An aneurysm is a pathological condition in which the walls of arterial vessels are stretched. With a cerebral aneurysm, intracranial vessels are damaged.
The disease occurs in 2 types:
- course of the disease according to the type of tumor;
- course of the disease with rupture of the vessel.
The course of the disease according to the type of tumor is characterized by a symptom of compression. The aneurysm increases in size and damages the cranial nerves (oculomotor, trigeminal, facial). The course of the disease with rupture of the vessel is characterized by hemorrhage into the subarachnoid space or into the substance of the brain.
The diagnosis is made on the basis of complaints, anamnesis, clinical symptoms, computed tomography, MRI, and x-ray data. If there are indications for removal surgery, surgical treatment is performed: clipping and endovascular removal. Since 1999, the 10th revision of the classification of international diseases has been introduced in Russia. Aneurysm of cerebral vessels has a personal code according to ICD-10 I67.1.
Prevalence
The exact prevalence of the disease cannot be determined. Aneurysm often occurs without any specific or nonspecific symptoms. It is possible to detect such damage only after the death of a person at an autopsy; 50% of cases are found in this way.
The prevalence of aneurysm in the world is 10-15 people per 100,000 population.
After rupture of an artery into the subarachnoid space, the immediate mortality of patients is 15%. 25% of patients with ruptures will die within the first 2 days after the incident, and 50% within the next 3 months. An aneurysm can appear in a person or be present from birth. The rupture occurs at the advanced age of 60 years.
Microsurgical treatment of asymptomatic aneurysms
Until recently, asymptomatic aneurysms were detected extremely rarely. In recent years, the widespread availability and availability of noninvasive neuroimaging techniques has led to a significant increase in the number of patients with incidentally discovered aneurysms. Over the past 10 years, the institute has operated on about 400 patients with asymptomatic aneurysms. The results of surgical treatment in this category of patients should be considered satisfactory. Taking into account these data, as well as the extremely high probability of an unfavorable outcome in case of rupture of an aneurysm, it can be argued that unruptured asymptomatic aneurysms in most cases require surgery. It should be noted that the patient must be fully informed about the nature of the disease, the upcoming operation and possible complications.
Causes
The main link in the pathogenesis of the disease is the thinning of the layers of the vascular wall. The wall cannot resist and adapt to blood pressure and begins to stretch. The stretching accelerates due to the filling of the cavity with blood, and a vortex blood flow is formed.
The reasons that trigger the process can be various diseases:
- inflammatory diseases of the membranes of the brain, meningitis lead to the destruction of the layers of the artery wall, it becomes less plastic;
- damage to the skull and brain;
- the presence of a focus of infection, which may not be located in the brain, for example, syphilis, infective endocarditis (the pathogen enters the skull with the general bloodstream);
- high blood pressure leads to thinning of arterial vessels;
- diseases with impaired immune response - systemic lupus erythematosus;
- dyslipidemia, which leads to the formation of atherosclerotic plaques in the body;
- neoplasms that can grow into the head arteries, but may not be located near the brain and damage the vascular wall with their decay products.
Contraindications
Absolute:
- Angiospasm detected during angiography;
- Acute infectious diseases;
- Exacerbations of somatic diseases;
- Bleeding disorders;
- State of shock;
- Collapse;
- Exacerbation of obstructive pulmonary disease or bronchial asthma;
- Decompensation of diabetes mellitus.
Relative:
- Aneurysms of the internal carotid or basilar artery;
- Motor and speech disorders;
- Heart failure;
- Pregnancy.
Clinical manifestations of aneurysm
The main symptoms are associated with the large size of the aneurysm. It begins to compress the brain tissue. Therefore, if the sizes are small, then there will be no signs of the disease. Diagnosis of an aneurysm in this case is random.
With rapid growth of the formation, symptoms appear:
- pressing severe headache;
- dysfunction of the brain, speech, vision, hearing;
- the appearance of spots before the eyes;
- dizziness that occurs at rest or with minor physical exertion;
- loss of memory, attention, concentration;
- vomiting, nausea, dysphagia;
- constant fatigue, fatigue;
- seizures.
The aneurysm may rupture. This is influenced by several reasons: a rapid increase in blood pressure, a stressful situation, injury, fever, nicotine or alcohol abuse.
When a rupture occurs, the person most often loses consciousness and becomes comatose. The severity of the disease depends on the size and location of the formation. If the aneurysm was in the subarachnoid space, then there will be a subarachnoid hematoma. Clinically, this will manifest itself as compression symptoms. If the location of the vascular protrusion was in the substance of the brain, a hemorrhagic stroke will occur. This is a more serious condition.
Symptoms of a ruptured aneurysm:
- severe headache;
- dizziness;
- nausea, vomiting;
- impairment of consciousness, speech, vision, hearing, coordination;
- convulsions.
At the first symptoms of a rupture, it is necessary to take the person to the hospital or call an ambulance. First aid consists of laying the patient down with an elevated head, ensuring a flow of fresh air, unbuttoning and removing all clothing that prevents the person from breathing, and checking the patency of the upper respiratory tract.
Rules for preparing for the event
Preparation differs between elective and emergency patients. For planned patients, the following measures are performed:
- Hospitalization in a hospital;
- Conducting urine and blood tests (read about general and biochemical blood tests separately), coagulograms, examinations for HIV, syphilis, hepatitis B and C, fluorography;
- Consultations with a neurologist, anesthesiologist, neurosurgeon;
- Obtaining consent for surgical intervention and familiarization with possible risks and complications;
- Shaving hair from the area of skin through which the incision will be made;
- Removing nail polish.
The last meal is taken in the evening on the eve of the upcoming intervention.
For patients admitted urgently due to complications, the following minimum preparations are performed:
- Hospitalization;
- Taking blood for tests;
- CT or MRI of the skull (depending on the prevailing clinic, other parts of the body may be examined);
- Correction of vital functions (respiration, blood pressure);
- If necessary, tracheal intubation.
Diagnostics
The disease is often asymptomatic, so detecting a cerebral aneurysm is difficult. The doctor should think about the presence of this formation in the patient if he has severe headaches, dysfunction of brain structures, or seizures.
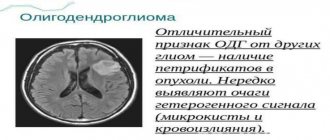
If suspected, the patient is referred to special instrumental research methods: CT, MRI, X-ray, electroencephalography.
The most important and informative methods are computed tomography and magnetic resonance imaging. In the pictures you can see the parameters of a cerebral aneurysm:
- dimensions;
- location;
- thrombus formation;
- hemodynamics inside the formation.
X-ray examination with the introduction of a contrast agent into the vessels of the brain has a high diagnostic value. On an x-ray, you can see the thickness of the vascular wall, the presence of a thrombus in the lumen of the vessel, stretching of the intima and adventitia of the arteries.
X-ray allows for a differential diagnosis in the early stages of the disease and to distinguish a malignant neoplasm from a cerebral aneurysm. X-ray radiation, even in small doses, affects the body with the appearance of negative effects. For pregnant women, pediatric patients, and patients with other diseases, it is preferable to undergo CT and MRI.
Electroencephalography records the biological potentials of the brain and shows the activity of white and gray matter. If brain function abnormalities are detected by EEG results, the patient may be suspected of having a cerebral aneurysm and sent for additional studies, for example, MRI, where the diagnosis of I67.1 will be confirmed. Electroencephalography does not have negative effects on the human body.
Indications for surgery
General indications for clipping:
- Risk of bleeding;
- Age over 75 years;
- The ratio of the width of the neck and the aneurysm is more than 2:1;
- History of an episode of bleeding after intravascular intervention;
- The size of the formation is more than 20 mm;
- Blood clots and calcifications in the protrusion.
Additional indications for clipping of cerebral aneurysms:
- Damage to the middle cerebral artery;
- Hemorrhage into the cerebral ventricle;
- The size of the formation is less than 3 mm;
- Intracerebral hematomas;
- The width of the protrusion neck is more than 4 mm.
Treatment of cerebral aneurysm
Treatment for such a vascular defect involves surgery and removal of the aneurysm. The operation is considered a mandatory procedure if the size of the protrusion reaches 7 mm. During the operation, the defect is removed and the integrity of the brain vessels is restored. There are several methods of surgical operations for this disease: clipping and endovascular removal.
Clipping
Clipping, a microsurgical operation, is the most commonly used method for treating unruptured aneurysms.
The essence of the operation is that the surgeon opens the skull, finds the location of the aneurysm and removes it. The operation carries great risks for the patient's life. The surgical intervention consists of several stages:
- Opening the integrity of the skull. The location of trepanation depends on where the vascular defect is located. Most often, trepanation is performed in the parieto-occipital region.
- Then the membranes of the brain are separated with a scalpel: hard, arachnoid, soft.
- The third step is to find the aneurysm and remove it. This stage is the most critical; the protrusion must not be allowed to rupture. Hemorrhage into the brain matter can lead to the death of the patient. To prevent rupture, a staple or clip is placed at the base of the defect, and the aneurysm is cut off and removed from the skull.
- The final stage is exit from the wound. It is necessary to apply stitches in the correct sequence.
Endovascular removal
Endovascular operations are performed only in high-tech centers. This manipulation requires special specialized equipment, as well as qualified specialists. The MEDSI clinic meets all the requirements for performing endovascular aneurysm removal surgery.
Craniotomy is not performed for this type of operation. The surgeon reaches the aneurysm through the great vessels. The catheter is inserted into the carotid or femoral artery and advanced to the brain. The operation is performed under the control of Doppler ultrasound or CT. The needle with the catheter is brought to the aneurysm, with the help of balloons it is switched off from the general blood flow, and the surgeon removes the aneurysm.
There is another way to separate the aneurysm from the general blood flow. A special chemical is released into the artery, which reaches the protrusion in the brain, forming emboli in the artery.
The highly specialized technology has a number of advantages:
- there is no need to make penetrating wounds of the skull, this contributes to less trauma to the patient;
- the postoperative period is halved;
- The patient does not require general anesthesia;
- if the aneurysm is located near the brain stem or in its depth, it can only be removed using endovascular surgery.
The operation may contain modifications and proprietary techniques.
Every operation carries a risk of complications. With endovascular removal of a cerebral aneurysm, complications are also possible:
- spasm of the arteries, ischemia of areas of the brain;
- rupture of protrusion of an iatrogenic nature;
- blood clot formation in an artery;
- death of a patient for an unknown reason during a removal operation.
Surgical clipping
The goal of the intervention is to apply a special clip to the neck of the aneurysm. This allows you to exclude it from the general bloodstream without blocking a normal vessel. If the aneurysm cannot be clipped, alternative techniques are used (wrapping, tripping, etc.).
Important! The operation to clip the cerebral vessels is performed with craniotomy. Microsurgical techniques are used to carry out the intervention. This allows you to free the aneurysm (its neck) from the feeding vessels. Complications after surgery arise from a previous rupture. Eliminating all its consequences is not so easy. When treating unruptured aneurysms, complications occur less frequently (in 4-10% of cases).
Request a call back Get a free consultation
Postoperative period
After surgery, the patient may experience consequences from removal of a cerebral aneurysm:
- noise in ears;
- loss of vision or loss of visual fields;
- incoordination;
- dizziness and frequent headaches;
- anxiety, malaise, increased irritability;
- fast fatiguability.
The most common problem in the postoperative period is thrombus formation. After applying a clip or suture to a vessel, atherosclerotic plaques may settle, which will close the lumen of the vessel and lead to cerebral ischemia.
Also, in the early period after surgery, the sutures may come apart, which threatens hemorrhage into the medulla or subarachnoid space.
Treatment of patients in the acute period of the disease
| Comparison of brain appearance in the acute and cold periods after SAH |
Treatment of patients in the acute period after SAH is a complex task that requires the involvement of various specialists. The rationale for operations in the acute period is, first of all, the possibility of repeated hemorrhages, which are accompanied by extremely high mortality. After switching off the aneurysm, it is also possible to begin intensive vascular therapy aimed at eliminating the consequences of hemorrhage. Based on an analysis of the results of surgical treatment of more than 600 patients in the acute period of SAH at the institute, it was shown that prognostically significant criteria for assessing the outcome of the operation are the massiveness of the hemorrhage, the patient’s condition on the Hunt-Hess or WFNS scale, and the duration of surgery after SAH. Taking these factors into account, the basic principles of treating patients have been developed. Indications for surgery in the acute stage of SAH must be strictly individualized. To resolve the issue of patient management tactics, the necessary minimum is to assess the patient’s condition using the Hunt-Hess or WFNS scale, CT, angiography, TC ultrasound and determining the severity of vasospasm. Particular attention should be paid to the period after hemorrhage. The operation is indicated for patients in stages I–II according to Hunt–Hess, regardless of the period after SAH; in stages III–IV according to Hunt–Hess within a period of 14 days after SAH. In stage III–IV patients undergoing surgery on days 0–3 after SAH, it is necessary to install sensors for postoperative ICP monitoring, since these patients are characterized by the development of vasospasm and cerebral edema in the early postoperative period. In stage III–IV patients on days 4–7 after SAH, in the presence of moderate or severe vasospasm, surgery should be abstained. The duration of delay of surgery for vasospasm depends on the TC parameters of the ultrasound scan: the operation can be performed when the blood flow velocity decreases to the level corresponding to a mild spasm, or when it stabilizes at the level of a moderate spasm for several days, but not earlier than 7 days after SAH. In stage V, surgery is indicated only in the presence of large intracerebral hematomas. In these cases, surgery is most effective with the earliest interventions possible. In the acute period of SAH, endovascular exclusion of the aneurysm should be considered the method of choice, especially in severely ill patients. In some cases, if it is impossible to completely occlude the aneurysm, you can limit yourself to partial shutdown, followed by a repeat operation after the condition improves. In addition to anatomical features, a limitation for endovascular surgery in the acute period is severe vasospasm, which prevents the insertion of a catheter. When performing direct intervention, it is necessary to take into account that the brain of a patient in the acute period of SAH is much more sensitive to surgical trauma; therefore, it is necessary to use the most gentle methods of access to the aneurysm with limited traction of the brain, the use of relaxation methods (osmodiuresis, removal of cerebrospinal fluid) and brain protection from ischemia. Throughout the entire period of treatment of patients in the acute stage of SAH, the leading task is the prevention and treatment of complications typical for hemorrhage from an aneurysm, primarily vasospasm, cerebral edema and acute or delayed hydrocephalus. Currently, to combat these complications, the technique of intravascular administration of antispasmodics under the control of TC ultrasound, 3H-therapy under multimodal monitoring, and decompressive craniotomy are used. Over the past 10 years, postoperative mortality during direct operations in the acute period averaged 7.3%, and overall mortality - 12.4%. Among surviving patients, 80% are completely independent in daily life, and about 40% have returned to work and school. The data obtained were used to create a recommendation protocol for the management of patients in the acute period of SAH together with leading neurosurgeons in Russia. The experience of the institute allowed us to take part in several international studies on the treatment of patients in the acute stage of SAH.
Rehabilitation process of patients
A patient who has suffered a rupture of a cerebral vascular protrusion requires rehabilitation. Methods used in the rehabilitation course:
- if the patient has muscle paralysis and is in a supine position, splints are used;
- carrying out massage procedures;
- rehabilitation using applications containing clay and ozokerite.
If there are indications for the use of physiotherapeutic procedures, they are included in the general rehabilitation course.
Treatment of pathology
Emergency treatment for patients with a ruptured brain aneurysm includes restoring deteriorating breathing and reducing intracranial pressure.
There are 2 main treatment options.
They allow you to fasten the intracranial protrusion of cerebral vessels.
- Surgical clipping.
- Endovascular embolization.
If possible, treatment is given within the first 24 hours after bleeding to close the ruptured aneurysm and reduce the risk of recurrences that affect the blood vessels.
Let's consider the features of both methods.