The retina of the eye is a part of the visual analyzer that provides the perception of visual images. Light-sensitive cells carry a large functional load, so the blood supply to the retina is more intense than to other parts of the eye. Arterial blood cells are obtained from the central retinal artery and the choroid. The outflow of the resulting venous blood is completely carried out by the central retinal vein (CRV). Disruption of the blood flow of the central vein provokes venous stagnation and the occurrence of hemorrhages, thrombosis of the central vein. The process can have serious consequences and requires immediate treatment and subsequent long-term observation.
Causes of the disease
There can be many reasons for the occurrence of this pathology, but mainly it is caused by other diseases of the body.
For example, processes occurring during diabetes mellitus, atherosclerosis or arterial hypertension affect the vessel. It thickens significantly, which, in turn, causes compression of the retina by the adjacent artery and deterioration of blood flow. As a result, a blood clot may form. Stagnation of blood significantly affects the fundus of the eye: blood vessels lose strength, more blood flows out, and characteristic swelling occurs.
With cataracts and glaucoma, complete loss of vision is possible
Glaucoma can also be a cause of blockage of the central vein. Diseases affecting blood viscosity or taking medications can also be a cause.
Diagnostics
The main and accurate research method in such a situation is an examination of the fundus. The study provides complete information about the condition of the fundus vessels and their structural features.
The analysis is carried out using a special device - an ophthalmoscope. Fundus examination is the only way to accurately diagnose or stage vascular disease.
Stages of retinal vein thrombosis
The disease develops gradually. In medicine, several stages have emerged, differing in characteristic features:
- The prethrombosis stage, that is, “preparation” before the initial stage of the disease. Its peculiarity is the change in the size of the veins, their unevenness, curvature and different thickness. Minor swelling begins to form and small effusions of blood are noticeable. The patient may experience dizziness and foggy vision, but these manifestations are rare, so most people often do not even suspect that they are developing an ocular thrombosis.
- Initial manifestations of the development of the disease, which doctors call “initial thrombosis.” This stage is difficult to miss; it is visible visually on the retina in the form of networks of hemorrhages. Changes in vision also appear, or rather, its sharp deterioration. Fog and noise are also characteristic of this initial stage.
- Rapid development of post-traumatic retinopathy. This process occurs directly under the influence of vein blockage. There may be leaps in the direction of improving the “purity” of vision, but for short periods of time. Cyst-shaped edema is characteristic. The vascular network, which covers the entire possible area of the eyeball, becomes dangerous.
Thrombosis of the central retinal vein Often, after treatment, a relapse of the disease is possible, and the stages are repeated in the same sequence.
Thrombosis of the central retinal vein of the eye is divided into two different types:
- Non-ischemic type of thrombosis - the condition of the retina remains almost unchanged and even the level of vision remains quite high.
- Ischemic thrombosis - blood flow is disrupted, vision decreases sharply. Hemorrhages and swelling are visually noticeable. In the ischemic form, diagnosis and treatment should be carried out immediately, and then be under constant medical supervision to avoid relapse.
How it develops
The development of pathology is divided into several stages:
- Prethrombosis - this stage is characterized by dilation and tortuosity of the ophthalmic veins, as well as single small hemorrhages. At the initial stage, there may not be any noticeable clinical manifestations; occasionally, short-term formation of a veil is possible.
- Direct thrombosis. This is the stage when the fundus of the eye is covered with small but multiple hemorrhages and swelling of the macula of the retina. Patients experience a sudden drop in visual acuity and color perception.
- Postthrombotic changes. Bruises and newly formed thin vessels are visible in the fundus. Visual acuity is restored within several years.
What therapy is prescribed?
Treatment of central vein thrombosis is usually carried out in an inpatient setting. The process itself takes a lot of time and requires patience from the patient. The primary goal of therapy is to improve vision and prevent the possibility of complications of the disease. Medicines used to treat thrombosis of the arteries of the eye include the following groups of drugs:
fibrinolytics destroy fibrin and restore blood flow in the vessel. Administered as an injection under the eye daily, 0.5 ml for 14 days. This group of drugs includes Fibrinolysin and Plasminogen;
- Antihypertensive drugs help reduce blood pressure and retinal edema. Used for intravenous injection and orally. The use of antihypertensive drops is also provided. For thrombosis of the central vein, intramuscular injections of Lasix and intravenous injections of Papaverine and Dibazol are given. Arutimol, Glautam and Okumed are used as eye drops of the hypotensive group;
anticoagulants are prescribed after treatment with fibrinolytics. The course of therapy is no more than 6 days. Heparin or Sulodexide is used as a direct anticoagulant. Treatment with Heparin is carried out comprehensively: both intramuscularly and parabulbarly;
- antiplatelet agents are used to reduce the risk of recurrent blood clots in the retinal artery. Quite often, Aspirin and Plavix are prescribed. These medications should be taken only in accordance with all the instructions of the attending physician, as they have a number of contraindications;
- hormonal medications reduce the inflammatory process and remove swelling. They must be taken regularly. Dexamethasone is administered parabulbarly for a week; quite often this drug is combined with Heparin.
A complete and detailed course of treatment can be determined exclusively by the attending physician according to all diagnostic studies. In the initial stage of retinal thrombosis, the course of therapy lasts a month, and daily use of Aspirin and Sulodexide in tablet form is mandatory.
Dexamethasone and Heparin are administered by injection for 10-12 days. Drops and eye ointments are used throughout the course of therapy.
In cases of acute thrombosis of the ophthalmic arteries, therapy is carried out more actively. Plasminogen injections are given parabulbarly over 12 days, while Furosemide, Dextran and Sodium chloride are injected in parallel. After a month's course of therapy, the patient experiences a decrease in blood clots and hemorrhages, swelling of the retina goes away and the risk of neoplasms decreases.
Laser coagulation of the retina is an alternative method for restoring the arteries of the visual organs. This operation is recognized as an ideal solution for the treatment of diseases of the eye shell.
This surgical measure is carried out using special equipment and is excellent for patients with loss of vision. Laser coagulation improves blood circulation and stabilizes vision.
Treatment
The main task in case of thrombosis is to detect the disease in time and begin to treat it as quickly as possible.
Medications
The use of medications is aimed at the following actions:
- dissolution of hemorrhages;
- restoration of blood circulation;
- normalization of retinal nutrition;
- reduction of swelling.
The following means are used:
- Antihypertensive (hypotensive) - reduce blood pressure, reduce swelling of the retina (intravenous injections of Dibazol, Papaverine, oral tablets - Lizoril, eye drops - Arutimol, Timolol);
- Fibrinolytic agents - promote the resorption of blood clots, restore blood circulation (daily eye injections of Plasminogen, Fibrinolysin, 0.5 milliliters for two weeks);
- Antithrombotic (anticoagulant) agents are used after a course of fibrionalytics to prevent blockages of the vessel. The direct-acting anticoagulant “Heparin” is used as a complex injection intramuscularly and into the lower eyelid area, the course is a week;
- Antiplatelet drugs - to prevent recurrence of the disease: Aspirin, Plavix tablets;
- Hormonal agents - serve to relieve inflammation and swelling. Drugs containing the active substance dexamethasone are administered by injection into the lower eyelid for a week;
- Vitamins - groups C and B.
Treatment at home
It is important to understand that it is impossible to fully cure eye thrombosis with folk remedies. They serve rather to prevent this disease. At the first suspicion, be sure to contact a qualified specialist.
This includes the following options:
Drops
- Take twenty grams of herbs, for example: cumin, cornflower flowers or plantain leaves, insist on two hundred grams of boiling water, strain. Instill five times a day during the entire course of treatment.
- Take clover, woodlice, squeeze out the juice and bury it.
Contraindications are possible in case of individual intolerance to the components.
Compresses
Compresses are made from tea leaves, cucumber juice, and herbal infusions. Twenty grams of any ingredient are poured with boiling water and left for an hour. The mixture in gauze is placed on the eyelids and kept for half an hour to fifty minutes. The procedure is carried out for two weeks, then after a break of fourteen days, the course is repeated.
Infusions, decoctions
It is good to use infusions from the following plants:
- hawthorn flowers;
- sage;
- mint leaves;
- lemon balm;
- elecampane root and others.
They can be brewed as tea, or the decoction can be infused in a thermos, or a vodka tincture can be prepared for ten days.
Gymnastics and massage
There are many options for eye exercises, here are some of them;
- Open and close your eyes with tension (five times); look right, left, up, down (five times).
- Blink intensely for two minutes.
- Massage with light pressure on the eyeball for two seconds. Repeat up to ten times.
Laser surgery
Laser treatment (laser coagulation) has a great effect; it is used after therapeutic treatment with medications, if the disease is ischemic in nature and the use of pharmaceutical drugs does not produce noticeable results.
The intervention is based on the effect of a laser on a blood clot, with the aim of resolving it and, as a result, normalizing blood flow in the retina.
Who is most at risk for CVV thrombosis?
Diseases of the central vein of the retina are typical for those who lead a sedentary lifestyle, do not play sports and generally move little.
Due to poor nutrition, the disease can also progress, especially if there is a degree of obesity.
Retinal thrombosis often occurs in people with cardiovascular disease.
Frequent patients with retinal thrombosis are people with cardiovascular diseases.
A special place among risk groups is occupied by the number of people with endocrine system problems.
Causes
Very often, the causes of thrombosis are diseases not related to the organs of vision. Among the most common reasons:
- Arterial hypertension;
- Atherosclerosis;
- Diabetes;
- Infectious diseases of various types;
- Increased pressure inside the eyes;
- Swelling of the optic nerve;
- Tumors.
The risk group, as a rule, consists of people leading a sedentary lifestyle, suffering from excess weight, heart disease and pathologies of the endocrine system.
Symptoms of retinal vein thrombosis
Each stage of disease progression has its own set of characteristic symptoms.
In the first stage of prethrombosis, the symptom is venous congestion, the veins themselves are dark in color, dilated, in the form of convolutions and crosses. Blood flow also slows down significantly.
The beginning of thrombosis of the central vascular system of the eye is also characterized by such indicators as wide and tense veins, with tissue edema and pinpoint effusions of blood.
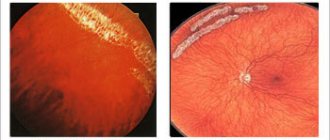
With complete thrombosis, the level of vision drops significantly, swelling of the nerve of the fundus disc is noticeable, the veins are immersed in the retina with edema, while they have a wide shape, and the arteries, on the contrary, are narrowed, and there is an outpouring of blood in large quantities and in various shapes.
Thrombosis of veins and arteries of the retina: stages of development
If thrombosis of the central vein is incomplete, symptoms in the form of hemorrhages in smaller sizes are characteristic. With thrombosis of the branches, they appear only at the bottom of the eye. Next, white foci develop - shine and degeneration are combined.
At the end of the stage of complete occlusion, new noticeable vessels may appear in the disc areas and in the center of the fundus of the eye. These formations are very permeable. Complications or a recurrent process may be indicated by hemorrhages and hemophthalmas of these new vessels. Further development of the disease can provoke secondary hemorrhagic glaucoma, degeneration and maculopathy of the retina, and atrophy of the nerve responsible for vision.
Thrombosis of the branches rarely develops into hemorrhagic glaucoma, but changes in the central area are quite common.
If we consider the symptoms depending on the type of disease, then for the non-ischemic variant they are less noticeable, but you can still consider the following:
Branch thrombosis rarely progresses to hemorrhagic glaucoma
- gradual slight decrease in the level of vision;
- peripheral blood effusions;
- The arteries are characterized by pallor and inconspicuousness.
Symptoms of the ischemic type are more noticeable and noticeable, mainly:
- thick effusions of blood like confluent lesions, the so-called “squashed tomato syndrome”;
- large and massive swelling with blood effusions;
- noticeable and significant decrease in the level of vision of the eye;
- slow pupil reactions to light stimuli;
- arteries are characterized by a pronounced manifestation of stenosis.
Prevention and prognosis
Retinal artery embolism belongs to dangerous vascular diseases. In order to get rid of this pathology, a lot of time and effort is required. It is necessary to take preventive measures to reduce the likelihood of developing blood clots.
To do this, you need to consult a doctor in such a situation. Because each situation is individual and requires a different approach. But the general rules of prevention are:
- Quitting smoking and drinking alcohol.
- Proper nutrition and an active lifestyle.
- Sleep at least 8 hours a day.
- Drink more fluid, 2 liters per day.
- Do not work in front of a computer for a long time.
Important! Preventing the formation of thrombosis in the vessels of the retina is easier than treating it.
We must remember this, because the eyes are the main sense organs of a person. Often the preservation of vision depends only on the patient himself.
Forecast
In the absence of a pronounced and prolonged ischemic process against the background of vein thrombosis in the retina, the prognosis is favorable. If it is not possible to avoid ischemia, the likelihood of complications is high:
- neovascular glaucoma;
- recurrence of thrombosis and vitreous hemorrhage;
- traction retinal detachment.
All these pathologies lead to permanent vision loss, which even modern surgical interventions cannot correct. That is why you should not ignore the signs of partial venous obstruction in the retina: the earlier it is diagnosed, the higher the chance of avoiding vision loss.
Diagnosis of the disease
Thrombosis of the central vein of the retina is diagnosed by an ophthalmologist. In this case, you should undergo a series of studies - physical and instrumental, anamnesis, and also obtain opinions from a cardiologist, endocrinologist, rheumatologist and hematologist.
A vision test will allow you to choose the optimal treatment
To diagnose retinal thrombosis, visual acuity and level are checked, perimetry, tonometry, biomicroscopy, ophthalmoscopy, angiography to determine the condition of the vessels, and electrophysiological studies are performed.
Let's look at each of these diagnostic methods in more detail.
Testing visual acuity - visometry. At the stages of prethrombosis or occlusion of the branches, vision practically does not deteriorate. For the non-ischemic type of thrombosis of the central retinal vein and its branches, the characteristic indicator is above 0.1. In the ischemic variant, the figure is correspondingly lower than this indicator. Central and paracentral scotomas form in areas of retinal damage, and visual fields are narrowed.
Daily tonometry. With its help, when taking into account the dynamics, ocular hypertension is diagnosed.
Biomicroscopy. Shows various changes in the eyeball, such as neovascularization of the iris, relative defects of the pupil, the presence of floating blood elements and suspensions in the vitreous area.
Ophthalmoscopy. It is used to diagnose the main signs of central vein thrombosis: swelling of the optic nerve head (ONH) and macules, hemorrhages, the shape and degree of vein dilatation, microaneurysms, as well as cotton wool-type lesions.
Ophthalmoscopy is used to diagnose the main signs of thrombosis
Fluorescein angiography. Conducts diagnostics of blood vessels, delayed contrast enhancement of the retina, uneven shape of veins, granularity of blood flow. It is this study that helps determine when the disease began, its location and stage of thrombosis, the condition of the macules and optic disc.
Electroretinography. Shows the degree of ischemic damage, the development of the disease over time, and can also predict the future quality of vision.
Laboratory research. Important indicators are the presence of blood sugar, cholesterol, lipoproteins, coagulogram and factors responsible for blood clotting.
Treatment of retinal thrombosis
The treatment process for central retinal vein thrombosis has several options:
- Therapeutic effect. Determined by the stage of the disease: early options provide the opportunity for faster and more positive dynamics of treatment. First, loads are dosed, food is analyzed and further monitored, thus influencing blood pressure and changes in its indicators.
- Medication option. Its main purpose is to dissolve the blood clot that has formed a blockage in the vein. The main drugs are gomez and streptokinase, but they are more helpful for hemorrhages. It is important to use a complex of drug treatment consisting of several types of drugs:
Treatment of retinal thrombosis
- fibrinolytics to restore damaged areas;
- hypotension agents, which often causes the development of the disease. At the same time, they reduce swelling. May be in the form of injections or drops;
- vitamin preparations, especially with vitamins C and B, important in the treatment of the disease;
- hormonal agents of general and local importance, reduce swelling and inflammation;
- antiplatelet drugs to avoid recurrence of retinal thrombosis, but only if it is possible to control blood clotting;
- the use of antispasmodics and angioprotectors, in combination with other drugs, is also a common option.