Retinal drusen are yellowish-white deposits that are located in the pigment epithelium and Bruch's membrane. They are also called “Hutchinson-Tye choroiditis”, “crystalline retinal degeneration”, “familial choroiditis”, “hyaline dystrophy”, “Guttat choroiditis”, “Leventin disease”, as well as “superficial Holsous-Batten choiretinitis” or “Doine honeycomb degeneration” " It has been established that there is a significant connection between the presence of hereditary drusen and the development of age-related macular degeneration.
The term “dominant drusen” can be used only in cases where they are found in members of the same family and are confirmed during examination of young people, which indicates their hereditary nature. Drusen are inherited in an autosomal dominant manner. Most often, they are first identified between the ages of 20 and 30 years, but the literature describes rare cases of drusen occurring at the age of 8-12 years. Variability in expression and the presence of incomplete penetrance of the gene often led to genetic errors in diagnosis.
It should be borne in mind that drusen of Bruch's membrane should not be identified with drusen of the optic disc, since, despite similar ophthalmological signs, their structure is different. However, no differences were found between hereditary Bruch's membrane drusen and drusen detected during ophthalmoscopy in the presence of senile macular degeneration. This is confirmed by microscopic, histological and ultrastructural studies. Currently, ophthalmologists consider hereditary drusen as the initial stage of age-related degeneration of the macular region, which was previously called senile macular degeneration.
Patients with familial drusen are characterized by the same hereditary degenerative disease of the visual organs. It is quite often the cause of decreased visual acuity in the sixth and seventh decades of life. The number of people who contracted it in one family is quite difficult to determine due to different expression of the gene and its incomplete penetrance. Drusen most often occur in men after 50 years of age and their frequency increases with age.
Symptoms
The color is white or yellowish-pink. Over time, they undergo calcification.
Symptoms:
- swelling of the optic nerve head;
- blurred disc boundaries.
During diagnostics, shiny particles are found on the surface of the optic disc. These are the Druze.
They have a pathological effect on nervous tissue, which is characterized by a deterioration in the acuity of visual perception. Over time, the field of vision narrows, the boundaries of the blind spot expand, and arcuate scotomas appear.
Globules of mucoproteins and mucopolysaccharides are located deeply, simulating stagnation and swelling of the optic disc. Therefore, the diagnosis is often made incorrectly.
Changes occur in one or both eyes. Often the second visual organ is affected several years after the disease is diagnosed.
There are several types of drusen:
- hard - round, have clear edges, small and scattered at a far distance from each other;
- soft - large, close, blurred edges.
Soft hyaline bodies can disrupt the layers of the retina and lead to detachment of the pigment epithelium.
Retinal dystrophy - treatment, classification, symptoms
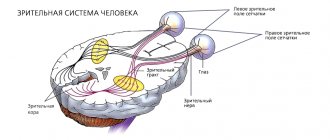
Retinal dystrophy - what is it? This question is asked by every person who has certain pathological disorders in the visual organ. In fact, this disease includes a whole group of pathologies of the retina, which is the functional structure of the eyeball. Retinal dystrophy is characterized by the death of tissue in the retina, that is, the organ begins to rapidly degenerate. The retina is considered the most important element of the visual organ, as it is responsible for visual acuity. After all, it is she who transmits light impulses to parts of the brain. It consists of a thin layer of nerve and light-sensitive cells, which are photoreceptors.
A working method to restore vision! You will throw your glasses in the trash in just 3 days...
Restoring vision. Real life story.
Classification features of retinal dystrophy
Dystrophy can be congenital or acquired. It is classified as follows:
- Peripheral retinal dystrophy occurs after injury to the visual organ. Most often it develops in the presence of congenital and acquired forms of myopia and myopia. In this case, the peripheral areas of the fundus are affected. Thus, the patient’s eye length may increase, blood circulation in the circulatory system of the eye may deteriorate, and myopia or myopia may progress. This all leads to retinal detachment and rupture. This form of the disease is very difficult to diagnose. This is due to the fact that in the initial stages the pathology is practically asymptomatic. Standard examinations by an ophthalmologist also rarely reveal peripheral dystrophy. The fact is that these particular areas are not visually visible. Therefore, there is a need for hardware examination.
- Central dystrophy is localized in the macular zone of the eye. It occurs as a result of aging, which is why it most often occurs in old age. There are two types of this form - dry and wet. The dry type is considered the most common. In this case, drusen are deposited under the nerve tissue in the form of white-yellow patches. Over time, these deposits join together to form a solid base. It prevents the visual organ from functioning normally. At the same time, retinal cells are destroyed and thinned, blood supply deteriorates, and tissues atrophy. All these pathological changes lead to loss of central vision. The form develops slowly and is characterized by damage to one eye. The wet form of central dystrophy is rarely observed. The pathology has this name due to the fact that there are frequent hemorrhages in the macula area. In this case, the capillaries begin to grow rapidly and burst. The connective tissue also increases in volume. Either one or both organs are affected simultaneously. Visual acuity deteriorates rapidly, leading to blindness. The cause of central dystrophy is age-related changes, alcohol abuse, smoking, hereditary factors, the negative effects of toxins and poor ecology.
- Retinal pigmentary dystrophy is considered the rarest form, as it is provoked by a genetic factor. In this case, there is a disruption in the functionality of photoreceptors in the nerve tissues and cells that are responsible for twilight and daytime light perception. Men are most susceptible to the disease. Symptoms can appear either rapidly or slowly. Visual acuity decreases quite a bit. Basically, the patient sees poorly in the dark.
Symptoms of retinal dystrophy
The main symptoms of retinal dystrophy:
- Blurred image of objects and partial loss of color vision.
- The presence of dark spots and spots before the eyes.
- Deterioration of lateral perception and loss of visual acuity.
- Formation of bright flashes and distortion of objects.
- The blur before the eyes and the importance of good lighting when reading.
- The patient cannot distinguish a moving object from a stationary one.
Reasons for the development of retinal dystrophy
- Pathological changes in the functionality of the retinal circulatory system, which leads to significant scarring.
- Weakened immune system and poor diet. It turns out that low-quality products can lead to retinal deformation.
- Bad habits: smoking and drinking alcohol.
- Viral infection that was not treated promptly or competently.
- Diabetes mellitus, heart disease, hypertension, pathologies of the endocrine apparatus.
- Complication after surgery.
- Poor metabolism.
How to treat retinal dystrophy, diagnosis
To make an accurate diagnosis of retinal dystrophy, a hardware examination is prescribed. This can be viziometry, ultrasound examination, perimetry, fluorescein angiography. In addition, samples for laboratory testing and instrumental examination are collected. Electrophysiological research methods are required to determine the degree of functioning of visual and nerve cells. Treatment of retinal dystrophy is carried out as comprehensively as possible and, first of all, it is drug therapy, which includes the following:
- Vasodilator and angioprotective drugs strengthen and expand the circulatory system, and also eliminate symptoms. These may be drugs such as Ascorutin, Papaverine, Complamin. The dosage and duration of treatment is determined solely at the individual level.
- Antiplatelet agents prevent the formation of blood clots. This could be Acetylsalicylic acid, Ticlopidine, Clopidogrel.
- Vitamin premixes are required.
- To improve microcirculation, Pentoxifylline is prescribed.
- Lucentis can prevent the growth of capillaries.
- Eye drops: “Taufon”, “Ophthalm-Katachrome”, “Emoxilin” and others. These drugs lead to the regeneration of damaged cells and acceleration of metabolism in the area of the visual organ.
- Electrical stimulation of the retina.
- Photostimulation of the eye.
- Low-energy laser radiation.
- Magnetotherapy, electrophoresis and so on.
Surgical intervention
In the most complex and advanced forms, surgical intervention is used. These could be the following methods:
- Laser coagulation of the retina can stop the progression of the disease. Using a laser unit, targeted cauterization of damaged tissue is performed.
- The operation can be performed using the vasoreconstructive method.
- It could also be revascularization.
- Vitrectomy involves removing the damaged areas using suction and installing an implant.
IMPORTANT! After drug therapy, you must follow all the doctor’s instructions. First of all, you should not expose your eyes to overstrain and exposure to sunlight. It is important to take additional vitamins and minerals and give up bad habits.
Notes[edit | edit code]
- Disease Ontology release 2019-05-13 — 2019-05-13 — 2020.
- Monarch Disease Ontology release 2018-06-29sonu - 2018-06-29 - 2018.
- ↑ 123
Golnik, K. (2006). Congenital anomalies and acquired abnormalities of the optic nerve, (Version 14.3). UptoDate (On-Line Serial) - ↑ 1 2 Friedman A.H., Henkind P., Gartner S.
Drusen of the optic disc. A histopathological study (English) // Eye (English) Russian. : journal. - 1975. - April (vol. 95, no. 1). - P. 4-9. - PMID 1064209. - Rosen E., Almog Y., Assia E.
(Hebrew) // Harefuah (English) Russian. - 2005. - נובמבר (vol. 144, num. 11). - P. 785-789. - PMID 16358654. - Tso MO
Pathology and pathogenesis of drusen of the optic nervehead (English) // Ophthalmology (English) Russian. : journal. - 1981. - October (vol. 88, no. 10). — P. 1066—1080. - doi:10.1016/s0161-6420(81)80038-3. - PMID 7335311. - Kapur R., Pulido JS, Abraham JL, Sharma M., Buerk B., Edward DP
Histologic findings after surgical excision of optic nerve head drusen (English) // Retina (Philadelphia, Pa.): journal. — 2008. — January (vol. 28, no. 1). - P. 143-146. - doi:10.1097/IAE.0b013e31815e98d8. - PMID 18185151. - ↑ 123456
Optic Nerve Head Drusen // Handbook of Ocular Disease Management (unspecified). - Jobson Publishing LLC, 2001. - Antcliff RJ, Spalton DJ
Are optic disc drusen inherited? (English) // Ophthalmology (English) Russian.. - 1999. - July (vol. 106, no. 7). — P. 1278—1281. - doi:10.1016/S0161-6420(99)00708-3. - PMID 10406605. - Riordan-Eva P., Hoyt WF
Neuro-ophthalmology // Vaughan & Asbury's general ophthalmology (unspecified) / John P. Whitcher; Riordan-Eva, Paul; Vaughan, Daniel; Asbury, Taylor. — 16th. - New York: Lange Medical Books/McGraw-Hill, 2004. - pp. 261-306. — ISBN 0-07-137831-6. - We are talking here about the “Caucasian race https://en.wikipedia.org/wiki/Caucasian_race”, that is, Caucasian, and not residents of the Caucasus
- OMIM 163950
- Nischal KK, Hingorani M, Bentley CR, et al.
Ocular ultrasound in Alagille syndrome: a new sign (English) // Ophthalmology (English) Russian. - 1997. - January (vol. 104, no. 1). - P. 79-85. - doi:10.1016/s0161-6420(97)30358-3. - PMID 9022108. - Spencer TS, Katz BJ, Weber SW, Digre KB
Progression from anomalous optic discs to visible optic disc drusen (English) // J Neuroophthalmol : journal. - 2004. - December (vol. 24, no. 4). - P. 297-298. - doi:10.1097/00041327-200412000-00006. - PMID 15662245. - Horton, J.
Disorders of the Eye // Harrison's principles of internal medicine (English) / Jameson JN, Kasper DL, Harrison TR, Braunwald E., Fauci AS, Hauser SL, Longo DL.. - 16th. - New York: McGraw-Hill Medical Publishing Division, 2005. - ISBN 0-07-140235-7. Archived copy from February 19, 2014 on the Wayback Machine - ↑ 1 2 Wilkins JM, Pomeranz HD
Visual manifestations of visible and buried optic disc drusen (English) // J Neuroophthalmol : journal. - 2004. - June (vol. 24, no. 2). - P. 125-129. - doi:10.1097/00041327-200406000-00006. - PMID 15179065. - Purvin V., King R., Kawasaki A., Yee R.
Anterior ischemic optic neuropathy in eyes with optic disc drusen (English) // JAMA: journal. - 2004. - January (vol. 122, no. 1). - P. 48-53. - doi:10.1001/archopht.122.1.48. - PMID 14718294. - Brodsky, MC
Ch 3: Congenital anomalies of the optic disc: Pseudopapilledema associated with optic disc drusen // Walsh and Hoyt's clinical neuro-ophthalmology (English) / Hoyt, William Graves; Miller, Neil; Walsh, Frank. — 6th. - Hagerstwon, MD: Lippincott Williams & Wilkins (English) Russian, 2005. - P. 178-187. — ISBN 0-7817-4811-9. - OMIM 127000
- OMIM 163200
- Calvo-González C., Santos-Bueso E., Díaz-Valle D., et al.
(Spanish; Castilian) // Arch Soc Esp Oftalmol. - 2006. - May (vol. 81, no. 5). - pp. 269-273. - PMID 16752318. - Grippo TM, Shihadeh WA, Schargus M, et al.
Optic nerve head drusen and visual field loss in normotensive and hypertensive eyes (English) // J. Glaucoma: journal. — 2008. — March (vol. 17, no. 2). - P. 100-104. - doi:10.1097/IJG.0b013e31814b995a. - PMID 18344754. - Delyfer MN, Rougier MB, Fourmaux E., Cousin P., Korobelnik JF
Laser photocoagulation for choroidal neovascular membrane associated with optic disc drusen (English) // Acta Ophthalmologica (English) Russian. : journal. - Wiley-Liss, 2004. - April (vol. 82, no. 2). - P. 236-238. - doi:10.1111/j.1600-0420.2004.00231.x. - PMID 15043550. - Chaudhry NA, Lavaque AJ, Shah A., Liggett PE
Photodynamic therapy for choroidal neovascular membrane secondary to optic nerve drusen // Ophthalmic Surg Lasers Imaging : journal. - 2005. - Vol. 36, no. 1. - P. 70-2. - PMID 15688974. - Sivaprasad S., Moore AT
Choroidal neovascularization in children (English) // British Journal of Ophthalmology (English) Russian - 2008. - April (vol. 92, no. 4). - P. 451-454. - doi:10.1136/bjo.2007.124586. - PMID 18369058.
Causes
Drusen of the optic disc and retina appear due to the influence of such factors:
- chronic bacterial infection;
- diabetes;
- eclampsia during childbirth;
- injuries;
- long-term inflammatory processes of the visual analyzer;
- intrauterine infections.
Today, drusen are considered as a polyetiological pathology with an unclear mechanism of development.
Diagnostics
Drusen are easy to diagnose if they are located on the surface of the optic nerve. FAGD plays an important role in diagnosis. Fluorescein angiography of the fundus does not require special preparation.
The study takes no more than 2 minutes for each organ. To carry out diagnostics, a dye is used that is easily washed off with cold water. The dye does not penetrate beyond the vessels into the surrounding tissue. It begins to fluoresce when the source of exciting light is turned on.
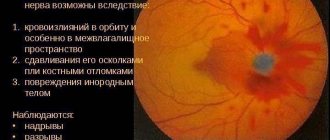
FAGD shows scalloped marginal hyperfluorescence of the disc; tissue contrast does not occur beyond its boundaries.
In some cases, during the diagnostic process, hemorrhage is detected in the retina and vitreous body.
Additionally, ultrasound and ophthalmoscopic examinations are performed. If hyaline bodies have become calcified, computed tomography is prescribed.
Visual fields are also determined to identify defects in peripheral vision.
Who can develop drusen in the optic disc?
Today, the exact cause of optic nerve drusen is unknown.
Although they are usually caused by abnormal deposits of substances of unknown origin in the optic nerve, many people with optic disc drusen claim a family history of the disorder, but this is not always the case.
Relative to age in general, it usually affects young adults and children .
Optic disc drusen
The etiology of drusen is unclear. A number of authors make assumptions about their hereditary nature. On microscopic examination, drusen are defined as deposits of hyaline in the circumference of the disc tissue and in the disc tissue. They are often localized in front of the cribriform plate of the sclera. Much less often they are located behind the cribriform plate. Sometimes (very rarely) lime is deposited in the druses.
Drusen may be present in only one eye, but are usually seen in both eyes. There are cases when the fellow eye was affected only after several years. Drusen may occur in members of the same family.
Drusen are observed in normal fundus, they can be combined with optic nerve atrophy, less often drusen are combined with retinitis pigmentosa and tuberous sclerosis. They can occur with Grönblad-Strandberg syndrome. When examining the dynamics of the disc, an increase in the number of drusen and their size is observed.
The literature indicates that disc drusen are inherited irregularly, in an autosomal dominant manner. O.I. Bessmeltseva, V.V. Volkov, A.V. Bocharova report on three patients with optic disc drusen. They believe that disc drusen is a progressive neuroopticopathy. E. Zh. Tron believed that disc drusen arise as a result of a degenerative process in the disc. It is also believed that drusen are formed due to metabolic disorders and the formation of colloidal substances - mucopolysaccharides. According to electron microscopic studies of disc drusen, prelaminar swelling and destruction of axons are determined, followed by calcium deposition and the development of shiny nodular formations, located mainly at the edges of the disc.
The mechanisms of pathogenesis of optic disc drusen remain unclear. Some doctors believe that drusen are the result of long-term pathological changes in the retinal nerve fiber layer. R. Seitz (1968), based on a histochemical study of drusen, believes that drusen are formed from axoplasmic derivatives during a slow destructive process in the nerve fibers of the disc area. Electron microscopic studies indicate prelaminar swelling, destruction and death of axons, which leads to the development of drusen. However, S. Vause et al. (1978), based on pathohistological studies of 52 eyes with drusen, using a set of special methods for staining preparations, were unable to identify primary degenerative changes in nerve fibers (axons). They do not confirm the hypothesis that the etiological basis for the formation of drusen is the products of destructive processes occurring in axons.
Clinical picture. Ophthalmoscopically, multiple small roundish grayish lesions are detected around the optic nerve head. At the same time, they protrude above the level of the disk. More often they are localized in the marginal zone of the disc, but rarely they are found on the disc, somewhat short of the exit point of the central vessels of the disc.
Visual functions with optic nerve drusen are, as a rule, not impaired. In some cases, a concentric narrowing of the visual field and the presence of paracentral scotomas may be detected due to compression of the optic nerve fibers by disc drusen. This is especially true in cases where disc drusen are located deep in the area of the sclerochoroidal canal. Scotomas in the field of view are detected by campimetry or static computer perimetry. Visual acuity is usually not affected. Patients with disc drusen and visual field abnormalities are subject to systematic monitoring.
Clinical observations indicate that drusen appear first at the edges of the disc and are more likely to occur in a narrow scleral canal, where the nerve fibers are more compressed by the ring of this canal.
A. M. Vodovozov proposed a classification of drusen: hidden, deep, obvious and amputated. The ophthalmoscopic picture with hidden drusen is expressed by unclear boundaries, sometimes scalloped disc boundaries, protrusion of the disc towards the vitreous body up to 1 mm, expansion and tortuosity of the retinal veins. In such cases, the ophthalmoscopic picture is very similar to congestive optic discs. With obvious drusen, round, whitish, shiny formations are revealed on the disc. Disc changes are usually bilateral, but drusen are often more severe in one eye. In such patients, the diagnosis of drusen is not difficult. Over time, hidden drusen become obvious.
Data from L. Frisen et al., who used computed tomography, showed that the diameter of the optic nerve in the retrobulbar region with drusen remains normal. This fact is a significant differential diagnostic feature in the initial symptoms of a congestive disc, in which an increase in the diameter of the retrobulbar (distal) part of the optic nerve is observed.
In childhood, drusen are often hidden under the surface of the optic disc tissue, resembling the picture of the initial manifestations of a congestive disc. With age, these hidden drusen may become obvious. According to W. Spencer, in many cases drusen are familial and hereditary in nature, and he recommends that parents of children with drusen be examined.
Diagnostics. With ophthalmoscopy, laser ophthalmology and chromoophthalmoscopy, the diagnosis of superficially located drusen of the optic nerve is relatively easy. However, it turns out to be more difficult with drusen located deep in the tissues of the disc, the so-called hidden drusen. In such cases, the methods of ultrasound B-scan and fluorescein angiography help in correct diagnosis. In the differential diagnosis of optic nerve drusen, it is necessary to exclude the initial manifestations of a congestive disc, optic neuritis and pseudoneuritis.
In rare cases, when it is necessary to make a differential diagnosis between optic nerve drusen and papilledema, fluorescein angiography helps. Fluorescein angiogram of optic nerve drusen shows marginal scalloped hyperfluorescence. In this case, there is no contrasting of tissues outside the disc. There are no changes in the papillary and retinal vessels. With disc edema, contrasting tissue outside the disc occurs against the background of changes in the retinal and papillary vessels.
One of the differential diagnostic signs between optic disc drusen and initial congestive optic disc is the fact, as a rule, of bilateral changes in the discs during congestion. With disc drusen, its changes can be unilateral. Sometimes the fellow eye is affected only after several years. Moreover, with long-term follow-up, an increase in the number of disc drusen may be noted. Drusen, clearly visible ophthalmoscopically, are most often located in front of the cribriform plate. The so-called hidden drusen, which are more difficult to diagnose, are often located behind the cribriform plate. Sometimes lime is deposited in the drusen, which does not occur with stagnant discs.
In cases of hidden disc drusen, fluorescein angiography of the fundus is of great importance. According to R. O. Mukhamadiev, no clear hemodynamic disturbances are detected in the retinal vessels with disc drusen. The optic disc fluoresces unevenly: the fluorescence of the disc is in some places enhanced, in others weakened. Against the background of uneven fluorescence, round white formations - drusen - are revealed. As fluorescein disappears from the retinal veins, disc fluorescence also fades. At the same time, disc drusen are brightly stained with fluorescein. Drusen sometimes cause local swelling of the disc only in certain areas, which is manifested by residual fluorescence of the disc.
Optic disc drusen have the special property of fluorescing at the same wavelength as fluorescein. Therefore, they can be photographed without intravenous fluorescein using filters such as those used in fluorescein angiography. This is the so-called true autofluorescence of drusen. With intravenous administration of a 10% fluorescein solution, drusen retain and accumulate it. In this case, late staining of drusen with fluorescein occurs. No bleeding of dye from drusen is observed. Fluorescence of drusen is well detected in the early prearterial phase.
Thus, fluorescein angiography of the fundus for disc drusen in a single examination makes it possible to completely exclude congestive optic disc.
For the purpose of differential diagnosis between congestive disc and optic disc drusen, E. E. Ioileva, P. F. Linnik, A. A. Shpak examined 38 patients with bilateral optic disc protrusion of varying degrees of severity. For the study, a diagnostic system was used based on computerized digital analysis of fundus images to obtain calorimetric measurements of the intraocular part of the optic nerve. As a result of studies, congestive optic disc was identified in 29 patients. Pseudocongestive optic disc caused by drusen was identified in 9 patients.
With disc drusen, according to computed tomography and ultrasound, the diameter of the optic nerve in its retrobulbar region remains within normal limits, in contrast to a stagnant disc in brain tumors, in which the diameter of the optic nerve is increased.
Treatment of optic nerve drusen is not effective and is not carried out. The prognosis for vision is favorable.
Announcement of an article on the topic of health - What to do if you have leg cramps
... Stretching the calf muscle can help relieve severe pain. To do this, you need to perform a gentle massage that will stimulate blood flow to the muscle tissue. Relief will come if you sit on the floor, stretch your legs and try to pull your feet towards your face; if pain prevents this, you can help pull your feet up with your hands.
Announcement of an article on the topic of health - Kinematics and dynamics of the foot when walking
... When walking, a person consistently leans on one leg or the other. This leg is called the supporting leg. The contralateral (opposite) leg is brought forward at this moment (This is the portable leg). The period of swinging the leg is called the “swing phase.” The full gait cycle—the double step period—is composed of the support phase and the swing phase for each leg. During the support period, the active muscular effort of the limbs creates dynamic shocks that impart to the center of gravity of the body the acceleration necessary for forward movement. When walking at an average pace, the stance phase lasts approximately 60% of the double step cycle, the stance phase approximately 40%. Let's consider the most common movements of the body in the sagittal plane during the double step. The beginning of a double step is considered to be the moment of contact of the heel with the support. Normally, the heel lands on its outer part. From this moment on, this (right) leg is considered the supporting leg. Otherwise, this phase of walking is called the front push - the result of the interaction of the force of gravity of the moving person with the support. In this case, a support reaction occurs on the plane of support; the vertical component of the cortex exceeds the mass of the human body.
Announcement of an article on the topic of health - What foods stain tooth enamel
... After drinking beets or beet juice, immediately brush your teeth, or at least rinse your mouth. Beets contain a large number of chromogens that have a coloring effect.
Differential diagnosis
Yellowish or whitish deposits located in the posterior pole of the eyeball can be observed not only in the presence of dominant drusen, but also in the case of some other diseases that belong to the flecked retina syndrome.
Thus, fundus punctatus albescens, or white-spot abiotrophy of the fundus, is a disease in which white spots, very similar to drusen, are identified in the middle periphery of the fundus. With this disease, visual acuity sharply decreases and progressive nyctalopia occurs. It is similar to mild early forms of retinal pigment abiotrophy.
Fundus albipunctatus, or fundus albipunctatus, is a bilateral hereditary disease, which in its ophthalmoscopic picture is similar to both the previous disease and hereditary drusen. It occurs without a decrease in visual acuity, has a non-progressive course and permanent night blindness. During ophthalmoscopy, you can detect whitish dotted spots of the same shape, rounded, located at the level of the pigment epithelium. They occupy a large area of the fundus of the eye. The area of maximum location is the equatorial and macular zone. In contrast to fundus albipunctatus, the size of dominant drusen is more variable, and they are more dominant in the macular area.
Fundus flavimaculatus, or fundus flavimaculatus, is a bilateral disease. It, in contrast to round, smooth dominant drusen with clear boundaries, is manifested by yellowish deposits located in the form of spots at the level of the pigment epithelium. Angiography often reveals blockade of choroidal fluorescence in the posterior field and in the periphery, which never occurs with dominant hereditary drusen. Fundus flavimaculatus is often associated with macular degeneration, which occurs in a bull's-eye pattern, which never occurs with hereditary drusen. When this disease is combined with Stargardt disease, visual acuity decreases. Also, in the presence of fundus flavimaculatus, a narrowing of the visual field is detected, which is not typical for drusen.
Crystallin dystrophy, or Bietti's dystrophy, is also characterized by the presence of whitish deposits on the retina. They, unlike dominant drusen, are localized in all layers of the retina, are polygonal in shape and have a “diamond-white” luster. With this disease, marginal corneal dystrophy develops and visual functions progressively decrease.