein thrombosis.
- Peripheral retinal dystrophy.
What is laser coagulation of the retina and when is it performed?
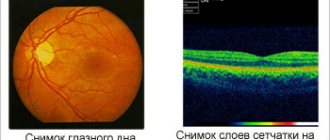
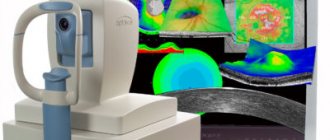
The operation to strengthen the retina is called laser coagulation. Using special equipment, the ophthalmic surgeon directs a laser beam into the patient’s eye and “seals” the problem area. The procedure allows you to stop the progression of diseases and pathological changes in the retina. There are several indications for laser surgery to strengthen the retina.
- Dystrophy of the retina. With this disease, irreversible damage to the photoreceptors occurs, as a result of which visual acuity decreases up to complete blindness.
- Retinoschisis. Against the background of dystrophy, retinoschisis often develops - a separation of the retina when fluid accumulates between its layers. Laser coagulation is effectively used to treat this pathology.
- Vascular changes and diseases. Laser surgery to strengthen the retina can be prescribed for thrombosis of the central vein, obstruction of the central artery, and also to prevent pathological proliferation of blood vessels.
- Retinopathy. The disease is characterized by damage to the vessels of the retina, which leads to impaired blood supply to the organ, atrophy of the optic nerve and loss of vision.
- Detachment. Detachment is a pathological process in which the retina is separated from the choroid, as a result, its nutrition is disrupted, and vision begins to deteriorate until complete blindness.
Also, laser coagulation of the retina is indicated for certain types of neoplasms and as a prevention of the development of pathological changes in the fundus.
Technique
A person to whom a doctor has prescribed surgery must undergo a full examination of the eye organs and be tested by a local physician. To prepare for surgery, the patient may be hospitalized on the day of the proposed PPLC.
The procedure itself is carried out in the following order:
- The person being operated on is put on a sterile headdress and a medical gown. The entire operation must be carried out under perfectly sterile conditions to prevent accidental infection of the eye.
- Special drops are injected into the patient's eyes, which have an anesthetic effect and help dilate the pupil.
- Then a special lens is placed on the eye, the design of which resembles the eyepiece of a microscope. It is used to focus the laser beam and point it to the desired part of the eye.
- Next, using a laser, the specialist glues together weak and detached areas of the retina. The duration of the procedure is about 20 minutes.
- At the end of the procedure, the patient remains under the supervision of a specialist for 30 minutes.
During the operation, adhesions are formed on the retina, which prevent further detachment. Within 1–2 weeks after the procedure, the adhesions become fully formed and only after this the doctor will be able to judge how successful the operation was.
During the operation, the patient is in a sitting position. He feels the impact of the laser device as bright flashes of light or a barely noticeable tingling sensation. The procedure is not painful, but some patients may experience dizziness or a gag reflex. In order for the patient to undergo the operation more comfortably, the doctor recommends that he concentrate on the second eye.
The patient will be able to return home on the same day as the operation. Before discharge, the doctor gives him recommendations regarding further behavior and care of the operated eye.
Reviews
Patient reviews are mostly positive. Patients note the achievement of lasting results after coagulation even in the most difficult situations. The procedure has helped more than one woman during pregnancy. After the procedure, they were allowed to have a natural birth. Some patients complained during the procedure that their eyeball hurt. This is tolerable pain that is short-term in nature.
Tatyana, 26 years old. I have suffered from myopia since my teenage years. Myopia progressed, and vision became worse and worse. The ophthalmologist at the clinic told me that myopia negatively affects the condition of the retina. As a result, even its detachment may occur. When he told me that this could ultimately lead to blindness, I realized that I couldn’t hesitate. I was offered laser coagulation, but first I underwent comprehensive diagnostics. She identified pre-tears of the retina, which can subsequently cause detachment. The day of the operation was set. I didn't prepare for it at all. Mydriatic was dripped into the eye to dilate the pupil, and then an anesthetic was dropped to relieve pain. The procedure lasted twenty minutes.
Lyudmila, 40 years old. For as long as I can remember, I have always had poor eyesight. I wore glasses for myopia for many years. After another examination, the doctor said that I have a thin and dystrophic retina. Last year I was prescribed laser photocoagulation of the retina. The manipulation was carried out under local anesthesia. The doctor used a laser to cauterize the areas where there were tears or a thin layer of the retina. The procedure was quick and painless. I didn't have any complications. That same day I was already at home. I took eye drops for several weeks after surgery. I also tried not to lift weights and watch less TV.
Anna, 28 years old. I am registered with an ophthalmologist with high myopia. When I was examined by a doctor during pregnancy, he told me that delivery could be artificial, since natural childbirth could negatively affect visual function. The ophthalmologist suggested that I strengthen my retina with a laser, but warned me that this must be done before 35 weeks. The doctor reassured me that there was nothing wrong with it. That’s right, laser coagulation turned out to be a quick and painless procedure. I was sent home that same day. For some time I continued to take the drops prescribed by the doctor and tried not to put too much strain on my eyes.
So, laser coagulation is a modern way to stop the progression of dangerous ophthalmic pathologies and restore vision. The non-contact technique eliminates the development of bleeding or the spread of an infectious process. However, it has some limitations and can cause a number of complications, about which the doctor warns the patient.
Possible complications and rehabilitation
Most often, complications after surgery develop in patients who had contraindications to undergoing it. Complications may manifest as:
- Conjunctivitis.
- Cloudiness of optical media.
- Myopia.
- Corneal edema.
Complications can also arise as a result of an unsuccessful operation. Although such cases are extremely rare in ophthalmological practice, incorrect actions by the surgeon can still lead to negative consequences:
- If the ophthalmologist applies coagulants that are too large and have intense effects on the iris, inflammation may develop. As a result of the inflammatory process, posterior synechiae are formed on the retina, which lead to pupil deformation. To eliminate this complication, surgery is used.
- After PPLC, the angle of the anterior chamber of the eye may close, which leads to surges in intraocular pressure. This complication develops due to edema of the ciliary body or choroidal detachment, which can occur as a result of strong exposure to the laser beam.
- If the retina is exposed to a laser beam that is too narrow, the lens may be damaged and cataracts may develop.
Consequences
Any medical procedure has a number of possible complications, and laser therapy is no exception. In rare cases, it can lead to the following consequences:
- corneal edema;
- decreased vision;
- glaucoma;
- cataract;
- inflammation of the conjunctiva;
- dry eye syndrome;
- repeated retinal detachment;
- the appearance of dark spots on the iris;
- deterioration of twilight vision;
- feeling blinded by bright light;
- tearfulness;
- color distortions;
- hemorrhage;
- redness of the eyes;
- inflammation of the iris.
To avoid complications, spend a few days after surgery at home if possible. To prevent infection, use antibiotic eye drops. During the entire rehabilitation period, follow your doctor’s recommendations.
Recovery period
The first time after surgery, the patient should be regularly monitored by an ophthalmologist, since complications may not arise immediately, but after 1–2 weeks.
In order not to provoke the development of complications, after the operation you should not strain, engage in intense physical activity or sports.
In addition, the patient should be aware of the following restrictions after surgery:
- Refrain from drinking alcoholic beverages for 1–2 months.
- Protect your eyes from hypothermia - try not to go outside in cold or windy weather. If such a need arises, you should try to spend as little time outside as possible.
- Avoid bending forward or standing in a vertical position.
- Protect your eyes from visual stress: refrain from driving a car, reading for long periods of time, or working at the computer.
Indications for implementation
The main goal of the technique is to create a strengthening adhesive between the retina and the choroid. The laser causes a burn ranging in size from 50 to 100 microns in duration for 0.05 - 0.1 seconds.
Laser coagulation is prescribed:
- Diabetic retinopathy. By influencing newly formed vessels, such dangerous conditions as hemophthalmos, traction detachment, and rubeosis of the iris are prevented;
- Retinopathy of prematurity (active phase). The technique stops the growth of venules and arterioles into the vitreous body, blocks the proliferation of connective tissue fibers;
- Rhegmatogenous detachment. This treatment method is effective only for fresh detachment;
- Formation of new vessels around the optic nerve head (if they occupy ? diameter). This increases the risk of multiple hemorrhages in the fundus and a sharp decrease in visual function;
- Peripheral dystrophy of the inner membrane. Laser photocoagulation carried out along the periphery stops further detachment;
- Benign and malignant tumors.
Patient preparation
Before the procedure, the patient communicates with an ophthalmologist, who gives a referral for surgery after undergoing diagnostic examinations. For a pregnant woman, it is necessary to obtain permission from the assigned antenatal clinic doctor.
This surgical intervention involves laboratory tests:
- general blood and urine tests;
- blood test for sugar levels;
- blood test for biochemistry;
- blood test for infectious diseases;
- blood clotting test;
- ECG.
Laser coagulation is performed on an outpatient basis, meaning there is no need to stay in a hospital during the rehabilitation period.
Contraindications to surgery for retinal detachment
Each type of operation has its own contraindications. Thus, vitrectomy cannot be performed if the patient is diagnosed with:
- clouding of the cornea of the eye;
- gross changes in the retina and cornea.
Extrascleral filling is not performed if:
- the vitreous body is opaque;
- ectasia (protrusion) of the sclera was diagnosed.
Laser treatment of the retina cannot be done if:
- there is severe retinal dissection;
- the media of the eye are opaque;
- there are vascular pathologies of the iris;
- Fundus hemorrhages were diagnosed.
All types of surgical interventions cannot be performed if the patient is allergic to the anesthetic or does not tolerate anesthesia well. Any inflammation in the active stage is also a contraindication to surgery.