Lacrimal gland cancer is a malignant neoplasm that grows in the epithelium of this gland and is prone to the rapid spread of metastases.
Causes of the disease
A malignant tumor of the lacrimal gland is extremely rare in modern oncology, but is considered one of the most life-threatening diseases. It most often progresses specifically in female bodies at 50–60 years of age, and is accompanied by a large-scale spread of metastases already at an early stage. It is almost impossible to overcome the disease, and the clinical outcome is not the most favorable for the patient.
The following types of disease are distinguished: pleomorphic adenocarcinoma, adenoid cystic, mucoepidermoid, squamous cell, the classification of which predominates according to morphological characteristics.
If we talk about the pathogenesis of a tumor of the lacrimal gland, then it grows rapidly, and when it reaches a certain size, it closes the lumen of the gland, provoking dysfunction of the entire body. As a rule, death is inevitable, but the patient manages to live another five years only if the diagnosis is made in a timely manner. A malignant tumor of the lacrimal gland has four traditional stages, but the first is characterized by the rapid spread of metastases and damage to neighboring tissues, vessels and lymph nodes.
The causes of this disease have not been clarified, but doctors are confident that the cause of the pathological process is a genetic predisposition and hereditary factor. In addition, the age of the typical patient and the prevalence of chronic vision problems play an important role.
Symptoms and course of the disease
Lacrimal gland cancer manifests itself in the 4th–6th decade of life. The history of the disease is shorter than with a benign tumor.
Pain is a sign of malignancy, but can also be due to inflammatory processes. Pleomorphic adenocarcinoma (malignant mixed cell tumor) is represented by three main clinical variants:
- After incomplete removal of a benign pleomorphic adenoma, subsequent one or more relapses over several years and eventually malignant transformation.
- Long-standing exophthalmos (or enlargement of the upper eyelid), which suddenly begins to increase.
- Without a prior history of pleomorphic adenoma as a rapidly growing formation of the lacrimal gland (usually over several months).
Signs of lacrimal gland cancer:
- A neoplasm in the area of the lacrimal gland, displacing the eyeball.
- Posterior extension involving the superior orbital fissure can lead to congestion in the conjunctiva and episclera and ophthalmoplegia.
- Limitation of upward and outward eye movements (common symptom).
- Hypoesthesia of the lacrimal nerve innervation zone.
- Swelling of the optic disc and choroidal folds.
Treatment of the disease
Treatment of lacrimal gland cancer is a complex task. Along with the radical point of view, whose supporters require mandatory exenteration of the orbit, there is an opinion about the possibility of organ-preserving treatment, combining local excision of the tumor with a block of adjacent healthy tissue and postoperative external irradiation of the orbit. The choice of a particular treatment method depends on the size of the tumor and its prevalence. If a violation of the integrity of the orbital bones is detected preoperatively, surgical treatment, including exenteration, is contraindicated.
- Radical removal can be performed in the form of orbital exentaration or midfacial resection. Unfortunately, it is rarely possible to completely remove the tumor tissue, which determines a poor life prognosis.
- Radiotherapy combined with local excision can prolong life and reduce pain.
The prognosis for life and vision is poor, since the tumor is not only prone to recurrence with invasion into the cranial cavity, but also to metastasis to the lungs, spine or regional lymph nodes. The timing of metastases varies from 1-2 to 20 years.
Benign tumors of the lacrimal glands
Pleomorphic adenoma is a mixed epithelial tumor of the lacrimal gland. Accounts for 50% of the total number of neoplasms of this organ. Women are affected more often than men. The age of patients at the time of diagnosis can range from 17 to 70 years, the largest number of cases of the disease (more than 70%) occur in 20-30 years. Arises from epithelial duct cells. Some experts suggest that the source of the tumor is abnormal embryonic cells.
It is a node with a lobular structure, covered with a capsule. The tissue of the lacrimal gland tumor on the section is pink with a grayish tint. Consists of two tissue components: epithelial and mesenchymal. Epithelial cells form chondro- and mucus-like foci located in a heterogeneous stroma. The initial stages are characterized by very slow progression; the period of time from the appearance of the lacrimal gland tumor to the first visit to the doctor can range from 10 to 20 years or more. The average time interval between the onset of the first symptoms and seeking medical help is about 7 years.
For some time, the tumor of the lacrimal gland exists without causing any particular inconvenience to the patient, then its growth accelerates. Inflammatory swelling appears in the eyelid area. Due to the pressure of the growing node, exophthalmos and an inward and downward displacement of the eye develop. The upper outer part of the orbit becomes thinner. Eye mobility is limited. In some cases, a tumor of the lacrimal gland can reach gigantic sizes and destroy the wall of the orbit. Upon palpation of the upper eyelid, a fixed, painless, dense, smooth node is determined.
A survey X-ray of the orbit reveals an increase in the size of the orbit due to displacement and thinning of its upper outer part. Ultrasound of the eye indicates the presence of a dense node surrounded by a capsule. CT scan of the eye allows you to more clearly visualize the boundaries of the tumor, assess the continuity of the capsule and the condition of the bone structures of the orbit. Surgical treatment involves excision of the lacrimal gland tumor along with the capsule. The prognosis is usually favorable, but patients must remain under clinical supervision throughout their lives. Relapses can occur even several decades after removal of the primary node. In more than half of patients, signs of malignancy are detected already at the first relapse. The shorter the period of remission, the greater the likelihood of malignancy of a recurrent tumor.
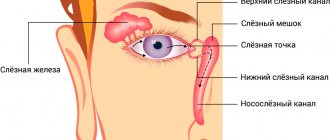
Diagnosis of the disease
It is impossible to make a final diagnosis solely after examination by an ophthalmologist, since this clinical picture requires more detailed diagnosis. Its basis is histological examination, which is shown in all clinical pictures.
However, a complex of instrumental studies is also required, represented by the following procedures:
- X-rays allow you to detect areas of bone destruction and visualize the focus of pathology, its size and shape;
- computed tomography carefully examines the pathogenic neoplasm, determines the unevenness of its boundaries and the contours of the bone wall of the orbit;
- Ultrasound determines the density and consistency of the tumor, as well as the presence of its shadow;
- a radioscintigram confirms the presence of a malignant tumor in the lacrimal gland;
- remote thermography;
- a biopsy allows a histological diagnosis to be made.
Additionally, it is recommended to examine the nervous system, since complications can extend specifically to it. When all the results are ready, the doctor gathers a consultation and makes a final diagnosis, after which he selects an adequate treatment regimen.
Prices
| Disease | Approximate price, $ |
| Prices for strabismus treatment | 14 190 |
| Prices for treatment of eye melanoma | 8 000 |
| Prices for treatment of keratoconus | 27 610 — 59 950 |
| Prices for cataract treatment | 8 690 |
| Prices for glaucoma treatment | 7 260 — 8 360 |
| Disease | Approximate price, $ |
| Prices for thyroid cancer screening | 3 850 — 5 740 |
| Prices for examination and treatment for testicular cancer | 3 730 — 39 940 |
| Prices for examinations for stomach cancer | 5 730 |
| Prices for diagnosing esophageal cancer | 14 380 — 18 120 |
| Prices for diagnosis and treatment of ovarian cancer | 5 270 — 5 570 |
| Prices for diagnosing gastrointestinal cancer | 4 700 — 6 200 |
| Prices for breast cancer diagnostics | 650 — 5 820 |
| Prices for diagnosis and treatment of myeloblastic leukemia | 9 600 — 173 000 |
| Prices for treatment of Vater's nipple cancer | 81 600 — 84 620 |
| Prices for treatment of colorectal cancer | 66 990 — 75 790 |
| Prices for treatment of pancreatic cancer | 53 890 — 72 590 |
| Prices for treatment of esophageal cancer | 61 010 — 81 010 |
| Prices for liver cancer treatment | 55 960 — 114 060 |
| Prices for treatment of gallbladder cancer | 7 920 — 26 820 |
| Prices for treatment of stomach cancer | 58 820 |
| Prices for diagnosis and treatment of myelodysplastic syndrome | 9 250 — 29 450 |
| Prices for leukemia treatment | 271 400 — 324 000 |
| Prices for thymoma treatment | 34 530 |
| Prices for lung cancer treatment | 35 600 — 39 700 |
| Prices for melanoma treatment | 32 620 — 57 620 |
| Prices for treatment of basal cell carcinoma | 7 700 — 8 800 |
| Prices for the treatment of malignant skin tumors | 4 420 — 5 420 |
| Prices for treatment of eye melanoma | 8 000 |
| Prices for craniotomy | 43 490 — 44 090 |
| Prices for thyroid cancer treatment | 64 020 — 72 770 |
| Prices for treatment of bone and soft tissue cancer | 61 340 — 72 590 |
| Prices for treatment of laryngeal cancer | 6 170 — 77 000 |
| Testicular cancer treatment prices | 15 410 |
| Bladder cancer treatment prices | 21 280 — 59 930 |
| Prices for cervical cancer treatment | 12 650 — 26 610 |
| Prices for treatment of uterine cancer | 27 550 — 29 110 |
| Prices for treatment of ovarian cancer | 32 140 — 34 340 |
| Prices for treatment of colon cancer | 45 330 |
| Prices for lymphoma treatment | 11 650 — 135 860 |
| Prices for kidney cancer treatment | 28 720 — 32 720 |
| Prices for breast reconstruction after cancer treatment | 41 130 — 59 740 |
| Prices for breast cancer treatment | 26 860 — 28 900 |
| Prices for prostate cancer treatment | 23 490 — 66 010 |
ADENOID CYSTIC CARCINOMA OF THE LACRIMAL GLAND: CASE HISTORY
Published in 2020, Issue January 2020, MEDICAL SCIENCES | No comments yet
Valkanov S.¹, Valkanov P.¹, Slaveykov K.², Trifonova K.², Popkharitov A.³, Tanev I.4, Petrov B.¹
1 Neurosurgery Clinic, 2 Ophthalmology Clinic, 3 Surgical Clinic, Stoyan Kirkovich University Hospital, Stara Zagora, Bulgaria, 4 Ophthalmology Clinic, Aleksandrovska University Hospital, Sofia, Bulgaria
ADENOID CYSTIC CARCINOMA OF THE LACRIMAL GLAND: CASE HISTORY
annotation
Adenoid cystic carcinoma is a rare form of malignant tumor of epithelial origin. It is the most common primary malignant tumor of the lacrimal gland, but accounts for less than 4% of all gland neoplasms. There is still controversy regarding the optimal treatment, mainly regarding the surgical approach and the extent of radical tissue removal. The presented case shows solutions to the issues of diagnosis and treatment of adenoid cystic carcinoma, and also discusses some of the most common errors.
Key words: adenoid cystic carcinoma, lacrimal gland, therapeutic approach.
Valkanov St. ¹, Valkanov P. ¹, Slaveykov K. ², Trifonova K. ², Popharitov A. ³, Tanev I. 4 , Petrov B. ¹
¹ Neurosurgery clinic, ² Ophthalmology clinic, ³ Surgery clinic, University hospital „Prof. Stoyan Kirkovich, MD”, Stara Zagora, Bulgaria, 4Ophthalmology clinic, University hospital “Aleksandrovska”, Sofia, Bulgaria
ADENOID CYSTIC CARCINOMA OF THE LACRIMAL GLAND – A CASE REPORT
Abstract
Adenoid cystic carcinoma is a rare form of malignant neoplasm with epithelial origin. It is the most common primary malignat neoplasm of the lacrimal gland, yet it is responsible for less than 4% of all neoplasms of the gland. There are still controversies about the optimal treatment, mainly concerning the surgical approach and the degree of radical removal of tissues. The presented case is a good example for the diagnostic and treatment dilemmas when dealing with adnoid cystic carcinoma of the lacrimal gland, as well as some of the most common mistakes made.
Keywords: adenoid cystic carcinoma, lacrimal gland, therapeutic approach
Adenoid cystic carcinoma (ACC) of the lacrimal gland is a rare form of malignant neoplasm with epithelial origin (1). It is the most common primary malignat neoplasm of the lacrimal gland, yet it is responsible for less than 4% of all neoplasms of the gland (2-4). Most individuals are diagnosed with the disease in the fourth through sixth decade of life (5), and rarely during childhood (6, 7). There are still controversies about the optimal approach for treating the neoplasm. Some author recommend a more conservative approach during surgery, followed by radiation or proton therapy (8). Others support radical evisceration with or without removal of surrounding bone structures as the most appropriate method of treatment (9). In general patients with ACC of the lacrimal gland have poor prognosis, which makes the choice of teurapethic approac difficult (10).
The presented case is a good example for the diagnostic and treatment dilemmas when dealing with adnoid cystic carcinoma of the lacrimal gland.
CASE REPORT: We present a case of a 79 yo female patient, operated on in another hospital in 2010 for a soft tissue formation in the left orbit. No material was taken for histological examination. Four moths after surgery, the patient enters the neurosurgery clinic in University hospital Stara Zagora with complaints of constant pain and swelling in the same area.
Fig.1 Transsupercilliary superlateroorbitotomy
Pic 1. No. 2008, 2009 from 06/28/2010 – adenoid cystic carcinoma
The orbit computer tomography (CT) establishes a soft tissue-equivelent tumor formation in the upper lateral part of the left orbit, extending to lateral orbital structures. Upon admission the patient and no focal neurological symptoms and no visual impairement. A left-sided osteoplastic frontoorbital craniotomy by V. Busarski was preformed (Fig.1), after which the tumor formation was extirpated en block under optic magnification. The formation did not affect the surrounding soft tissues and bone structures. The upper lateral orbital rim waas restored. Histology showed adenoid cystic carcinoma (Pic. 1).
Fig.2 Tumor formation
Fig.3 Preoperative CT
Fig.4 A- Extracranial part of the neoplasm; B 1- bulbus oculi, 2- previous craniotomy, 3 – processus frontalis; C- Dissection of the intra-orbital part of the tumor formation; D – Extirpated intracranial portion of the tumor formation.
Fig.5 Postoperative CT
Pic 2. No. 1903, 1904 from 10.30.2014 – recurrence of adenoid cystic carcinoma
Postoperative radio- and chemotherapy was recommended to the patient, which she did not comply with. In September 2014 the patient reenters the clinic with a relapse of the tumor formation. The size of the formation was 2/3 sm, with hard elastic consistency, adherent to underlying structures, slightly painful on palpation with ulcerations of the overlaying skin (Fig. 2). CT of orbits confirms reccurance of a tumor formation on the left periorbitally, covering and lysing the squama of the temporal os, lateral retroorbital space, lateral rectus muscle and processus forntalis of os zygomaticum (Fig. 3). From the ophthalmologic status: Visus of the right eye is 0.7, visus of the left eye is perceptio et projection lucis certa. The right eye is pseudophacic with an intraocular lens. The left eye has a corneal adherence to the iris at 6 o'clock on 3 mm from the limbus. Anteriro chamber is uneven, the pupil is streched torward 6 o'clock and the lens is completely opaque. The patient was taken for reoperation, the extracranial part of the tumor formation was dissected (Fig. 4A) and removed untill healthy tissue was reached. Processus frontalis os zygomaticum was lysed to missing (Fig. 4B). The intraorbital part of the tumor formation was disseted and extirpated en block (Fig. 4 C, D) and usures were found on the lateral wall of the orbit (Fig. 5). Histology confirmed recurrence of adenoid cystic carcinoma (Pic. 2).
Adenoid cystic carcinoma is an unusual tumor. Despite its rarity it is the second most common epithelial neoplasm of the lacrimal gland, after benign pleomorphal adenoma and it is the most common malignant neoplasm of the gland (11).
Reoccurance is common until the fourth year after excision. The tumor usually spread via local invasion, and less likely with distant metastasis. In accordance with the dissemination methods in recent years there is a tendency for radical surgery with removal of the neighboring orbital bones (radical orbitectomy) in combination with radio- and cehmotherapy (2-5; +12-+18). Even with this radical approach some author discuss poor prognosis for patients with the disease (13; 14).
The presented case is an example for the diagnostic and treatment dilemma when facing adenoid cystic carcinoma of the lacrimal gland. In our case, the patient had a soft lesion in the region of the upper lateral orbital rim, which was treated without the required preoperative diagnostics and preparations. A CT was appropriate, which even then would have shown that the tumor formation had an intraorbital part. The surgical approach would have been different – frontoorbital craniotomy would have provided an easier access to the formation and extripation en block. Another error was the lack of histological verification of the lesion. During the second hospitalization of the patient, in our hospital, a more appropriate action would have been evisceration. The relatevely early diagnosis of the neoplasm, the macroscopic characteristics (capsulated), the lack of histological verification of the previous incision, as well as the completely preserved functions of the eye were argument for the lack of evisceration. There are some author who prefer a more conservative approach during treatment of ACC of the lacrimal gland (8). The refusal for radio- and chemotherapy from the patient after dehspitalization also supports the reoccurance.
Adenoid cystic carcinoma is the most common malignant neoplasm of the lacrimal gland. It spreads usually by local invasion and distant metastasis. Surgical removal, followed by radio- and chemotherapy is the only right approach to treatment of the disease. The surgical intervention should be preceded by serious preoperative diagnostics. Appropriate operative access must be chosen, which allows total extripation, and when needed evisceration with removal of the affected bone structures.
References
- Font RL, Smith SL, Bryan RG. Malignant epithelial tumors of the lacrimal gland: a clinicopathologic study of 21 cases. Arch Ophthalmol 1998;116:613–6
- Shields JA Epithelial tumors of the lacrimal gland: primary carcinomas. Shields JAed.Diagnosis and Management of Orbital Tumors. Philadelphia, Pa WB Saunders Co1989;267- 272.
- Shields JABakewell BAugsburger JJFlanagan JC Classification and incidence of space-occupying lesions of the orbit: a survey of 645 biopsies. Arch Ophthalmol. 1984;1021606-1611.
- Shields CLShields JAEagle RCRathmell JP Clinicopathologic review of 142 cases of lacrimal gland lesions. Ophthalmology. 1989;96431-435.
- Font RLGamel JW Adenoid cystic carcinoma of the lacrimal gland: a clinicopathologic study of 79 cases. Nicholson DHed. Ocular Pathology Update. New York, NY Masson Publishing USA1980;277-283.
- Dagher GAnderson RLOssoinig KCBaker JD Adenoid cystic carcinoma of the lacrimal gland in a child. Arch Ophthalmol. 1980;981098-1100.
- Tellado MVMclean IWSpecht CSVarga J Adenoid cystic carcinomas of the lacrimal gland in childhood and adolescence. Ophthalmology. 1997;1041622-1625.
- Asikin Natanegara IAA, Koornneef L, Veenhof K, et al. An alternative approach for the management of adenocystic carcinoma of the lacrimal gland. Orbit 1990;9:101–105.
- Marsh JL, Wise DM, Smith M, Schwartz H. Lacrimal gland adenoid cystic carcinoma: intracranial and extracranial en bloc resection. Plast Reconstr Surg 1981;68:577–585.
- Esmaeli B, Ahmadi MA, Youssef A, et al. Outcomes in patients with adenoid cystic carcinoma of the lacrimal gland. Ophthalmic Plast Reconstr Surg 2004;20:22–26.
- Vasantha Thavaraj, M.R. Sridhar, A. SethP and L.S. Arya. Adenoid Cystic Carcinoma of the Lacrimal Gland. Indian Joumal of Pediatrics, Volume 70—September, 2003, p 751 – 753.
- Font RLGamel JW Epithelial tumors of the lacrimal gland: an analysis of 265 cases. Jakobiec FAed.Ocular and Adnexal Tumors. Birmingham, Ala Aesculapius1978;787-805.
- Henderson JW Adenoid cystic carcinoma of the lacrimal gland: is there a cure? Trans Am Ophthalmol Soc. 1987;85312-334.
- Jakobiec FA Discussion of Henderson JW. Adenoid cystic carcinoma of the lacrimal gland: is there a cure? Trans Am Ophthalmol Soc. 1987;85314-337.
- Lee DACampbell RJWaller RRIlstrup DM A clinicopathologic study of primary adenoid cystic carcinoma of the lacrimal gland. 1985;9212-34.
- Byers RMBerkeley RGLuna MHesse R Combined therapeutic approach to malignant lacrimal gland tumors. Am J Ophthalmol. 1975;7953-55.
- Wright JEStewart WBKrohel GB Clinical presentation and management of lacrimal gland tumors. Br J Ophthalmol. 1979;63600-606.
- Gamel JWFont RL Adenoid cystic carcinoma of the lacrimal gland: the clinical significance of a basaloid histologic pattern. Hum Pathol. 1982;13219-225.