- Indications
- Contraindications
- Operation technology
- Retinal filling
- Vitrectomy
- Pneumatic retinopexy
- Possible complications and consequences
- Recovery period
- Operation under compulsory medical insurance, price in private medical centers
- Patient reviews
- Video: operations for retinal detachment
- Operation price
Retinal detachment is the separation of the inner retinal layers from the underlying pigment epithelium and choroid. Thus, the normal functioning and light perception of the retina is disrupted. Without appropriate treatment, this condition can lead to complete or partial irreversible vision loss.
A similar diagnosis was first made by de Saint-Yves in the early 1700s, but people began to talk about the disease reliably in 1851, when Helmholtz first invented the ophthalmoscope. Unfortunately, until the 1920s. Retinal detachment always resulted in blindness until Jules Gonin, MD performed the first retinal detachment surgery. In subsequent years, there has been a rapid growth in methods and technologies for surgical treatment of retinal detachment, and modern capabilities of ophthalmic microsurgery make it possible to successfully combat the described condition through various types of surgical intervention. They will be discussed in this article.
Indications
Indications for surgical intervention for detachment depend on the etiology, duration of the disease, the patient’s condition and the presence of concomitant ophthalmological pathology.
Let's consider various clinical situations:
- Rhegmatogenous retinal detachment is undoubtedly an emergency condition requiring emergency surgical intervention. The optimal timing of surgery is 1-2 days after the onset of the disease. The sooner the integrity of the layers is restored, the greater the patient’s chances of regaining good vision. If the macula is involved in the process, treatment should begin within 24 hours. If the macula remains intact, the operation can be waited for several days, provided that strict bed rest is observed. Regardless of the patient’s age, surgical treatment should consist of two main components – closing the defect (tear) and eliminating the traction effects that led to the formation of the tear.
- Surgery for tractional retinal detachment may not be so urgent - the patient can be monitored dynamically, especially if there is no significant progression. But when the macular area is involved in the process, microsurgical intervention is often indicated. If there is a significant traction component, vitrectomy is indicated, and sometimes there is a need for episcleral filling.
- Exudative retinal detachment rarely requires emergency intervention. The exception is submacular hemorrhages, delay in which leads to irreversible changes. The type of intervention mainly depends on the etiology of the disease. For example, inflammatory conditions require topical or systemic corticosteroids, and bacterial infections require appropriate antimicrobial therapy. For patients with diabetes, an integral part of treatment is the selection of an insulin therapy regimen for glycemic control and adequate antihypertensive therapy.
Indications for surgery, as well as treatment tactics, are determined individually by the attending physician, depending on the clinical situation and the patient’s condition.
Indications for surgery
Thus, indications for this microsurgical intervention:
- retinal dystrophy and detachment;
- nearsightedness (myopia);
- formation of blood clots in blood vessels (thrombosis);
- vascular diseases suggesting further hyperplasia (as a prevention of proliferation);
- damage to the retina (retinopathy);
- retinal rupture (peripheral dystrophy);
- angiomatosis associated with vascular defects.
Advantages of the technique:
- speed of operation;
- thanks to laser exposure, the nature of the operation is low-traumatic and bloodless;
- local anesthesia is sufficient;
- the operation is easily tolerated by patients;
- short duration of the recovery period, which often does not imply a decrease in working capacity.
Contraindications
Despite the fact that interventions for detachment are often carried out for emergency reasons, there are certain limitations. Surgical treatment of detachment is contraindicated in the following situations:
- The presence of a pronounced irreversible violation of the transparency of the cornea.
- Irreversible pathological changes in the retina.
- Ectasia of the sclera and a significant decrease in the transparency of the vitreous body (relevant for episcleral filling).
- Inflammatory processes of the eyeball requiring treatment.
- General condition of the patient, severe concomitant diseases in the acute phase.
Since there are several types of operations to treat detachment, specialists always try to help the patient as much as possible and choose the optimal treatment tactics for him.
When is retinal surgery needed?
Surgery on the retina is a necessary measure in case of retinal detachment. During this pathological process, the inner layers of the retina are separated. As a result of this separation, fluid begins to accumulate in the eyeball. The extrascleral filling procedure is designed to bond the layers in order to restore vision to its functionality.
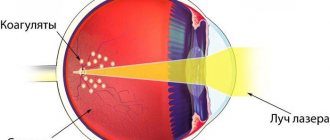
For mechanical injuries to the head and visual organs directly, which result in a rupture, the laser coagulation technique is used. This method is also popular in the treatment of peripheral retinal detachment. As a result of the intervention, breaks in the shell remain, but their edges are sealed with special coagulants. This operation is of an emergency nature when there is an urgent need to stop the progression of the disease.
Vitrectomy is performed in cases where the doctor identifies pathologies in the vitreous body. The operation is usually performed when there is extensive damage to the retinal layer, changes in the structure of the vascular system and hemorrhages in the localization of the vitreous body.
Operation technology
Regardless of the surgical method chosen, the goal is to identify and close the retinal tear or tears while minimizing iatrogenic damage. It is retinal tears that in the vast majority of cases are the cause of detachment. Also, during manipulation with the patient, it is necessary to eliminate the traction effect on the retina from the vitreous body.
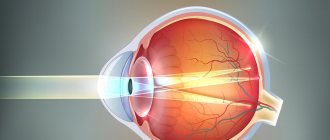
All types of operations for retinal detachment can be divided into extrascleral and endovitreal methods. Extrascleral retinal filling is performed outside the eyeball on the surface of the sclera, and the detached retina is brought closer to the underlying pigment epithelium by indenting the outer wall of the eye. Endovitreal methods involve pressing the retina from inside the eye. Sealing of defects is carried out through the formation of strong chorioretinal adhesions due to temperature or energy effects on the eye tissue in the area of the retinal tear. The most widely used methods are:
- Scleral diathermy, during which an alternating electrical discharge with a frequency of 13.56 MHz is generated. As current passes through tissue structures, the temperature increases due to the different resistance of certain cellular structures. Thanks to this temperature effect, coagulation of the required area on the retina occurs. Among the disadvantages of the method, subsequent necrosis of the scleral area can be noted.
- Transscleral cryopexy (cryotherapy) or exposure to low temperatures. Adhesive bonds formed in this way are less stable during the first week. They reach maximum strength during the second week after the intervention.
- Laser photocoagulation is a much less traumatic and safe method.
High-energy laser beams directed by a specialist to the area of the damaged retina are transformed into thermal energy. This leads to denaturation of cellular proteins and coagulation of the injured area. The manipulation is practically painless, short in duration, and most often used for retinal detachment in combination with basic surgical techniques.
Retinal filling
To carry out episcleral filling of the retina, fillings made of solid silicone or silicone sponges are used, which allows for radial, sectoral or circular extrascleral filling, depending on the number and location of breaks, and on the volume of the detached retina. The essence of the operation is as follows: a conjunctival peritomy is performed with the release of the rectus muscles. To localize all ruptures, indirect ophthalmoscopy is performed. Once the defects are identified, they are closed using transscleral cryopexy.
The filling element is prepared and sewn on the outside of the eyeball, pressing the sclera in the projection of the retinal break so that the break is completely located on the seal depression shaft. If there is a significant amount of fluid under the retina, the surgeon decides on the need to drain the subretinal space to ensure a tight fit of the detached retina on the filling without a significant increase in intraocular pressure. A circular continuous suture or interrupted sutures are placed on the conjunctival incision, which are removed 10-14 days after surgery.
Vitrectomy
Initially, vitrectomy was the procedure of choice for complicated conditions such as giant retinal tears or diabetic tractional detachments. Today, microinvasive vitrectomy is successfully used by many vitreoretinal surgeons for uncomplicated primary conditions.
The most popular is the 3-port technique using 23- and 25G instrumentation. If axial opacities are present (for example, vitreous hemorrhage), they are removed. In phakic patients, pars plana vitrectomy has a higher risk of cataract formation compared to scleral buckling, so the vitreoretinal surgeon takes necessary precautions to avoid damaging the lens. According to some experts, it is almost impossible to completely eliminate vitreoretinal traction without damaging the lens. In this regard, there is an opinion that vitrectomy is the operation of choice for retinal detachment in pseudophakic and aphakic patients. Or a combined intervention is required, when the lens is replaced before vitrectomy.
Standard transciliary vitrectomy is performed as follows. Using a vitreotome instrument, the vitreous humor is removed - a transparent gel-like substance that fills the eyeball from the inside and is the cause of the formation of a retinal tear due to its traction effect. Subretinal fluid is aspirated through the existing retinal defects, and the edges of the retinal tear are then treated with cryotherapy or laser photocoagulation to form a chorioretinal adhesion. In order to securely fix the retina, intraocular tamponade with a long-absorbable gas-air mixture or silicone oil is used. The advantage of gas is the large area of pressure on the defect compared to silicone. Also, the gas bubble gradually resolves on its own, while the silicone is removed during a second operation after 2-4 months. After vitrectomy, postoperative positioning is required for the first 10-14 days.
Vitrectomy is performed on an outpatient basis or in a hospital setting. Anesthesia can be either local (eye drops with anesthetic), regional (retrobulbar injections of anesthetic) or general, depending on the indications, the patient’s condition and the standards of ophthalmological care adopted in a particular medical institution.
Pneumatic retinopexy
Pneumoretinopexy involves intravitreal injection of an expanding gas bubble to press the retina from inside the eye in the area of the tear to the pigment epithelium and choroid. Pneumoretinopexy is extremely rarely used as a separate independent operation for retinal detachment. In the vast majority of cases of surgical treatment, laser coagulation or cryopexy is performed simultaneously in the area of ruptures.
Diagnostics
What tests should be taken for retinal detachment? Early diagnosis of retinal detachment allows timely initiation of therapy and improvement of the outcome of the disease, ultimately normalizing vision. The scope of mandatory examinations as part of the diagnostics for suspected retinal detachment includes:
- study of visual acuity with and without correction;
- performing perimetry;
- slit lamp examination;
- examination of the fundus by the attending physician (a high-diopter aspheric lens or a three-mirror Goldmann lens is used);
- IOP measurement.
You can clarify the diagnosis using other diagnostic methods, especially with concomitant diseases. The doctor will prescribe an ultrasound scan and an optical coherence tomography examination of the posterior segment of the eye, fluorescein angiography, electroretinography, CT and MRI studies, etc.
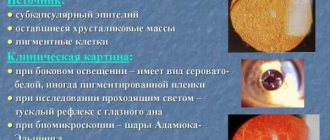
When a retinal detachment occurs, a symptom may be a raised portion of the retina. It becomes fuzzy, with a grayish tint, and its surface has the shape of a dome. When the pupil moves, it moves. The course of the vessels follows the shape of the detached surface of the retina. The boundaries of the detachment may have pigmentation (with an “old” detachment), and in the anterior chamber there is a characteristic presence of the “tobacco dust” symptom.
Possible retinal detachment is indicated by a positive Markus Gunn pupil sign. Schaefer's symptom in 70 percent of cases indicates a retinal rupture in patients who have no history of visual impairment or eye surgery. It is possible to reduce intraocular pressure by 5 mm Hg. Art. from the norm. Examination of retinal detachment shows the occurrence of breaks in quadrants. In approximately half of the cases of detachment, several breaks can be identified, mostly located within 900.
With traction retinal detachment there are no breaks. There is less subretinal fluid and it does not extend to the dentate line. The greatest height of retinal elevation is diagnosed at the site of vitreoretinal traction. Signs of the disease are characterized by the following: its mobility is noticeably reduced, and the subretinal fluid does not shift.
Changes in the visual fields during detachment appear unexpectedly and rapidly progress. The retina has a convex, smooth shape; there are no folds or tears. Sometimes the disease occurs with a high level of subretinal fluid, which can move from one part to another under the influence of gravity, depending on the position of the patient's head. In the anterior segment, signs of inflammation appear, as well as symptoms such as rubeosis, dilatation and changes in retinal vessels.
If diagnosing the factor that caused problems with the retina is difficult, it is recommended to involve other specialists in the examination, check in accordance with the expected pathology and symptoms, conduct additional laboratory tests and study the retina even more carefully.
Given that such a diagnosis may require surgery, the patient will need to undergo the following tests:
- general blood test, urine test;
- blood chemistry;
- HIV test;
- performing analysis for RW, analysis for HBS, HCV;
- ECG, chest x-ray
The sooner the doctor understands what's wrong, the sooner you can start treatment. Consequently, the doctor will cure you faster, relieving you of disturbing symptoms and eye problems and additional complications on the retina that usually arise if the patient does not solve the detachment situation or does not carry out timely diagnosis.
Possible complications and consequences
Any surgical intervention carries a risk of complications. Experts always warn patients in advance about the likelihood of an undesirable scenario, after which informed consent is signed. After surgery for retinal detachment, the following complications are possible:
- Infectious processes. The addition of a bacterial infection can cause serious endophthalmitis. For prevention, eye drops with an antibacterial drug are usually prescribed.
- Hemorrhages are possible during any operation. Before surgery, it is necessary to carefully review all regularly taken medications, paying special attention to anticoagulants and antiplatelet agents.
- Damage to the lens and development of cataracts after vitrectomy.
- Development of strabismus after episcleral filling.
- Intraocular hypertension.
- Recurrence of retinal detachment, which requires repeated surgery.
All described complications can be successfully corrected with timely diagnosis. After the operation, the specialist determines a schedule for visiting the clinic for follow-up examinations. If there is a sudden deterioration in the condition, the appearance of pain or a sharp deterioration in vision, you should visit your doctor on the same day.
Diagnosis of retinal detachment
Retinal detachment is an extremely unpleasant condition that requires immediate treatment. However, patients may not notice any signs of this abnormality for a long time.
To diagnose it in the initial stages, you need to see a doctor who will conduct an extensive diagnostic examination. Only with an integrated approach will it be possible to determine the characteristics of the course of this disease.
Typically, the diagnosis of retinal detachment includes the following:
- Perimetry is a study that determines the angle of the visual field. It allows you to determine the condition of the retina in the periphery.
- Electrophysiological study. This procedure allows you to determine how well the nerve cells of the optic nerve and retina are functioning.
- Ultrasound examination of the internal structures of the eye. Allows you to determine degenerative processes in the retina.
- Ophthalmoscopy is a procedure that allows you to assess the condition of the fundus.
Keep in mind that only a qualified specialist can diagnose retinal detachment; it is very important to undergo a comprehensive examination, thanks to which it is possible to identify multiple abnormalities in the condition of the eye.
Recovery period
Standard postoperative prescriptions include topical antibiotic eye drops (7-10 days), and corticosteroids also in the form of eye drops for a month. Constant monitoring of intraocular pressure and, if necessary, its correction are necessary. The patient is also given certain recommendations that he must adhere to for a speedy recovery and restoration of vision, the main ones of which are the following:
- Postoperative positioning to better compress the retina with a gas bubble or silicone oil in the area of the tear.
- It is forbidden to rub your eyes, apply external pressure to them, or use cosmetic makeup products for 2 weeks.
- For the first few days, it is optimal to follow a gentle regimen; subsequently, avoid intense physical activity and heavy lifting.
- It is undesirable to carry out activities associated with eye strain for a long time, including reading, watching TV, using a computer, tablet or smartphone.
- There are restrictions on visiting baths and saunas.
- When performing gas-air tamponade during vitrectomy or pneumatic retinopexy, air travel is prohibited until the gas is completely absorbed, since when atmospheric pressure changes at flight altitude, gas expands and an uncontrolled increase in intraocular pressure occurs, which can lead to the death of the optic nerve. Silicone tamponade does not have this drawback, and air travel is not prohibited.
Only strict adherence to all recommendations will help shorten rehabilitation and restore vision faster.
Vitreoretinal surgery. Vitrectomy
For many years, surgical treatment of patients with retinal detachment was limited mainly to episcleral filling operations. Methods of filling the sclera in the area of a retinal tear in combination with diathermopexy, cryopexy or laser photocoagulation of the retina give quite satisfactory results in uncomplicated cases and are widely used today.
The advent of a method such as vitrectomy, proposed by R. Machemer in 1971, made it possible to successfully treat previously incurable cases of retinal detachment with severe vitreoretinal proliferation, which include tractional retinal detachment after trauma to the organ of vision, tractional retinal detachment against the background of diabetic retinopathy and relapses of previously operated rhegmatogenous retinal detachment. With proliferative vitreoretinopathy, proliferative strands and membranes form in the vitreous body and on the surface of the retina, exerting a traction effect on the retina and causing retinal detachment.
Vitrectomy is a method of surgical treatment of retinal detachment, in which the altered vitreous body, fibrovascular cords and preretinal membranes on the surface of the retina are removed from the eye cavity. The detached retina is straightened using perfluorocarbon compounds, pressed and fixed to the underlying choroid using a laser. Upon completion of the operation, the eye cavity is filled with a special balanced saline solution or sterile air, which are replaced with the patient’s own intraocular fluid within the next 24 hours after the operation.
In some cases, to form reliable chorioretinal fusion at the sites of laser coagulation of the retina, tamponade of the eye cavity is performed with a perfluoroorganic compound in the form of liquid or gas, or silicone oil, which presses the retina to the choroid from the inside.
You can learn more about vitrectomy in our video
Install Flash Player to watch the movie.
You can learn about the removal of preretinal membranes from the surface of the retina in our video
Install Flash Player to watch the movie.
Operation under compulsory medical insurance, price in private medical centers
It is possible to perform free surgery for retinal detachment. State health care institutions have quotas for such treatment. That is, after waiting in line, the patient can undergo vitrectomy or extrascleral retinal filling free of charge. Laser coagulation is also performed free of charge as prescribed by the attending physician. In the hospital, after examination, the patient is registered for surgery. However, timely, as soon as possible, surgery for retinal detachment is the main factor in restoring vision lost as a result of the disease.
There are practically no queues at private ophthalmology clinics. The cost of the operation varies depending on the status of the clinic, the availability of this or that equipment, and the choice of surgical method. The price of laser coagulation of the retina varies between 10,000-15,000 rubles, the cost of episcleral filling is in the price range of 35-60 thousand rubles, the price of vitrectomy is 50-100 thousand rubles.
Causes
A conversation with the patient and taking an anamnesis helps a specialist understand the cause of the disease. There are several reasons for the separation of the retina and choroid, they are:
- external;
- internal;
- combined.
Depending on their predominance, the following causes of detachment are distinguished:
- traumatic;
- primary;
- secondary retinal detachment.
Traumatic retinal detachment is characterized by pain and is caused by external mechanical or chemical factors.
Primary retinal detachment occurs due to tears in the retina and penetration of fluid from the nearby vitreous into the forming cavities. The cause of the condition is not fully understood, so this type of retinal detachment is also called idiopathic.
Secondary retinal detachment is a complication of many diseases of the eye and other organs and systems (diabetes mellitus, arterial hypertension, kidney disease, etc.).
A separate cause is severe myopia (nearsightedness). Severe myopia leads to difficulties with vision and the retina, as the size of the eyeball increases, which means the retina is even more stretched.
Risk factors include work associated with intense physical exertion or intense heat on the face, as well as the presence of similar pathology or other diseases in close relatives.
Patient reviews
According to statistics, the vast majority of the operations described are successful. Patients leave positive reviews and talk about the rapid restoration of vision. Complications, if they arise, do not go unattended and are quickly stopped.
There are also negative reviews. They are associated with an insufficient degree of vision restoration, according to patients. In such cases, it is necessary to take into account the patient’s initial condition and the presence of serious diseases such as diabetes mellitus.
Thanks to the modern capabilities of eye microsurgery, hundreds of people with retinal detachment are cured, live full lives and do not lose their sight.
Rehabilitation
To quickly restore tissue during rehabilitation, you should adhere to the following recommendations:
- do not lift heavy objects weighing more than 3 kg;
- avoid colds, strengthen the immune system;
- do not stay in the sun for a long time, use sunglasses when going outside;
- Avoid temperature changes: visiting saunas, going out into the cold from a warm room.
Visual functions are restored slowly. On average, the process takes from 2 to 6 months. The visual acuity of patients who have silicone placed into the intraocular cavity may deteriorate. The negative effect goes away on its own within a week.
If the position of the retina was fixed using gas during surgery, you should avoid flying or taking the subway. Changes in atmospheric pressure can cause the gas to expand or contract, which can cause destruction of the optic nerve.
The first 48 hours - features
In the first 2 days after the operation, the body is in a state of stress. Therefore, any negative impact on the affected area can provoke the development of complications.
To avoid unpleasant consequences, you should follow several rules:
it is necessary to observe bed rest, not to overstrain the organs of vision and not to exercise physical activity;
- Do not rub or press on the operated eye or touch the mucous membranes with dirty hands;
- It is forbidden to make sudden movements of the head or tilt it to the sides;
- to pick something up from the floor, you need to squat;
- You cannot use cosmetics for 3-4 weeks.
The patient experiences discomfort for 48 hours. A person feels the false presence of a foreign body in the operated area. In some cases, the unpleasant feeling is accompanied by tingling pain. The bandage is removed from the eye the next day after the procedure. In this case, there is irritation and redness of the eyes, and swelling of the eyelids.
The first 2 weeks of the postoperative period
The speed of restoration of the visual apparatus in the postoperative period depends on the surgical technique, the type of retinal dissection and the individual characteristics of the patient. During tissue regeneration, the activity of the immune system decreases, so you need to take antibiotics for the first 2 weeks after the procedure.
The dosage and duration of use of the drugs should be prescribed by an ophthalmologist. Antimicrobial agents prevent the development of infection and accelerate tissue regeneration. Anti-inflammatory eye drops will help relieve swelling. During 2 weeks of rehabilitation, the patient must observe semi-bed rest, avoid stressful situations and physical activity. During this period, you can take sick leave so as not to put strain on your vision. The patient should be observed by an ophthalmologist and promptly inform the doctor about the occurrence of discomfort or complications.
IMPORTANT. It is necessary to protect the operated eye from contact with irritating agents: detergents, dirt, small particles.
Operation price
| code | Name | |
| 20.11 Surgical treatment of the retina and vitreous body | ||
| 2011030 | Extrascleral ballooning for retinal detachment | 26500 |
| 2011031 | Local extrascleral filling for retinal detachment | 31500 |
| 2011032 | Circular extrascleral filling for detachment | 40350 |
| 2011033 | Combined extrascleral filling for detachment | 54000 |
| 2011034 | Additional extrascleral filling in case of detachment | 24050 |
| 2011035 | Pneumoretinopexy for retinal detachment | 18500 |
| 2011036 | Removal of a silicone filling within a period of more than 6 months. after the first operation | 15550 |
| 2011037 | Removal of a silicone filling implanted in another medical institution | 20750 |
| 2011038 | Vitrectomy for uncomplicated hemophthalmia or vitreous opacities of the first category | 55000 |
| 2011039 | Vitrectomy for uncomplicated hemophthalmos or vitreous opacities of the second category | 68750 |
| 2011040 | Vitrectomy for uncomplicated hemophthalmia or vitreous opacities of the third category | 75500 |
| 2011041 | Vitrectomy for complicated conditions of the first category of complexity | 82500 |
| 2011042 | Vitrectomy for complicated conditions of the second category | 87900 |
| 2011043 | Vitrectomy for complicated conditions of the third category of complexity (20) | 105900 |
| 2011044 | Vitrectomy for complicated conditions of the highest category of complexity (30) | 120750 |
| 2011045 | Vitreoretinal surgery for complicated conditions (2-stage) of the first category of complexity | 80350 |
| 2011046 | Vitreoretinal surgery for complicated conditions (2-stage) of the second category of complexity | 110950 |
| 2011047 | Vitreoretinal surgery for complicated conditions (2-stage) of the third category | 145000 |
| 2011048 | Vitreoretinal surgery for complicated conditions (2-stage) of the highest category | 175050 |
| 2011049 | Revision of the vitreous cavity of the first category of complexity | 27000 |
| 2011050 | Revision of the vitreous cavity of the second category of complexity | 33500 |
| 2011051 | Revision of the vitreous cavity of the third category of complexity | 40500 |
| 2011052 | Unscheduled revision of the vitreal cavity | 49500 |
| 2011053 | Removal of epiretinal membranes or posterior hyaloid membrane of the first category of complexity | 30500 |
| 2011054 | Removal of epiretinal membranes or posterior hyaloid membrane of the second category of complexity | 39750 |
| 2011055 | Removal of epiretinal membranes or posterior hyaloid membrane of the third category of complexity | 48000 |
| 2011056 | Endodiathermocoagulation | 10250 |
| 2011057 | Endolaser coagulation of the retina, delimiting (one quadrant) | 12000 |
| 2011058 | Circular peripheral endolaser coagulation of the retina | 23850 |
| 2011059 | Introduction of perfluoroorganic liquids into the vitreous cavity | 15000 |
| 2011060 | Injection of liquid silicone into the vitreous cavity | 20000 |
| 2011061 | Injection of gas into the vitreous cavity | 15000 |
| 2011062 | Retinotomy and retinectomy | 12000 |
| 2011063 | Circular retinotomy or retinectomy | 24000 |
| 2011064 | Removing liquid silicone from the vitreous cavity | 15000 |
| 2011065 | Removal of perfluoroorganic liquids from the vitreous cavity | 10000 |
| 2011066 | Reconstruction of the anterior chamber | 10000 |
| 2011067 | Endodrainage of subretinal fluid | 14000 |
| 2011068 | Microinvasive revision of the anterior chamber | 19500 |
| 2011069 | Peripheral vitrectomy of 1st category of complexity | 15800 |
| 2011070 | Peripheral vitrectomy 2nd category of complexity | 25000 |
| 2011072 | Introduction of drugs of the 1st degree of complexity into the vitreous cavity | 22500 |
| 2011073 | Introduction of drugs of the 2nd degree of complexity into the vitreous cavity | 32500 |
| 2011074 | Introduction of drugs of the 3rd degree of complexity into the vitreous cavity | 65000 |
| 2011076 | Cost of the drug (Ozurdex) | 58000 |
| 2011027 | Cost of medicines (Eylea, Lucentis) | 46000 |
| 2011028 | Set of disposable consumables for vitreoretinal surgery | 48000 |
Types of surgical intervention
Many patients are interested in what operations are performed for damage to the retina. Surgery can be performed inside the eye cavity or outside. Endovitreal methods are used to eliminate extensive damage to the retina. The extrascleral technique involves fixing the retina by applying pressure to the outer wall of the eye.
Vitrectomy
Vitrectomy is the complete or partial removal of a gel-like concentrate from the cavity of the eyeball. The technique allows easy access to the retina. The operation is indicated for epiretinal membrane, extensive ruptures, and tissue transplantation. After the procedure is completed, the vitreous is replaced with saline, silicone or gas. The duration of the procedure is from 1 to 2 hours. Patients with gas are not recommended to sleep on their backs, so as not to cause the substance to enter the anterior chamber of the eye.
IMPORTANT. An air bubble is often placed in front of the retina to help fix the tissue in its normal position.
Laser coagulation
Laser surgery is based on the action of thermal radiation. During the procedure, the ruptures and detachments of the inner membrane are cauterized. Laser coagulation can be carried out regardless of the pathological process - the method is equally effective in cases of damage to the peripheral and central zones of the reticular layer. The technique helps prevent tissue degeneration. The duration of the procedure is 20-40 minutes. After surgery, it is not recommended to fall asleep on your back to avoid increased intraocular pressure.
Extrascleral filling
During extrascleral filling, the distance between the retina and the pigment layer, which was formed during the process of delamination of the membranes, decreases. The surgical technique allows preserving the vitreous body compared to vitrectomy.
ARTICLES ON THE TOPIC:
- A high-tech method of vision preservation - vitrectomy, its consequences and...
- How is surgery performed for a macular hole in the retina and features of the period...
- How is surgery performed for retinal detachment: performance and recommendations for...
The operation is carried out according to the following algorithm:
The area of retinal detachment is determined. The filling is made from silicone. It puts pressure on the sclera, thereby preventing rupture of soft tissue. The filling helps the fluid accumulated under the retina to dissolve in a short time.
- The surgeon cuts the conjunctiva, places the filling in the desired position and sews it to the tissue.
- The accumulated fluid under the retina is evacuated if necessary. For additional fixation of the retina, the surgeon may inject gas into the intraocular cavity.
- The incision is sutured.
The duration of the procedure is 40-90 minutes. Visual function is restored within 2-3 months. However, complete rehabilitation does not occur. The degree of restoration of the functional activity of the organ of vision depends on which area of the retina is detached. The severity of the pathological process plays an important role. The postoperative period after applying a filling increases in old age.
Cryocoagulation
Cryocoagulation helps prevent the detachment from spreading to the macula. Cryopexy prevents divergence of the edges of the retinal tear. The operation is performed on an outpatient basis with local anesthesia. A tube is inserted into the eye, delivering a stream of liquid nitrogen. The substance freezes the tissue, pressing the retina to the vascular layer. As a result, the neurosensory membrane fuses with the choriocapillaris. The duration of the procedure is no more than 40 minutes. The procedure does not impose restrictions on lifestyle during the rehabilitation period.
Extrascleral ballooning
This type of surgery is performed for retinal detachment, which is not accompanied by the development of complications.
Extrascleral ballooning cannot restore extensive tissue damage and does not help with hemorrhages in the intraocular cavity.
Patients wonder how surgery works. During the procedure, a special balloon is inserted into the organ of vision through a catheter. It is left inside the vitreous. After installation, liquid begins to flow into the cylinder, causing the device to increase in size. In this state, the instrument creates pressure on the sclera, which allows the retina to be fixed in its normal position. To strengthen the retina after removing the catheter, the doctor may perform laser coagulation.
On the 5-7th day of the postoperative period, the balloon is removed, because during this time the tissues are completely regenerated. The effectiveness of extrascleral treatment is 98%. The duration of the procedure is about 2 hours.