Secondary glaucoma is a collective name for a number of eye lesions, most often related to the acquired form, which are formed against the background of a gradual increase in IOP (intraocular pressure). In fact, secondary glaucoma is a complication or consequence of previous eye injuries or ophthalmological pathologies. Both children and adults are susceptible to it.
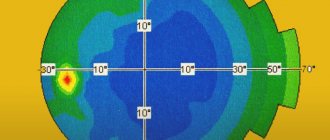
Increased pressure inside the eyes with glaucoma
What is glaucoma
Glaucoma is a broad group of eye diseases characterized by constant or periodic increased intraocular pressure, atrophy of the optic nerve with the subsequent development of typical visual field defects and decreased visual acuity.
This disease occupies a leading place among the causes of irreparable blindness. Vision in glaucoma decreases gradually, and therefore the patient most often notices changes in visual functions already in the advanced stage of the disease. In this case, vision decreases, up to the onset of blindness, which is irreversible, as the optic nerve dies. It is no longer possible to restore sight to a patient who has gone blind for this reason!
Early diagnosis and treatment of this disease can compensate for the course of glaucoma, prevent damage to the optic nerve and associated vision loss. Therefore, it is very important to be regularly examined by competent specialists.
Primary open-angle glaucoma usually develops due to progressive impairment of the outflow of intraocular pressure. As a rule, the cause is age-related changes in the angle of the anterior chamber of the eye. IOP can also rise due to too active synthesis of aqueous humor, which is observed in people with myopia.
Angle-closure glaucoma occurs due to a sharp overlap of the anterior chamber angle by the root of the iris. What most often happens to people with farsightedness. Their eyeball is small, the anterior chamber is small, and the lens is large. These anatomical features contribute to the development of the disease.
The following factors can trigger an attack of angle-closure glaucoma:
- drinking large amounts of liquid at one time;
- long stay in a dark room;
- frequent work with a tilted head;
- instillation of mydriatics into the eye - drugs that dilate the pupil.
It should be noted that during an appointment with an ophthalmologist, a person often receives drops to help dilate the pupil and clearly see the fundus of the eye. In people with high intraocular pressure, these drugs can cause an attack of angle-closure glaucoma. That is why it is necessary to measure IOP before using mydriatics.
Treatment methods
Drops serve as first aid during attacks of exacerbation of the disease.
To determine the provision of assistance to the patient, it is important to determine the root cause of the pathological condition and eliminate it so that there is no relapse. For this purpose, in case of phacomorphic glaucoma, treatment is aimed at stopping an acute attack: 1% Pilocarpine is administered intraorbitally every 15 minutes for 1 hour, and then once an hour until the intraocular pressure decreases. 0.5% Timolol is instilled 2 times a day. 20% Mannitol and 1% Furosemide solution are administered intravenously. After normalization of pressure, surgical treatment is carried out in order to normalize the size of the lens and return the anterior chamber angle to normal.
Therapy for pharmacolytic glaucoma is only surgical. During the operation, all pathological layers are removed to restore normal outflow of ocular fluid. The cause is untreated cataracts, so surgery involves removing them. With pharmacotypic glaucoma, there is no other way out than removing the dislocated lens, which has ceased to be viable.
Causes of glaucoma development
Glaucoma can occur at any age and mainly affects people over 40 years of age. But this disease can also affect young people (juvenile glaucoma) and even newborns (congenital glaucoma), since most often it develops in those people whose parents also suffered from this disease. Glaucoma can be an occupational disease, develop due to age-related changes, injuries or concomitant diseases.
Risk factors include:
- age over 50 years;
- family history - the presence of glaucoma in close relatives;
- wounds, eye contusions;
- chronic ophthalmological diseases such as cataracts, high myopia, iridocyclitis, chorioretinitis;
- the presence of hypertension, hypotension, diabetes mellitus, obesity;
- sclerotic changes in blood vessels or deposition of atherosclerotic plaques in them;
- cervical osteochondrosis, leading to disruption of the innervation of the eyeballs.
Causes
The sources leading to an increase in pressure inside the eyes are varied:
- infectious and inflammatory pathologies of the membranes of the eye or their consequences (keratitis, uveitis, and so on);
- change in lens parameters;
- trauma of any origin;
- retinal vein blockage;
- dystrophic changes in the eye system;
- poor blood supply to the retina, during which the process of neovascularization of the iris occurs, that is, the appearance of new vessels.
Symptoms of glaucoma
Glaucoma is most often asymptomatic; deviations from the norm are often detected by chance, during an examination or visit to an ophthalmologist for some other reason.
Over time, a person begins to navigate much worse in space due to a narrowing field of vision. In the later stages of the disease, it may seem to him that he is looking at the world around him as if through a spyglass. Twilight vision is also greatly affected. The patient practically loses the ability to see something in the dark.
With angle-closure glaucoma, a person experiences severe pain in the eye, which soon spreads to the entire half of the head. The patient's body temperature rises, chills, nausea and even vomiting appear. When palpated, the eye turns out to be very hard, reminiscent of stone. All symptoms appear abruptly and develop rapidly.
Some nonspecific symptoms may indicate the presence of the disease:
- mild pain, feeling of heaviness in the eyes;
- rapid visual fatigue;
- deterioration of visual acuity at dusk;
- double vision;
- the appearance of rainbow circles when looking at the light;
- feeling of increased moisture in the eyes.
Stages of glaucoma
According to the severity of the process, 4 stages of glaucoma are distinguished:
- I initial stage - the early stage is characterized by periodic surges in intraocular pressure, causing sharp dilation of the pupils and headaches.
- Stage II of advanced glaucoma - advanced glaucoma is manifested by a significant narrowing of the visual field on the nasal side or the formation of a large arcuate scotoma. Increased intraocular pressure provokes pain in the affected eye; sometimes the enlargement of the eyeball is even visible visually. Visual acuity decreases. At this stage, it is most often impossible to do without surgery.
- Stage III of advanced glaucoma - at this stage, glaucoma is accompanied by a concentric narrowing of the visual field and the complete loss of its large areas, that is, a significant increase in the blind spot. Sharply increased intraocular pressure leads to other pathologies: retinal detachment, clouding of the lens, and the formation of hemorrhages. Drug therapy and diet for the third stage of glaucoma serve only as an aid; the main method of treatment in this case is surgery.
- IV terminal stage of glaucoma - complete loss of central vision and complete loss of objective vision. With terminal glaucoma, there is a serious increase in intraocular pressure, it is accompanied by severe headaches and eye pain, enlargement and clouding of the eyeball - buphthalmos or bull's eye.
Depending on age, glaucoma is divided into congenital (in children under 3 years of age), infantile (in children from 3 to 10 years of age), juvenile (in persons aged from 11 to 35 years of age) and glaucoma adults (in persons over 35 years of age). All forms are acquired, except congenital.
Definition of disease
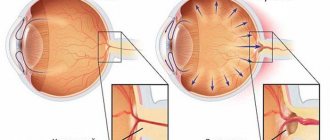
Glaucoma is a serious ophthalmological disease, the main symptoms of which are a strong increase in intraocular pressure, retinal degeneration and complete blindness. It develops as a complication of various ophthalmological diseases or injuries of the eyeball. Characteristic signs of secondary glaucoma are excessive formation of intraocular fluid or disruption of its outflow.
If left untreated, secondary glaucoma leads to retinal degeneration and complete blindness.
Glaucoma treatment
Is glaucoma curable?
If there is a suspicion that a person has glaucoma, then it is possible to determine the stage of development of the disease during an examination by a specialist. The doctor will decide how to treat the patient based on the diagnostic data obtained. At the initial stage of development of the disease, it is possible to treat glaucoma without surgery, the so-called conservative method. Therapy is carried out using special eye drops that lower the pressure inside the eye, improve the outflow of fluid passing through the organ, or reduce its secretion.
A positive effect from such treatment is possible with the open-angle type of the disease, when there are no changes in the structure of the eyes. If a patient is diagnosed with angle-closure glaucoma, then medications are practically useless. And to eliminate problems, surgical treatment methods are already used. With their help, angle-closure glaucoma is curable both at the initial stage of the disease and at later stages.
Surgery for glaucoma
Surgery is indicated for open-angle glaucoma that responds poorly to prescribed medications. In case of an acute attack of angle-closure glaucoma, surgery is necessary if
if intraocular pressure cannot be normalized with drug treatment.
- Laser methods of treating glaucoma are considered the most modern and least traumatic operations:
1. Laser iridotomy is the removal of glaucoma without surgery. This type of treatment is highly effective, easily tolerated and safe. Removing glaucoma using a laser guarantees a complete cure for the disease. Laser iridotomy is performed without opening the eyeball and is a microsurgical intervention. The risk of complications is minimal.
2. Trabeculoplasty - the surface of the diaphragm is burned with a laser, which increases its tension and, as a result, permeability. As a result, more fluid swells from the anterior chamber, and the pressure decreases.
- Cryodestruction: the essence is similar to the previous method, but the effect is carried out not by a laser, but by cold, and the object is not the iris, but the sclera. It is exposed to cold, applying applications at several points at once. The operation is contraindicated for terminal stages of glaucoma, unsuccessful surgical interventions, or a history of pain. Cryodestruction is not as safe and more often causes complications. It is used if laser correction is contraindicated for a patient for some reason.
Prevention of glaucoma
Preventative measures will help reduce the damage that high blood pressure causes to the visual system, thereby preventing optic atrophy and blindness.
1. Do not overexert yourself - limit both physical and psycho-emotional stress. 2. Do not keep your head tilted - it is harmful for patients with glaucoma to engage in activities that require prolonged tilting of the head down. This applies to reading, drawing, drawing, knitting, embroidery and others. It is necessary to maintain a level head position when working at the computer or watching TV. 3. Set up the right lighting - it is dangerous for people with glaucoma to work in poor lighting. It is important to make it bright so as not to strain your eyes. 4. Give up bad habits, as smoking negatively affects the blood supply to the whole body. The transport of oxygen and nutrients to all elements of the eyeball is disrupted. 5. Choose loose clothing that does not interfere with blood circulation in the neck and head. 6. Avoid visual fatigue - it is important to take breaks while working at the computer, reading and watching movies. It is recommended to set aside 15-20 minutes every hour for rest. At this time, you need to really rest, and not change one strenuous activity to another. 7. Eat right - to prevent glaucoma, you need to include raw vegetables, fish, fruits in your diet, while reducing the amount of animal fats and sugar. 8. Consume moderate amounts of water and other drinks. You should not drink more than one glass of any liquid at a time. To be on the safe side, you can check your reaction to coffee or green tea: measure your blood pressure before and after. 9. Get proper rest, get a good night’s sleep, it is advisable not to stay up late, take a walk in the fresh air in the evening. You need to sleep on comfortable pillows. After waking up, it is recommended to do a warm-up without getting out of bed. 10. Do not refuse drug treatment. 11. Avoid sudden changes in lighting—changes in lighting intensity are a strong strain on the eyes, so before going to the cinema, for example, you need to use drops that prevent pupil dilation. 12. Constantly monitor your condition. Even with stable intraocular pressure, you should visit your doctor at least four times a year.
These measures will help avoid not only glaucoma, but also other diseases of the visual system. Prevention is recommended for everyone, since glaucoma can occur even in a completely healthy person. At Lensmaster you can undergo a free vision diagnostic by making an appointment through the website.
Types and forms
Let's look at the main types and forms of this disease.
Closed and open angle
Secondary glaucoma is divided into closed-angle and open-angle.
- Eye pressure depends on an even balance between the entry and exit of internal fluid. The outflow of fluid inside the eye occurs through the drainage system (anterior chamber angle). The output is carried out without delay when the angle between the iris and cornea is thirty degrees. If for some reason it decreases, drainage worsens, pressure increases, and secondary angle-closure glaucoma occurs.
- With degenerative changes in drainage structures, there is also a decrease in the output of internal fluid. Such pathologies lead to another type of secondary glaucoma - open-angle. Secondary open-angle glaucoma is easier to tolerate, and its treatment brings a more noticeable effect.
Dystrophic
This includes forms of the disease that appear as a result of diseases of a dystrophic nature.
- Iridocorneal endothelial syndrome - is expressed in the inferiority of the corneal endothelium, iris atrophy and the formation of a thin membrane on the surface of the iris. It is characterized by damage to one eye.
- This also includes cases of increased IOP due to retinal detachment, intraocular hemorrhages, etc.
Inflammatory
Develops during or after the inflammatory process, with keratitis, scleritis, uveitis, etc. It occurs as a chronic open-angle glaucoma (with damage to the drainage system of the eyes and episcleral vessels) or as a closed-angle glaucoma (due to the occurrence of fusion and fusion of the pupil).
Traumatic
Based on the nature of the initial injury, it is divided into subtypes resulting from burns, radiation or exposure to chemicals. In this case, the causes may be various types of hemorrhages inside the eye, changes in the size and shape of the lens due to mechanical action, damage to the blood vessels of the eye due to injury from radiation or chemicals. This type of secondary glaucoma can appear even years after the injury. Therefore, it is very important to undergo a special examination after such injuries.
Vascular
A type of secondary glaucoma with retinal vein thrombosis, frequent hemorrhages, and eye cancer. Has two types.
- Secondary neovascular glaucoma - this dangerous type of disease develops in the presence of diabetes mellitus, consequences in the form of diabetic retinopathy, temporal arteritis, stenosis, and so on. New vessels first appear at the pupil along the edge of the iris, then spreading along the anterior surface of the iris.
- Phlebohypertensive - manifests itself due to increased pressure in the episcleral veins. In this case, the episcleral veins expand. This form of glaucoma can occur against the background of Sturge-Weber syndrome, edematous endocrine exophthalmos, etc.
Phacogenic
As a rule, it is a consequence of cataracts. This appearance appears due to changes in the lens. It has three types: phacotopic, phacomorphic and phacolytic.
Let's look at each of them in a little more detail:
- Phacotopic - this type is associated with dislocation-subluxation of the lens (displacement of the lens from its usual location) into the anterior chamber of the eye, or into the vitreous body. In the first case, it occurs according to the closed-angle type, so it is necessary to remove the lens.
- Phacomorphic - manifests itself due to swelling of the lens (during immature senile or traumatic cataract). In this case, a block of the pupil appears due to an increase in the lens fibers (the lens is not homogeneous, it consists of fibers). Removal of cataracts (while reducing IOP with medications) usually leads to a complete cure of this type of glaucoma.
- Phacolytic - occurs with overripe cataracts. In this case, protein molecules leave the lens body through the anterior capsule and clog the trabecular filter. This type is clinically similar to an acute attack of glaucoma with hyperemia of the eyeball, pain and high levels of intraocular pressure. Cure also occurs when cataracts are removed.
Neoplastic glaucoma
This is a complication of intraocular or orbital formations.
The reasons may be:
- melanoblastoma of the cornea and ciliary body
- tumor of the choroid proper
- retinoblastoma
In this case, the reasons for the increase in IOP of stage II–III tumors are:
- block of the anterior chamber angle by a tumor;
- deposition of its breakdown products.
The following methods are used to diagnose a tumor:
- echography
- diaphakoscopy
- radionuclide diagnostics
If vision continues to decline and a diagnosis cannot be made, doctors prefer to remove the eye, because there is a high probability of tumor development.
Postoperative
As a result of eye surgery, IOP may increase. This type of disease is one of the most common consequences of cataract surgery (aphakic glaucoma), retinal detachment, and keratoplasty. It can be either closed- or open-angle (ZUG and OUG).
Reactive hypertension of the eye, which appears from surgical trauma, can last from several hours to two to three days.