Aqueous humor circulates along the episcleral and intrascleral venous network of the anterior segmented area of the eyeball. It supports the metabolic processes of the cornea, lens, and trabecular apparatus. Under normal circumstances, the human eye contains 300 mm of the component or 4% of the total volume.
The fluid is produced from the blood by special cells that are part of the structure of the ciliary body. The human eye produces 3-9 ml of the component per minute. The outflow of moisture occurs through the episcleral vessels, uveoscleral system and trabecular meshwork. Intraocular pressure is the ratio of the produced component to the withdrawn component.
Structure
Functions
Symptoms
Treatment
Structure
The aqueous humor of the eye is almost 100% water. The dense component includes:
- anorganic components (chlorine, sulfate, etc.);
- cations (calcium, sodium, magnesium, etc.);
- insignificant proportion of protein;
- glucose;
- ascorbic acid;
- lactic acid;
- amino acids (tryptophan, lysine, etc.);
- enzymes;
- hyaluronic acid;
- oxygen;
- a small amount of antibodies (formed only in the secondary fluid).
Intraocular fluid is produced mainly by
Content
Intraocular fluid is produced mainly by Answer to test 1. c) 2. a) 3. b) 4. e) 5. a) 6. a) 7. a) 8. d) 9. a) 10. a) 11. a) 12. b) 13. b) 14. a) 15. c) 16. d) 17. c) 18. a) 19. a) 20. c
1. The thinnest wall of the orbit is: a) the outer wall b ) upper wall c) inner wall d) lower wall e) upper and inner
2. The optic nerve canal serves for the passage of: a) the optic nerve b) the abducens nerve c) the oculomotor nerve d) the central retinal vein e) the frontal artery
3. The lacrimal sac is located: a) inside the orbit b) outside the orbit c) partly inside and partly outside the orbit d) in the maxillary cavity e) in the middle cranial fossa
4. In case of eyelid wounds, tissue regeneration is: a) high b) low c) does not differ significantly from tissue regeneration in other areas of the face d) lower than in other areas of the face e) higher than in other areas of the face
5. Tear-producing organs include: a) lacrimal gland and accessory lacrimal glands b) lacrimal puncta c) lacrimal canaliculi d) nasolacrimal canal
6. The nasolacrimal canal opens into: a) the inferior lacrimal canal b) the middle nasal passage c) the superior nasal passage d) the maxillary sinus e) the main sinus
7. The sclera has the greatest thickness in the area of: a) limbus b) equator c) optic disc d) under the rectus tendon e) under the oblique tendon
8. The cornea consists of: a) two layers b) three layers c) four layers d) five layers e) six layers
9. The layers of the cornea are located: a) parallel to the surface of the cornea b) randomly c) concentrically d) in an oblique direction
10. The cornea is nourished by: a) marginal looped vascular network b) central retinal artery c) lacrimal artery d) anterior ciliary arteries e) supratrochlear artery
11. The optic disc is located: a) in the center of the fundus b) in the nasal half of the fundus c) in the temporal half of the fundus d) in the upper half of the fundus e) outside the fundus
12. The functional center of the retina is: a) optic disc b) fovea c) dentate line zone d) vascular bundle e) juxtapapillary zone
13. The optic nerve leaves the orbit through a) the superior orbital fissure b) for. Opticum c) inferior orbital fissure d) foramen rotundum e) maxillary sinus
14. The vascular tract performs: a) trophic function b) light refraction function c) light perception function d) protective function e) support function
15. The retina performs the following function: a) light refraction b) trophic c) light perception d) protective function e) support function
16. Intraocular fluid is produced mainly by: a) iris b) choroid c) lens d) ciliary body e) cornea
17. Tenon’s capsule separates: a) the choroid from the sclera b) the retina from the vitreous c) the eyeball from the orbital tissue d) there is no correct answer e) the cornea from the sclera
18. Bowman’s membrane is located between: a) corneal epithelium and stroma b) stroma and Descemet’s membrane c) Descemet’s membrane and endothelium d) layers of the retina
19. The choroid nourishes: a) the outer layers of the retina b) the inner layers of the retina c) the entire retina d) the optic nerve e) the sclera
20. The motor apparatus of the eye consists of - ... extraocular muscles a) four b) five c) six d) eight e) ten
Symptoms
The amount of fluid inside the eye may change due to the development of eye diseases or when exposed to external factors (trauma, surgery).
If the moisture outflow system is disrupted, a decrease in intraocular pressure (hypotension) or an increase (hypertonicity) is observed. In the first case, retinal detachment is likely to occur, which is accompanied by deterioration or complete loss of vision. With increased pressure inside the eye, the patient complains of headache, blurred vision, and the urge to vomit.
The progression of pathological conditions leads to the development of glaucoma - a disruption of the process of removing fluid from the organ of vision and its tissues.
How to treat?
Many patients agree to treat glaucoma with laser. This procedure is divided into 3 types such as:
- trabeculoplasty;
- surgery that affects the iris;
- cyclophotocoagulation.
In the first stages, you can stop the development of the disease with eye drops. But they are not effective if the pathology progresses for a long time. In addition, they should be prescribed on an individual basis, since some drugs cause an allergic reaction. In more complex situations, they resort to surgical intervention - trabeculectomy. During the operation, the doctor creates a channel for the outflow of fluid. But sometimes one procedure is not enough, so the operation is repeated.
Diagnostics
Diagnostic measures for suspected development of pathological conditions in which the intraocular fluid for some reason is in excess, in deficiency, or does not go through the entire circulation process inside the eye, are reduced to the following procedures:
- visual examination and palpation of the eyeball (the method allows you to determine visible deviations and location of pain);
- fundus ophthalmoscopy - a procedure to assess the condition of the retina, optic nerve head and vascular network of the eye using an ophthalmoscope or fundus lens;
- tonometry is an examination that allows you to determine the level of change in the eyeball when exposed to the eye cornea. With normal intraocular pressure, deformation of the sphere of the organ of vision is not observed;
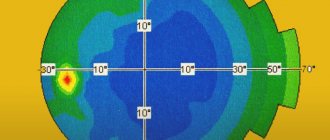
- perimetry – a method of determining visual fields using computer technology or special equipment;
- campimetry – identification of central scotomas and size indicators of the blind spot in the visual field.
General information
The production and outflow of intraocular fluid is regulated by intraocular pressure. It fluctuates during the day from 9 to 22 mm Hg. Art. It usually rises in the morning and returns to normal in the evening. With normal pressure in the eye, fluid is produced that nourishes the lens and iris. It contains proteins, chlorides, ascorbic acid. When there is a lack or blockage of fluid flow to a certain part of the eye and its accumulation, glaucoma can develop. This disease is dangerous because it occurs unnoticed in the first stages, and then leads to blindness and atrophy of the optic nerve.
Treatment
For the above-mentioned disorders, as part of the therapeutic course, the patient is prescribed medications that restore intraocular pressure, as well as medications that stimulate blood supply and metabolism in the tissues of the organ.
Surgical treatment methods are applicable in cases where drugs do not have the desired effect. The type of surgery performed depends on the type of pathological process.
Thus, the intraocular fluid is a kind of internal environment of the organ of vision. The composition of the element is similar to the structure of blood and provides the functional purpose of moisture. Local pathological processes include disturbances in fluid circulation and deviations in its quantitative indicator.
Outflow of intraocular fluid
The cavity of the eye contains light-conducting media: aqueous humor that fills its anterior and posterior chambers, the lens and the vitreous body. Regulation of metabolism in the intraocular structures and maintenance of the tone of the eyeball is ensured by the circulation of intraocular fluid in the chambers of the eye. This is the anatomical norm for the eye. Intraocular fluid is an important source of nutrition for the internal structures of the eye. Aqueous humor circulates mainly in the anterior segment of the eye. It is involved in the metabolism of the lens, cornea, vitreous body and plays an important role in maintaining a certain level of intraocular pressure.
Intraocular fluid is continuously produced by the processes of the ciliary body and accumulates in the posterior chamber, which is a slit-like space of complex configuration located behind the iris. Then most of the moisture flows out through the pupil, washing the lens, after which it enters the anterior chamber and passes through the drainage system of the eye, located in the area of the angle of the anterior chamber - the trabecula and Schlemm's canal (venous sinus of the sclera). From it, the intraocular fluid flows through the outflow collectors (leavers) into the superficial veins of the sclera. This is a physiological norm that ensures normal outflow of intraocular fluid.
This path is the main one, and an average of 85–95% of aqueous humor flows through it. In addition to the anterior pathway for the outflow of intraocular fluid, there is also an additional one: approximately 5–15% of aqueous humor leaves the eye, seeping through the ciliary body and sclera into the veins of the choroid and scleral veins, forming the so-called uveoscleral outflow tract.
Development mechanism
Glaucoma is considered a multifactorial disease with a threshold effect. This means that for the development of the disease, a number of reasons are necessary, which together lead to its occurrence. Particularly important are heredity, individual characteristics or anomalies in the structure of the eye, pathology of the cardiovascular, nervous and endocrine systems.
Currently, scientists suggest that the development and progression of glaucoma is a sequential chain of risk factors that are cumulative in their action, resulting in the triggering of a mechanism leading to the onset of the disease.
However, the mechanisms of visual dysfunction in the pathogenesis of glaucoma remain poorly understood to date. The main stages of development of the pathological process in glaucoma can be presented as follows:
- disruption and deterioration of the outflow of aqueous humor from the cavity of the eyeball, which can be due to a variety of different reasons;
- an increase in intraocular pressure (IOP) above a level that is tolerable (tolerable, tolerable) for a given eye;
- deterioration of blood circulation in the tissues of the eye;
- hypoxia (lack of oxygen) and ischemia (impaired blood supply) of tissues in the area where the optic nerve exits;
- compression (squeezing) of nerve fibers in the area of their exit from the eyeball, which leads to disruption of their function and death;
- dystrophy (malnutrition), destruction (destruction) and atrophy of optic fibers, disintegration of their maternal retinal ganglion cells;
- the development of so-called glaucomatous optic neuropathy and subsequent atrophy (death) of the optic nerve.
Depending on the development of the glaucomatous process, some of the nerve fibers of the optic nerve atrophy, and some are in a state of parabiosis (a kind of “sleep”), which makes it possible to consider it possible to restore their function under the influence of treatment (medical or surgical).
One important postulate follows from the above. Treatment of glaucoma is aimed, first of all, at normalizing the level of intraocular pressure (IOP) and bringing it to an individual tolerant level - i.e. values carried by the optic nerve of a particular patient (usually 16-18 mm Hg when measured with a standard Maklakov tonometer).
This so-called target pressure is the IOP level that the ophthalmologist who prescribes drops and the surgeon who performs antiglaucomatous surgery strives for. The effect of treatment primarily depends on the preservation of the nervous tissue and therefore, as a rule, it can be said objectively that the visual functions that are “taken away” by glaucoma do not return.