A person’s success directly depends on how quickly he orients himself in space and time. The key to this is, among other things, visual acuity. Technological progress and the rapid modern pace of life can cause vision deterioration at a fairly young age. World ophthalmology is guarding this. Preventive diagnostics includes a huge range of procedures to monitor eye health.
One of these procedures is perimetry - the study of the boundaries of the visual field (peripheral vision), the indicators of which help ophthalmologists diagnose eye diseases, in particular glaucoma or optic atrophy. To measure the necessary parameters, doctors have modern diagnostic equipment in their arsenal, the examination of which is painless and without contact with the surface of the eyes, which reduces the risk of inflammation.
In case of any problems, it is recommended to consult a doctor without delay, and also not to neglect annual preventive examinations.
The concept of the boundaries of the field of view
Content:
- The concept of the boundaries of the field of view
- Indications for the procedure
- Contraindications to perimetry
- Diagnostic methods
- Computer perimetry
- Decoding the results
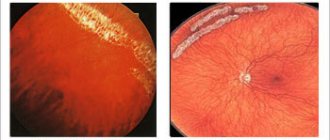
Peripheral vision gives a person the ability to see and recognize a certain volume of objects around him. To check its quality, ophthalmologists use a technique for studying the boundaries of the visual field, which is called perimetry. In medicine, the boundaries of the visual field mean the visible space that a stationary eye can recognize. In other words, this is an overview that is available provided that the patient's gaze is fixed on one point.
The quality of such visual ability is directly dependent on the volume of points present in space, which are covered by a stationary eye. The presence of certain deviations in the indicator obtained during perimetry gives the doctor grounds to suspect a particular eye disease.
In particular, determining the boundaries of the visual field is necessary in order to find out what condition the retina or optic nerve is in. Also, such a procedure is indispensable for identifying pathologies and diagnosing ophthalmological diseases, such as glaucoma, and prescribing effective treatment.
Table for determining visual acuity
For normal visual acuity (1.0 or “one”), the distinguished elements must have an angular size of 1', while the entire optotype has an angular size of 5' - this international agreement on the size of parts formed the basis for the creation of optotypes.
The method of testing vision according to the Golovin-Sivtsev table, placed in a Roth apparatus, is the most common in Russian clinics (in commercial ophthalmological centers they often use sign projectors from foreign manufacturers with a different set of signs).
Indications for the procedure
In medical practice, there are a number of indications for which it is necessary to prescribe perimetry. For example, visual field impairment can be caused by the following reasons:
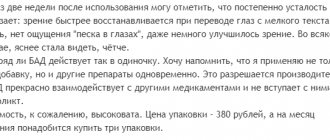
- Retinal dystrophy, in particular its detachment.
- Retinal hemorrhages.
- Oncological formations on the retina.
- Injuries to the optic nerve.
- Burns or eye injuries.
- The presence of certain ophthalmological diseases.
In particular, perimetry makes it possible to diagnose glaucoma with subsequent research and clarification of this diagnosis or to establish diseases associated with damage to the macula.
In some cases, information about perimetry data is required when applying for a job. With its help, the employee is checked for increased attentiveness. In addition, using this research method, it is possible to diagnose traumatic brain injuries, chronic hypertension, as well as strokes, ischemic disease and neuritis.
Finally, visual field detection helps identify feigning moods in patients.
Vision testing methods for visually impaired patients
With a significant decrease in visual acuity, the quality of life of the subject is greatly reduced. His movement and other movements are difficult, and it is not possible to conduct an examination using tables. In such cases, a number of other methods are used.
Eye test by counting fingers. Here the verification is carried out by counting fingers. The patient is shown fingers from different distances and the result is recorded, in which he was able to name their number. For example, the entry might look like this: “Vis OS counting fingers from 4 m.”
Determination of the patient's level of light perception. This method is used if others are not possible. Visometry is carried out using a point source of light, which is directed into the eye from different angles and sides. This allows you to determine the sensitive areas of the retina, and determine whether the correct light projection is preserved (important for further therapy). The following entry is made: visus =1/∞ proectio lucis certa, or briefly - plc Its decoding will mean “the quality of vision corresponds to the perception of light, the light projection is preserved and correct.”
Sometimes a number of other methods are used to determine the quality of vision, which are called objective methods.
- When determining optokinetic nystagmus, the patient is shown a chessboard or grid and the eye movements are observed. The result is recorded by involuntary eye movement.
- When studying visual evoked potentials, fixation of electrical potentials in the occipital region using special equipment. They appear with minimal differentiation of the shown patterns.
- When testing forced selective vision, two types of drawings are used: in the form of a solid strip and a checkerboard. The child is more willing to look at a structured object, while he is required not only to move his eyes, but also his head and neck. This is recorded (it will be erroneous if there are disorders of the child’s oculomotor system).
Contraindications to perimetry
In some cases, the use of perimetric diagnostics is contraindicated. In particular, this technique is not used in cases of aggressive behavior of patients or the presence of a mental disorder. The results are distorted not only by patients being in a state of alcohol or drug intoxication, but also by the consumption of even minimal doses of alcohol-containing drinks. Contraindications to determining peripheral visual acuity are also the mental retardation of patients, which does not allow them to follow the doctor’s instructions.
If such a diagnosis is necessary in these cases, doctors recommend resorting to alternative methods of examination.
Diagnostic methods
To carry out perimetry in ophthalmological practice, several types of devices are used, which are called perimeter. With their help, doctors track the boundaries of the visual field using specially developed methods.
The following are the main types of procedure. All of them are painless and non-invasive, and do not require any preliminary preparation from the patient.
Kinetic perimetry
This is a procedure that allows you to evaluate the dependence of the field of view on the size and color saturation of an object that is moving. This test requires the presence of a bright light stimulus in an object moving along predetermined trajectories. During the examination, points are recorded that cause a certain reaction in the eyes. They are entered into the perimetric study form. Their connection at the end of the event makes it possible to identify the trajectory of the boundaries of the field of view. When carrying out kinetic perimetry, modern projection perimeters with high measurement accuracy are used. With their help, a number of ophthalmological pathologies are diagnosed. In addition to ophthalmological abnormalities, this research method makes it possible to detect some pathologies in the functioning of the central nervous system.
Static perimetry
During static perimetry, a certain stationary object is observed and recorded in a number of areas of the visual field. This diagnostic method allows you to determine the sensitivity of vision to changes in the intensity of the image display, and is also suitable for screening studies. In addition, it can be used to determine initial changes in the retina. An automatic computer perimeter is used as the main equipment, making it possible to study the entire field of view or its individual sections. Using such equipment, a threshold or suprathreshold perimetric study is carried out. The first of them allows you to obtain a qualitative assessment of the sensitivity of the retina to light, and the second allows you to record qualitative changes in the visual field. These indicators are aimed at diagnosing a range of ophthalmological diseases.
Campimetry
Campimetry refers to the assessment of the central visual field. This study is carried out by fixating the eyes on white objects that move along a black matte screen - a campimeter - from the center to the periphery. The doctor marks points where objects temporarily fall out of the patient's field of vision.
Amsper's test
Another fairly simple method for assessing the central visual field is the Amsper test. It is also known as the Macular Retinal Degeneration Test. During diagnosis, the doctor studies the reaction of the eyes when the gaze is directed at an object located in the center of the grid. Normally, all grid lines should appear absolutely even to the patient, and the angles formed by the intersection of the lines should appear straight. If the patient sees the image as distorted, and some areas are curved or clouded, this indicates the presence of pathology.
Donders test
Best materials of the month
- Why you can't go on a diet on your own
- 21 tips on how to avoid buying stale food
- How to keep vegetables and fruits fresh: simple tricks
- How to curb your sweet cravings: 7 unexpected products
- Scientists say youth can be extended
The Donders test allows you to very simply, without the use of any instruments, determine the approximate boundaries of the visual field. When carrying it out, the gaze is fixed on an object, which begins to move from the periphery to the center of the meridian. In this test, along with the patient, an ophthalmologist is also involved, whose visual field is considered normal.
The doctor and the patient, located at a distance of a meter from each other, must simultaneously focus on a specific object, provided that their eyes are at the same level. The ophthalmologist covers his right eye with the palm of his right hand, and the patient covers his left eye with the palm of his left hand. Next, the doctor raises his left hand from the temporal side (beyond the line of sight) half a meter from the patient, and begins, moving his fingers, to move the hand to the center. The moments are recorded when the eye of the subject catches the beginning of the appearance of the contours of an object that is moving (the doctor’s hands) and its end. They are decisive for establishing the boundaries of the visual field for the patient’s right eye.
A similar technology is used to fix the outer boundaries of the visual field in other meridians. In this case, to study in the horizontal meridian, the ophthalmologist’s hand is positioned vertically, and in the vertical meridian - horizontally. In a similar way, only in mirror image, the visual field indicators of the patient’s left eye are examined. In both cases, the ophthalmologist's field of view is taken as the standard. The test helps to determine whether the boundaries of the patient’s visual field are normal or whether they are narrowing concentrically or sector-wise. It is used only in cases where it is not possible to carry out instrumental diagnostics.
Central vision
To diagnose visual acuity and objectively assess it in clinical practice, visometry is used.
Normal visual acuity is diagnosed if two points that the eye can distinguish are located at an angle of 1 minute. For convenience, ophthalmologists prefer to measure visual acuity using reciprocal values rather than visual angles. In this case, normal vision corresponds to the inverse value of an angle of 1 minute. In this case, the following pattern applies: visual acuity is in inverse proportion to the magnitude of the visual angle. That is, the smaller the angle, the higher the visual acuity. As a result of the research, special tables were developed that allow us to establish visual acuity. Their main difference is the variety of optotypes (test objects), the value of which can be used to determine the severity.
In optics there are concepts used in practice. These include the minimum visible, recognizable and distinguishable. In this case, the patient must see the test object, distinguish the details of the optitype, recognize signs and letters. To test vision, optotypes are projected onto a screen or placed on a wall. Letters, digital symbols, drawings, circles, and stripes are used as test objects. The main condition for an optotype is a certain size. It is selected in such a way that from a certain distance, significant details are visible at a viewing angle of 1 minute. The entire optotype must fit within a visual angle of 5 minutes. The international optotype is represented by a Landolt ring, which has a gap in the outline.
In domestic practice, ophthalmologists more often use Sivtsev’s letter tables. In each table, the letters are arranged in 12 rows, which gradually decrease towards the bottom of the poster. In this case, the degree of reduction in letter sizes corresponds to arithmetic regression. The top 10 rows have a step of 0.1 units of visual acuity, the last two rows – 0.5 units. That is, if the patient is able to distinguish the fourth row of letters, then his vision is 0.3, if the fifth, then 0.5.
When conducting optometry using Sivtsev tables, the subject is seated at a distance of five meters from the screen, the lower edge of which is located at a level of 120 cm from the floor.
First, the visual acuity of one eye is checked, then the second, while the opposite eye is covered with an impenetrable shield. If the patient can distinguish the details of the tenth letter row from a distance of five meters, then his visual acuity is normal and is 1.0. For convenience, at the end of each row the visual acuity (V) is indicated, which corresponds to the given letter size. At the beginning of the row there is a distance (D) from which the acuity can be set to 1.0, provided that the subject reads this line. For example, a person with 1.0 vision can distinguish the letters of the first line from a distance of 50 meters.
In some patients, it is possible to identify a higher level of visual acuity, which corresponds to 1.5 or even 2.0. They can distinguish between the eleventh and twelfth rows of the table, respectively. If the patient's visual acuity is less than 0.1, then the subject should be brought closer to the table until he sees the first line.
Due to the fact that the thickness of the optotypes of the first line approximately corresponds to the thickness of the fingers, for an approximate assessment of visual acuity, you can show the patient the fingers spread to the maximum distance. It is advisable to place them on a dark background. When the distance changes, it becomes possible to determine visual acuity if this indicator is below 0.1. If the acuity value is less than 0.01, but the patient is able to count fingers at a distance of 10, 20, 30 cm, then visual acuity corresponds to counting fingers at this distance. Sometimes the subject cannot count the fingers, but is able to detect the movements of the hands near his face. In this case, visual acuity moves to the next gradation.
The minimum indicator of visual acuity is vis=1/-, which corresponds to light perception. In this case, the light projection can be correct or incorrect. To determine light projection, a beam from an ophthalmoscope is used, which is directed from different directions. If there is no light perception, then visual acuity is taken as zero (vis = 0), that is, the eye is considered blind.
In children who do not yet know alphabetic signs, Orlova tables are used to determine visual acuity. In this case, various objects and animals serve as optotypes. However, first you should review all optotypes with your child so that they are recognizable to him.
If the patient's visual acuity is less than 0.1, then Polyak's optotypes, which are line tests and open rings, can be used. They are shown at close range. It is these test objects that are suitable for medical and social examination services and the military medical commission, which are carried out to identify contraindications to military service or the presence of disabilities.
In addition to subjective methods for determining visual acuity, there is also an objective type of examination. It is based on optoclistic nystagmus. Using special equipment, the patient is shown moving optotypes, which are represented by stripes or squares of a chessboard. In this case, the subject experiences involuntary nystagmus, which is recorded by the doctor. The smallest optotype value at which nystagmus is recorded is considered the value of visual acuity.
To correctly determine visual acuity, you should follow a number of important recommendations:
1. Visual acuity should be determined separately for each eye (monocularly). It is preferable to start the study with the right eye. 2. When conducting an examination, you should not squint your other eye; it is better to keep it open and cover it with a shutter. If the subject covers his eye with his palm, it is important not to press too hard on the eyelids, as this may temporarily reduce vision. To eliminate the possibility of peeking, the shutter should be held strictly vertically, avoiding light falling on the eyeball. 3. During optometry, the patient's head, eyelids and gaze should be correctly positioned. In this case, you should avoid bending to the side, turning your head or tilting it forward. It is also not allowed to squint, as this may increase visual acuity (in patients with myopia). 4. Last but not least is the time factor. Thus, in standard clinical work the time is about 2-3 seconds, and in control experimental studies it reaches 4-5 seconds. 5. Optotypes must be demonstrated to the patient using a pointer, the end of which is clearly visible. For clarity, the tip of the pointer is placed directly below the sign, at some distance so as not to overlap the details. 6. At the beginning of the examination, the doctor demonstrates the signs from the tenth line, then, if necessary, the doctor moves on to higher lines. If it is known that the patient has reduced visual acuity, then in some cases the study begins from the top line, gradually moving down. If the patient makes a mistake, the doctor returns to the overlying signs.
Only the row in which the patient was able to identify all the signs without errors is suitable for assessing visual acuity. If the patient made a mistake once in rows three to six and twice from seven to ten, then visual acuity can be assessed using these rows, but be sure to indicate the errors in the medical documentation.
To diagnose visual acuity and objectively assess it in clinical practice, visometry is used.
To determine visual acuity at close range, you need to use a special table located at a distance of 33 cm from the eyes. If the visual acuity of the subject is less than 0.1, that is, he is not able to read even the top line, then at the second stage the doctor must determine the distance from which the patient begins to distinguish the letters of the top line. To do this, the subject is gradually brought closer to the table until he can read the letters of the top row. It is also possible to use cut tables, which consist of optotypes, the dimensions of which coincide with the first row. In this case, the tables themselves are brought closer to the immobile patient.
Assessing visual acuity in a newborn is quite difficult; for this purpose, a friendly and direct reaction of the pupil to light is used. If the child's eyes are illuminated, then the closing of the eyelids and the general reaction of the body will normally follow. At the age of two weeks, the child can register bright objects in the field of vision by turning his eyes towards them, and the ability to observe them for a short time also appears. At the age of 1-2 months, the baby can fix his gaze on an object and follow it with both eyes. From 3-5 months, vision is checked using a bright red ball, the diameter of which is 4 cm. By the age of one year, the size of the ball decreases to 0.7 cm. If you place the ball at different distances from the baby, you can determine the approximate visual acuity. If the baby has no vision, then he remains able to respond only to sounds or smells.
Visual acuity decreases for various reasons, among which there are three groups of factors:
1. The most common cause is refractive error, which includes astigmatism, myopia, and farsightedness. Most often, visual acuity improves or is completely restored with the use of optical devices (lenses, glasses). 2. The second group includes pathologies that are associated with clouding of the transparent media of the eyeball, which are responsible for refraction. 3. The third group of causes combines the pathology of the retina, as well as nerve fibers (optic nerve, pathways, cortical centers).
It is important to note that visual acuity changes significantly as the patient ages and matures. In this case, maximum values are observed at 5-15 years, and by 40-50 years there is a gradual decrease in visual acuity.
- Interesting
How to maintain normal vision in a child?
- Interesting
New treatments for amblyopia
The traditional way to treat amblyopia, or “lazy eye” in children, is most often to tape the stronger eye,…
- Interesting
Visual impairment in children - how to stop it
Various visual impairments in children are currently, unfortunately, widespread. Eye pathologies...
Computer perimetry
The greatest accuracy in assessment is provided by computer perimetry, for which a special computer perimeter is used. This modern, highly effective diagnostics uses programs to conduct a screening (threshold) study. Intermediate parameters of a number of examinations remain in the device’s memory, which makes it possible to conduct a static analysis of the entire series.
Computer diagnostics allows you to obtain a wide range of data on the state of vision of patients, ensuring their greatest accuracy. However, it is not anything complicated and looks like this.
- The patient is positioned in front of the computer perimeter.
- The specialist asks the subject to fix his gaze on an object that is presented on the computer screen.
- The patient can see a number of marks moving chaotically across the monitor.
- Having fixed his gaze on the object, the patient presses a button.
- Data on the results of the inspection are entered into a special form.
- At the end of the procedure, the doctor prints out the form and, after analyzing the results of the study, gets an idea of the state of vision of the subject.
During the procedure according to this scheme, a change in the speed, direction of movement and color scheme of objects presented on the monitor is provided. Due to its absolute harmlessness and painlessness, this procedure can be repeated many times until the specialist is convinced that objective results of the study of peripheral vision have been obtained. After diagnosis, no rehabilitation is required.
Objective methods of visometry
Objective methods for determining visual acuity can be used in children when malingering and aggravation are suspected, to clarify the cause of vision loss, that is, in cases where standard visometry is not suitable.
Optokinetic nystagmus method
In this case, special objects are used that have a periodic structure, for example, a chessboard or a lattice. The subject is shown this object in motion, and the doctor observes the nystagmus of the patient's eyes. If the patient is able to distinguish the structures of an object, then his eyes make involuntary and rhythmic movements. Visual acuity is determined by the size of the minimum object that causes nystagmus.
Visual evoked potential method
In this case, the examination does not depend on eye movement, but the patient must be attentive. At the same time, electrical potentials that are formed in the cells of the occipital region of the brain in response to visual stimuli are recorded. The subject is shown a field with black and white cells that change places with a given frequency. In this case, the cells gradually decrease in size. Those cells that lead to oscillations on the EEG that coincide with the reversal of colors are considered minimally distinguishable.
Forced selective vision method
The preferred gaze test is based on the fact that a person, in particular a child, prefers to look not at homogeneous objects, but at structured ones. In this case, two test objects are placed in front of the subject’s eyes. One of them is uniformly colored gray, and the second is represented by vertical stripes. Typically the test is performed using Keeler cards. If the child is able to distinguish between them, then he prefers to look at the brighter object, which is represented by a grid. Assessing visual function requires not only eye movements, but also head and neck movements. In this regard, if it is impossible to perform the test, we may be talking about a violation of the oculomotor function, and not at all about problems with the primary sensory system.