Structure of the optic nerve
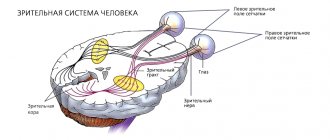
The human optic nerve contains more than a million nerve cell projections that transmit information from the retina to the brain and provide vision. The transformation of information occurs in the occipital lobe of the brain. This is where response signals are generated.
The optic nerve originates from the disc (head) in the eyeball and runs through the tissues of the orbit. Once in the cranial cavity, the optic nerves from different eyes connect and then run as part of another structure.
The nerve is covered with several membranes, which allows for high-speed conduction of impulses, as well as protection and nutrition of the element. The membranes and intrathecal space have a connection with the brain; accordingly, when the latter is inflamed, the optic nerve can be affected.
Depending on the damaged part of the optic nerve, ordinary neuritis (inflammation of the intraocular part), retrobulbar (damage to parts that lie outside the eye) and papillitis (mixed pathology) are distinguished.
Forms of neuritis:
- Peripheral. Exudate accumulates in the subdural and subarachnoid (between the hard and soft membrane) spaces of the optic nerve.
- Axial. Inflammation is localized in the axial bundle (central nerves). This form of neuritis is most often diagnosed.
- Transversal. The most severe form of neuritis, which provokes severe dysfunction of the visual apparatus. Inflammation spreads from the axial fascicle to the rest of the nerve.
Types of neuritis
There are different types of symptoms, which depend solely on the location of the lesion (central or peripheral lobe). In neurology, retrobulbar neuritis is divided into three classes:
- Axial - a common form of inflammatory reaction, localized only in the axial fascicle, characterized by a sharp decrease in central visual acuity and the appearance of scotomas.
- Peripheral - originates in peripheral structures, accompanied by the formation of intrathecal fluid, which provokes pain. A narrowing of the optical fields is characteristic.
- Transversal - a detrimental anomaly progresses in the periphery or axial region and then reaches the diameter of the nerve center. The patient is completely blind.
Another area of division of retrobulbar neuritis depends on the variability of the course:
- Acute form - manifests itself in the rapid loss of visual acuity. Most often it is diagnosed in the primary version of the lesion, which is typical for young people.
- Chronic form - symptoms have a gradual scale of increase, which are caused by a cerebral disorder. Patients experience some periods of remission or exacerbation. There is a possibility of the acute form becoming chronic.
Features of retrobulbar neuritis
Retrobulbar neuritis is an inflammatory process that affects the nerve fibers of the optic nerve outside the eyeball. A characteristic feature of the pathology is a gradual depression of visual function.
Most often, this form of neuritis is diagnosed in patients 25-35 years old. Retrobulbar neuritis is believed to be an early sign of multiple sclerosis.
Typically, retrobulbar neuritis develops against the background of existing inflammation of any localization. Unfavorable external and internal factors provoke demineralization and inflammation of the nerve fibers that line the optic nerve. Without treatment, inflammation gradually atrophies the fibers, which causes a decrease in visual acuity.
It is noteworthy that specifically in retrobulbar neuritis, the optic disc is not involved in the inflammatory process; destruction occurs outside the eyeball. Nerve inflammation is manifested by cell proliferation (division) and pinpoint infiltration (penetration of abnormal cells into healthy tissue). Inflammation begins from the pia mater, moving to the nerve fibers.
When the process is localized in the nerve trunk, the inflammation is nonspecific. Swelling and infiltration develop, many vessels and connective tissue are formed. Atrophy of nerve fibers occurs secondary. After treatment, the functionality of the affected area can be restored, and accordingly, visual acuity will improve.
Factors causing retrobulbar neuritis
Various problems provoke the development of abnormal vision impairment. Inflammation itself begins as a result of damage to the body by infectious diseases, chronic diseases caused by immunodeficiency. Etiological reasons include:
- Chronic stages of viral infections - the main causative agent is cytomegalovirus, which provokes the development of mononucleosis. The stable location of harmful agents causes deformations in immune properties. Due to the production of antibodies for one's own tissues, the process of autoimmune inflammation begins.
- Chronic infectious points - most often the anomaly is caused by unfavorable foci that are located nearby (for example, sinusitis, otitis media and others), much less often - by distant places (cystitis). The infection enters the nervous structure of the visual apparatus through blood transportation.
- Inflammatory phenomena in the orbit - provocateurs are inflammatory processes. Spread occurs in two ways: hematogenous and perineural, which causes damage to the retrobulbar perimeter of the nerve. Quite often, total optic neuritis is diagnosed.
Secondary progression of optic nerve disorder begins as a result of an anomaly that is localized in the cerebral region. The main etiofactors include the following diseases:
- Multiple sclerosis - selective damage to the myelin sheath of nerve fibers moves to the optical areas, which causes an inflammatory reaction. Neuritis of a retrobulbar nature is considered the initial stage in more than 65% of cases of disease.
- Brain tumors - when voluminous tumors form in the area of the chiasm glioma, objects in another place begin to actively pressure the optic chiasm, disrupting the process of blood circulation in the body and metabolism in tissues. As a result, the patient develops symptoms of neuritis.
- Neuroinfections - Lyme disease, neuroAIDS, tuberculous meningitis can provoke abnormalities in the retrobulbar zone. Inflammatory phenomena are associated with the entry of infectious microorganisms into the body. In some cases, the disease may appear due to intoxication. Exogenous lesions are caused by the influence of toxic chemicals, methyl alcohol, iodine substances. Toxins appear as a result of dysmetabolic processes, renal failure or during pregnancy.
Causes of inflammation of the optic nerve
As a rule, the progression of retrobulbar neuritis is associated with the development of multiple sclerosis: this pathology primarily provokes inflammation of the nerves. However, there are other causes of neuritis, so diagnosis plays a critical role in the process of choosing therapy.
It happens that it is not possible to reliably establish the cause of neuritis. In this case, they speak of an idiopathic (independent) form of neuritis.
Causes of retrobulbar neuritis:
- head injuries;
- brain pathologies;
- inflammation of the membranes of the eye and orbit;
- infectious and non-infectious lesions of the lining of the brain (encephalitis, meningitis);
- pathological pregnancy;
- chronic diseases (diabetes mellitus, gout, nephritis);
- viral and infectious pathologies (tuberculosis, brucellosis, typhus, malaria, smallpox, syphilis, influenza, tonsillitis, otitis media, sinusitis, tonsillitis, erysipelas);
- multiple sclerosis.
Intoxication of the body aggravates the course of neuritis. This applies to drugs, alcohol and some medications.
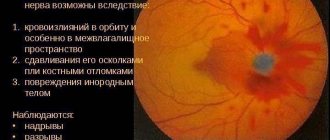
Symptoms of acute and chronic retrobulbar neuritis
At the initial stage of retrobulbar neuritis, the fundus of the eye may not be deformed, but most often there is hyperemia and distortion of the boundaries of the optic nerve head. Retrobulbar neuritis typically affects only one eye, but the disease can spread to the second. Simultaneous inflammation of both eyes is rarely diagnosed.
With this type of nerve inflammation, a central scotoma (blind area) occurs. Initially, the spot is large, but gradually decreases with adequate treatment. Sometimes the central scotoma turns into a paracentral annular scotoma.
The severity of neuritis symptoms is determined by the extent of inflammation. Typically, acute and chronic forms of neuritis are distinguished.
In acute pathology, a few days are enough for symptoms to develop. A person experiences visual discomfort and a sharp decrease in visual acuity occurs. In acute neuritis, the pain intensifies from pressing the eyeball into the orbit.
The acute form of neuritis also causes impaired color vision and acute pain when moving the eyes. In severe cases, pain persists even at rest. Visual acuity usually returns after treatment, but in rare cases the eye remains almost completely blind.
Chronic neuritis is characterized by gradual depression of visual function. The clinical picture is not expressed. As the disease progresses, a blind spot may appear in the field of vision, and patients complain of a feeling of blurred vision.
In addition, chronic neuritis is accompanied by nausea and vomiting, visual illusions, and general weakness. Symptoms will intensify as the disease progresses and after physical activity. People with neuritis should also avoid worries and stress.
Retrobulbar neuritis caused by diabetes mellitus is usually chronic. The disease is more common in men and affects both eyes. Vision is slowly depressed, and absolute or relative central scotomas appear.
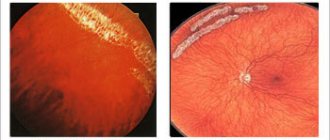
Signs of retrobulbar optic neuritis
Like other diseases, optic neuritis can be acute or chronic. In the acute form of retrobulbar optic neuritis, symptoms clearly appear within a couple of days. The patient experiences severe pain, which intensifies with eye movement, and visual acuity decreases. In this case, problems appear with the perception of certain colors. Typically, pathological processes develop in one eye, and over time they move to the second. In some cases, swelling and hyperemia also occur. In the chronic form, visual acuity decreases gradually.
Over time, the optic nerve atrophies, causing a blind spot to appear in the center of the eye. It occurs in 60% of cases. According to patients, it seems as if everything around is in twilight, sometimes dots and figures appear that do not actually exist. Red eyes, nausea, and headaches may also occur. Sometimes double vision and nystagmus (involuntary movements) are also observed. It is often difficult for the patient to control the position of the head.
All symptoms can be much brighter if there is emotional or physical stress. The signs common to both forms of retrobulbar neuritis are:
- gradual decrease in visual acuity;
- increased sensitivity of the retina;
- pain in the eyes;
- discomfort in bright light.
In each patient, all these symptoms manifest themselves with different strength: sometimes vision may deteriorate only slightly, in other cases blindness develops when the patient sees only light. The latter is most often recorded in axial and transversal retrobulbar optic neuritis.
The most severe eye pain occurs in the peripheral form of the disease. It is worth noting that patients themselves rarely indicate problems with color perception: this symptom of neuritis is detected during a medical examination.
The severity of symptoms depends on where the optic nerve is affected.
Clinical picture of toxic neuritis
The clinical picture of retrobulbar neuritis, which is caused by intoxication, has some of its own characteristics. The most common cause is poisoning with methyl alcohol and mixtures containing it.
In mild poisoning, only nausea and vomiting are observed, in severe cases - unconsciousness. After a few days, vision begins to deteriorate (up to complete blindness). On examination, the pupil is dilated and the reaction to light is weakened. The fundus is not deformed, although symptoms of ischemic neuritis may appear. Without treatment within a month, visual acuity may be restored, but with subsequent deterioration.
Alcohol and tobacco intoxication develops with chronic alcoholism and abuse of strong varieties of tobacco. Neuritis affecting the papillomacular bundle is diagnosed mainly in men over 30 years of age. The course of inflammation is similar to retrobulbar neuritis: mild hyperemia of the disc, the presence of a central scotoma. It is possible to improve visual acuity by giving up bad habits.
Classification of neuritis
Optic neuritis is classified according to the clinical picture that appears. The decisive points in dividing the disease into types are the causes of its occurrence and the source of inflammation.
Depending on the causes of optic neuritis, the following types are distinguished:
- Infectious.
- Parainfectious. Manifests itself as a consequence of viral diseases or the administration of vaccines.
- Demyelinating. The cause of the pathology is the destruction of the membrane of neurons.
- Ischemic. The result of disturbances in cerebral circulation.
- Toxic. Consequences after poisoning with methyl alcohol.
- Autoimmune. Occurs due to impaired immune functions.
If we take into account the area of damage to the optic nerve, then neuritis can be divided into intrabulbar and retrobulbar. The first of them extends to the optic nerve head. Most often, this deviation is observed in children. Retrobulbar neuritis is the result of untimely treatment. It manifests itself as inflammation of the nerve fibers located in the deeper layers of the eye.
In addition, the following types of neuritis are distinguished:
- Orbital. Inflammation penetrates into the eye socket.
- Transverse. All tissues of the optic nerve are affected.
- Papillitis. Damage to the optic nerve head in the early stages. Accompanied by hemorrhage.
- Neuroretinitis. The fibrous layer of the retina becomes inflamed.
- Interstitial. Accompanied by inflammation of auxiliary nerve cells and connective tissue.
- Axial. Those parts of the nervous system that are located directly behind the eyeball are affected.
As we see, optic neuritis has many varieties. Therefore, it is very difficult to establish an accurate diagnosis. The causes and symptoms of the pathology can provide significant assistance in diagnosing the disease. If neuritis is not treated in time, serious consequences are possible. Some of them can be found in this commentary:
Diagnosis of retrobulbar neuritis
Any manifestations of retrobulbar neuritis are a good reason to consult an experienced doctor and undergo a full examination. It is very important to make an accurate diagnosis and study in more detail the specifics of the development of the disease in a particular patient. Before choosing a treatment method, you need to find out the cause of the neuritis.
Typically the examination includes the following procedures:
- ophthalmological examination;
- visometry (determining visual acuity);
- light perception test;
- ophthalmoscopy (examination of the fundus of the eye);
- additional tests that help examine the reaction of the visual system to visual stimuli and determine the conduction speed of nerve impulses.
Magnetic resonance scanning is considered the most informative method for diagnosing optic neuritis. The procedure consists of obtaining images of the optic nerve with the preliminary introduction of a special contrast agent into it. MRI is a safe procedure and allows for detailed examination of the optic fiber.
Diagnosis of the disease
In the early stages, it is very difficult to detect optic neuritis. The appearance of the first signs of the disease is a signal that you need to visit a doctor. Based on your complaints and symptoms, the ophthalmologist will conduct research and make a diagnosis. The following diagnostic methods will be used:
- Testing visual acuity and ability to distinguish colors.
- Study of the structure of the fundus using ophthalmoscopy.
- Tracking the reaction to a light stimulus.
- Blood analysis.
- MRI of the brain.
- Ultrasound of the eye.
During the diagnostic process, the cause of the disease and the degree of its manifestation are identified. This helps to create a more accurate clinical picture and prescribe systematic treatment.
Differential diagnosis of neuritis
Diagnosis of typical cases of retrobulbar neuritis is quite simple; it is more difficult to identify mild forms of inflammation that do not affect visual abilities, and swelling of the optic nerve. The most difficult part of the diagnosis is to rule out edema and congestive disc complications. Both of these conditions, like neuritis, are accompanied by a decrease in visual acuity.
Differential diagnosis consists of excluding pseudoneuritis and optic disc congestion. In the case of pseudoneuritis, vision does not deteriorate, there is no progression of the condition. The initial stage of a stagnant disc is also characterized by preservation of vision and partial marginal swelling of the nerve disc. As the disease progresses, intracranial pressure increases.
Differentiation of retrobulbar neuritis from ordinary neuritis occurs by assessing the condition of the disc and checking visual acuity. Sharp blindness, the presence of a central scotoma and minor changes in the disc indicate a retrobulbar type of inflammation.
First aid for retrobulbar neuritis
Before determining the cause of retrobulbar neuritis, antibacterial and anti-inflammatory therapy should be carried out. Urgent desensitization, dehydration, correction of immunity and measures to improve metabolism in the tissues of the central nervous system are prescribed.
Broad-spectrum antibiotics are prescribed by injection for a week. Do not use ototoxic drugs (Streptomycin, Gentamicin, Neomycin), which have a negative effect on the optic nerve. Corticosteroids are considered safe: Dexamethasone 1 ml every day (10-15 procedures), Prednisolone 0.005 g (4-6 times a day) for five days.
Therapy for retrobulbar neuritis:
- Diacab (Acetazolamide). 0.25 g of the drug 2-3 times a day. The course of treatment is three days. In parallel, Panangin is prescribed two tablets three times a day.
- Glycerol. 1-1.5 g/kg.
- Magnesium sulfate 25%. Intramuscularly 10 ml.
- Glucose 40% intravenously and Solcoseryl (Actovegin) intramuscularly.
- Hexamethylenetetramine solution 40%.
- Adrenaline solution 0.1%. Tampons in the middle nasal passage for 20 minutes.
- Piracetam (Nootropil). Up to 12 g/day.
- Dibazol. 10 mg twice a day for 2-3 months.
Similar therapy is indicated for bilateral toxic neuritis, which developed against the background of methyl alcohol poisoning. Only antibiotics are excluded.
How to treat retrobulbar neuritis
Therapy for inflammation of the optic nerve has a favorable prognosis only if it is started on time. If the disease is ignored, severe complications can develop, including multiple sclerosis and even complete loss of vision.
Retrobulbar neuritis requires hospitalization of the patient. Inpatient treatment helps to avoid complications. If multiple sclerosis is suspected, the patient must be admitted to a hospital. Only constant monitoring of the patient’s condition and timely adjustments to the treatment plan guarantee complete recovery.
The course of treatment for neuritis should be determined by the doctor depending on the cause of the development of the pathology. In cases where the cause has not been established, complex anti-inflammatory therapy is recommended. It is very important to stop the spread of the process and promote the restoration of the affected fibers.
Drugs for the treatment of retrobulbar neuritis:
- anti-inflammatory;
- antihistamines;
- antiviral;
- antibacterial;
- hormonal (for local use);
- vitamin supplements (especially group B).
It is recommended to combine drug therapy and physiotherapy. To eliminate inflammation of the optic nerve, magnetic therapy and laser stimulation are used.
Noticeable improvement occurs only after a month of regular treatment. In severe cases, regression of inflammation can only be achieved through surgery. The procedure involves opening the nerve sheath, which helps relieve pressure on its fibers. However, neuritis requiring surgery is extremely rare. As a rule, conservative therapy is effective.
After determining the etiology of neuritis, drugs are added to treat the cause. This could be specific therapy for tuberculosis, drugs for herpes, surgical relief of sinusitis.
Retrobulbar optic neuritis: treatment
The treatment regimen for retrobulbar optic neuritis depends on the cause of its development. If it has not been established, then complex therapy is used. Treatment is carried out after hospitalization: this way the specialist can fully monitor the patient’s condition and adjust therapy based on it.
If the cause of bulbar neuritis is a viral infection, then the course of treatment includes taking antiviral drugs. For bacterial infections, antibiotics are used. In parallel with this, antihistamines are used. In the presence of poisoning, unpleasant symptoms are relieved with detoxification drugs.
To relieve inflammation and swelling, glucocorticosteroids are prescribed, for example, the drugs Prednisolone, Dexamethasone. In cases where visual function is impaired, medications can be administered behind the eyeball using a syringe.
In addition, patients are advised to normalize their diet and take vitamins PP, B1, B6 - they improve metabolism. Saturation of the brain and optic nerve with oxygen is facilitated by taking drugs such as Actovegin and Trental.
Cholinesterase inhibitors, including Neuromidin, help improve the transmission of nerve impulses.
If retrobulbar neuritis occurs against the background of multiple sclerosis, then interferons and immunosuppressants are used.
At the recovery stage, you can use folk remedies. One of them is an infusion of medicinal plants. To prepare it, you need to put a few aloe leaves in the refrigerator. A few days later they are cleaned and crushed, 5 grams of eyebright, cornflower flowers, and 200 grams of honey are added to them. The mixture is poured into a bottle of dry wine, heated for 40 minutes in a water bath and filtered. You need to take this medicine one tablespoon before meals every day. Before taking traditional medicine, consult your doctor. Do not use any decoctions or infusions without his approval.
Consequences of retrobulbar neuritis
Most often, pathological changes caused by inflammation of the optic nerve can be reversed. In most patients, visual function is restored almost completely within a year.
However, in cases where inflammation appears against the background of neuromyelitis or multiple sclerosis, the risk of relapse of neuritis increases. It is noteworthy that 70% of women who have had retrobulbar optic neuritis subsequently develop multiple sclerosis. In the absence of these or similar pathologies, the chances of re-inflammation are minimal.
Causes of optic neuritis
The causes of this disease are still poorly understood. According to the results of one study, the main factor provoking the development of retrobulbar optic neuritis is genetics. Because of this predisposition, myelin proteins are mistakenly perceived as harmful, resulting in the accumulation of T cells and activation of immune defenses.
The risk of developing the disease is highest at a young age: the first symptoms occur in patients under 30 years of age. Retrobulbar neuritis appears especially often in women. Among the reasons that provoke the development of the disease are infectious and non-infectious factors. Primary inflammation can occur due to viral infections: herpes, infectious mononucleosis, etc. In addition, it can be caused by tonsillitis, tonsillitis and sinusitis. A separate group of diseases that cause inflammation of the optic nerve includes uveitis and chorioretinitis.
If there has been brain damage, secondary retrobulbar neuritis may occur. It can occur due to HIV infection, Lyme disease, and inflammation of the brain.
The vast majority of people with multiple sclerosis are diagnosed with secondary bulbar neuritis, which occurs due to a lack of myelin. At the same time, at first, atrophic processes in the myelin sheath are invisible: they can be difficult to detect even on MRI.
Signs of myelin atrophy are noticed approximately 5 years after the onset of the disease. In 50% of patients, demyelination of both visual pathways is noticed in the images; in approximately 37%, the process is noticeable only on one side; in the remaining patients, both pathways are intact.
Prevention of inflammation of the optic nerve
To avoid toxic neuritis, you need to give up bad habits, or reduce the amount of alcohol consumed and replace strong cigarettes with light ones. You also need to protect yourself from toxic liquids.
Since inflammation of the optic nerve develops for various reasons, prevention must be comprehensive. It is important to complete treatment of acute forms of pathologies and control chronic ones.
Retrobulbar neuritis may resolve on its own, but there is an increased risk of nerve atrophy and complete blindness in one or both eyes. If any symptoms occur, you should immediately undergo examination and consult with an experienced specialist.
Sources used:
- How to remove glasses forever / Ruschel Blavo. - M.: Ripol Classic, 2011.
- Physiology and pathology of the retina: Primary mechanisms of vision / G.G. Demircioglyan. — M.: Medicine
- Ophthalmopharmacology. Guide for doctors: monograph. / E.A. Egorov, Yu.S. Astakhov, T.V. Stavitskaya. - Moscow
- Kazan State Medical University