Causes of accommodation paresis
The causes of this process are associated with pathological conditions of the eyes. Anterior uveitis, glaucoma and iridocyclitis lead to weakening of the ciliary muscle. Infections that can cause paresis:
- flu;
- diphtheria;
- Infectious mononucleosis;
- tuberculosis;
- meningitis;
- encephalitis;
- syphilis;
- botulinum toxin;
- fungal spores.
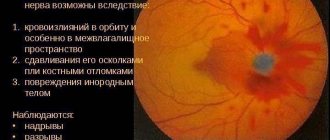
Also, the etiology is due to damage to the oculomotor nerve (3rd pair of cranial nerves) due to hemorrhage or tumor (glioma).
The cause may be optic disc edema (develops as a result of a persistent increase in intracranial pressure), trigeminal neuralgia, Adi-Holmes syndrome (ciliary muscle dysfunction), ciliary body aplasia, partial subluxation of the lens, myotonic dystrophy, pineal tumor and Guy-Wernicke syndrome.
Some medications can also cause weakness. For example, Atropine leads to this condition by disrupting the conduction of nerve impulses.
The causes of peripheral weakening are toxic, mechanical conditions and atrophy of the ciliary muscle.
Features of the course and treatment of oculomotor nerve paresis
The combination of neurological pathologies of the visual apparatus poses a great danger to humans, so it is important to monitor not only the state of vision, but also the health of the eye itself. One of the most serious diseases in this regard is paresis of the oculomotor nerve, which causes paralysis of the eyeball and other complications. In turn, the problem can only be a symptom of other diseases. It is difficult to treat and stop, so when you detect the first signs of a disorder, it is important to consult a doctor as soon as possible.
Symptoms of incomplete paralysis of accommodation
At school age, persistent paralysis develops between the ages of 7 and 15 years. More often caused by stressful situations at home or school.
An important accompanying symptom is the expansion of the pupil. The worse the disorder, the more dilated the pupil. Along with this, there are signs of a basal process.
Symptoms are accompanied by the appearance of asthenopic complaints, cephalgia and increased sensitivity to light. Accommodation paresis is characterized by persistent muscle tension, which persists even at rest.
Other signs:
- involuntary tonic tension of the ciliary muscle;
- a sharp decrease in relative accommodation reserves;
- unstable position of the nearest or farthest points of clear vision;
- redness of the eyeballs;
- reading difficulties;
- squinting when necessary to look at objects located at a far distance.
The disease occurs on both organs of vision simultaneously.
Diagnostics
The diagnosis is made by a neurologist and ophthalmologist. An optometrist at an optical salon can also determine paresis. The examination includes:
- determination of visual acuity;
- fundus examination;
- refractometry;
- measuring the fluid pressure inside the eye.
Differential diagnosis with the involvement of specialists is intended to identify or exclude optic neuritis or its infiltration in glioma and sarcoidosis, cavernous sinus thrombosis or Chiari syndrome, Foster-Kennedy syndrome, drug intoxication, Lyme disease (with increased intracranial pressure), medulloblastoma or lymphoblastic leukemia.
Treatment
Special exercises and physical therapy
Gymnastics for the eyes is carried out in combination with exercises and massage for other parts of the back, as well as the head and temples. It allows you to restore the muscle frame.
Gymnastics for the eyes strengthens the ciliary muscle, allowing the eye to adapt faster. Special exercises help adjust the level of curvature of the lens.
Physiotherapy is carried out after relief of the signs and causes of the disease. It allows drugs to better penetrate tissues.
Eye drops
Medicines relieve spasms. Prescribed:
- Cyclomed;
- Atropine.
Medicines dilate the pupil. Sometimes Irifrin is used, which relaxes the ciliary muscle as much as possible.
The course of treatment and dosage is determined by an ophthalmologist after a comprehensive examination of the patient’s eyes and determining the cause. Sometimes it is enough for a patient to use eye drops for 1 week to obtain a positive effect.
Treatment is carried out in combination with exercises and physiotherapy, since eye drops provide short-term results.
Surgical intervention
The operation is performed if the disease has led to myopia, which is difficult to correct with glasses or lenses and the patient constantly has to use vision correction devices.
Oculomotor abducens palsy in children
A person is able to move the eyeball thanks to 3 cranial nerve pathways. The main role in this process is played by the oculomotor nerve, which goes under number 3. It is responsible for the movements of the eyelid and eye, as well as its reaction to exposure to light. The abducens nerve controls the abduction of the eyeball, and the trochlear nerve turns it outward and downward. These nerve pathways are numbered 6 and 4.
Any disturbances in the innervation of the extraocular muscles affect the ability to see fully. Among such disorders, paresis of the eye muscles in children can be identified, since, in addition to the main causes that are characteristic of adults, they often exhibit congenital anomalies. Treatment is usually carried out using a whole range of procedures; in especially severe cases, surgery is used.
Causes and symptoms
Abducens nerve palsy manifests itself as isolated paralysis. In this case, a person cannot fully avert his eyes and a double image of one object appears (diplopia).
This phenomenon occurs due to a violation of the innervation of the lateral muscle, for which the abducens nerve is responsible.
Similar symptoms are characteristic of diseases of the orbit, so you should undergo detailed diagnostics to make a diagnosis.
The abducens nerve is damaged due to the following factors:
- Aneurysm;
- Damage to the carotid artery;
- Traumatic brain injuries;
- Infectious diseases;
- Oncological diseases;
- Microinfarctions and strokes;
- Pathologies of the nervous system;
- Multiple sclerosis.
The abducens nerve in children is also injured due to the above factors. However, other reasons are also common for children:
- Gradenigo syndrome;
- Mobius syndrome;
- Duane's syndrome.
Damage to the trochlear nerve causes partial paralysis of the eye and the person has a double image in an oblique or vertical plane.
This symptom intensifies when the eye is lowered down, so people suffering from this pathology often walk with their heads tilted to the healthy side to reduce the manifestation of diplopia.
During diagnosis, myasthenia gravis (autoimmune pathology of nerve and muscle tissue) and diseases of the orbit should be excluded.
Oculomotor nerve palsy usually occurs in conjunction with disruptions of the facial, abducens, and trochlear nerve pathways. A separate form of pathology appears extremely rarely. This nerve is damaged primarily due to an aneurysm. It arises on the posterior communicating artery and gradually compresses the nervous tissue.
The nerve can be damaged by a growing tumor, as well as manifestations of stroke and multiple sclerosis. In most cases, such factors affect the nucleus of the nerve tract and the posterior longitudinal fasciculus.
Sometimes neuropathy of the oculomotor nerve, caused by the above reasons, manifests itself in the form of bilateral drooping eyelids (ptosis). In more rare cases, paresis of the superior rectus muscle of the eye is observed.
It is localized on the reverse side of the main site of damage.
According to statistics, the oculomotor nerve is often damaged due to a microinfarction. It can occur due to vascular pathologies, such as diabetes and hypertension.
Such diseases usually do not immediately lead to disruptions in cerebral circulation and they should be predominantly in an advanced state. Neuritis of this nerve does not affect the reaction of the pupil to light, but in rare cases it is slightly weakened.
A microinfarction occurs near the cavernous sinus or in the area of the interpeduncular fossa. It takes about 3 months for the oculomotor nerve to recover after suffering a disorder.
You should consult a doctor if you notice several symptoms characteristic of paresis of the eye muscles, especially when it comes to children. Among the common manifestations of optic neuropathy, the most basic can be identified:
- Diplopia;
- drooping eyelid;
- Strabismus;
- Decreased pupil reaction to light;
- Inability to turn the eyeball inward;
- Loss of the ability to quickly look at objects located at different distances from each other;
- Protrusion of the eye.
Diagnostics
It is easiest to recognize the lesion, since this pathological process is characterized by drooping eyelids, dilated pupils and abnormal deviations of the eyes.
Based on such signs, making a diagnosis will not be a problem, but often they are combined with each other in various combinations, so the doctor suspects the secondary nature of the disease.
To differentiate paresis of the eye muscles from other possible ailments, the ophthalmologist will need to prescribe an examination, which consists of the following procedures:
- Fundus examination;
- Determination of visual acuity and degree of mobility of the eyeball;
- Light reflex test;
- Angiography (to identify vascular pathologies);
- Magnetic resonance imaging (checks brain tissue for abnormalities).
Sometimes a consultation with a neurologist may be required. If it was not possible to determine the cause of the pathology, then the patient should be registered with a doctor and periodically examined. To prevent the condition from getting worse, your doctor may recommend special sets of exercises and other treatment methods.
Course of therapy
Treatment methods for paresis of the eye muscles in children are not particularly different from those in adults. However, it must be borne in mind that most congenital anomalies are corrected through surgery.
If the operation is successfully performed, the extraocular muscles are partially or completely restored.
If the problem is compression of the nerve pathway, then the main task is to eliminate the cause.
For this purpose, exercises that strengthen the oculomotor muscles are often used. They serve as the basis for the treatment of minor injuries and are a good preventive measure.
In severe cases of the disease, therapeutic exercises well complement the main course of therapy.
Drug therapy for paresis may include the following:
- Vitamin complexes;
- Preparations for strengthening the extraocular muscles and restoring their innervation;
- Eye drops;
- Medicines that improve blood circulation;
- Corrective glasses and bandages.
The pathology can be treated with medications only according to the regimen prescribed by the doctor, so as not to aggravate its course and not to impair vision, especially if the child is sick. It is recommended to combine drug therapy with other methods, namely:
- Steriopictures. By watching them, the extraocular muscles are trained and blood flow improves. The nerve tissues that innervate the muscles of the eye are extremely tense during the procedure, due to this the lost innervation is restored. The procedure must be carried out under the supervision of a specialist so as not to cause complications;
- Electropheresis. This physiotherapeutic procedure is carried out with a 1.5% solution of Neuromidin. The duration of one session of electropheresis usually does not exceed 20 minutes, and it acts directly on the synapses (junctions) of the muscle and nervous tissue of the eyeball. After a course of such therapy, the patient’s severity of paresis decreases and the innervation of the eye muscles improves.
It is impossible to eliminate some causes of paresis in children, for example, congenital anomalies, without surgical intervention. Their duration and degree of risk depend on the type of operation and the factor that influenced the development of the pathology. In the case of severe damage to the optic nerves, it will not be possible to completely eliminate the problem, but there will be a chance to save the child’s vision.
Due to paresis of the extraocular muscles, many complications develop, such as strabismus, ptosis, etc. In children, this pathological process is often a consequence of congenital anomalies. It may not appear immediately, but only over time. This is why it is important to see an ophthalmologist and other doctors, especially in the first years of a child’s life.
Source: https://NashiNervy.ru/perifericheskaya-nervnaya-sistema/prichiny-pareza-glaznyh-myshts-u-detej.html