A brain abscess (BAA) is a focal lesion of the higher part of the central nervous system with an accumulation of pus in the medulla, limited to the capsule. The purulent component is formed as a result of bacteria, fungal infections, and protozoan microorganisms entering the brain structures.
Common causative agents of an abscess are forms of pathogenic agents such as staphylococci, streptococci, meningococci, Proteus, Escherichia coli, etc. Often two or more bacteria are diagnosed simultaneously, as well as a combination of anaerobic and aerobic infections. In this case, the abscess can be single or multiple. Penetration of the pyogenic source into the brain tissue occurs through contact, traumatic, and hematogenous routes.
Diagnosis on photographs.
Purulent brain damage is a fairly rare phenomenon, but dangerous. For every 100 thousand people hospitalized in a neurological hospital, there is 1 case with this pathology. The danger of a progressive abscess is the development of severe complications: depression of central nervous system functions, seizures, hydrocephalus (dropsy of the brain), inflammation of the bone marrow, etc. Very high risks of disability and mortality are determined.
Epidemiological situation
Despite the widespread introduction of powerful bactericidal drugs and the successes of microbiological and thermal imaging diagnostics, the medical and statistical indicator of the incidence rate remains relatively constant.
- Pathology can develop at any stage of life, but according to statistics, the average age of patients is from 35 to 45 years.
- The prevalence of cases of brain abscess among male and female populations is in the ratio of 2:1. That is, men are 2 times more likely to get the disease than women.
- Of 100% of patients, about 25% are children and adolescents under 15 years of age. The incidence in children under two years of age is extremely rare in practice, mainly due to meningitis with gram-positive flora.
- Due to previous otitis media, the disease reaches its peak in children and adults over 40 years of age.
- The consequences of various forms of sinusitis in the form of AGM are mainly observed in people 10-30 years old.
- Brain abscesses are the predominant type of intracranial infectious processes in HIV-infected patients. With HIV, the most common causative agent is toxoplasma (up to 30% of cases).
Unfortunately, the possibility of death cannot be excluded: death due to AGM occurs in 10% of patients. Pathology can also threaten disability, which occurs in 50% of patients, even after treatment. In 1/3 of the surviving patients, the consequence of AGM is epileptic syndrome.
Consequences of a brain abscess
The prognosis of this disease depends on several factors:
- The state of the body's immune system.
- Timeliness and adequacy of treatment.
- Number of purulent foci.
Statistics say that the mortality rate for this pathology is 10%, but disability reaches high numbers (on average 55%).
There are a number of complications that a brain abscess can lead to:
- Melting of the skull bones as a result of their inflammation.
- Epileptic syndrome (almost 1/3 of patients).
- Breakthrough of abscess contents into the ventricles of the brain.
- Hydrocephalus (fluid accumulation inside the skull).
What causes pus to form in the brain?
Favorable ground for the introduction of infection into the brain is created by a decrease in immunity in combination with the presence of a pathogenic source in the body. Against the background of a depressed immune system, it is possible to get a complication in the form of an intracranial abscess even from a sore throat, sinusitis or otitis media. We emphasize that acute inflammation of the middle or inner ear and paranasal sinuses in 45% of cases are the culprits of cerebral abscesses. In addition, often sources of infection are:
- chronic lung infections - bronchiectasis, pyothorax, abscess pneumonia;
- bone osteomyelitis;
- cholecystitis;
- infectious pathologies of the gastrointestinal tract;
- pelvic organ infections.
Somewhat less frequently, the causative factors are complications of the following pathologies:
- bacterial endocarditis;
- hereditary hemorrhagic angiomatosis;
- CHD – congenital heart defects;
- bacterial meningitis (traditionally complicated by an abscess in children, generally not in adults).
Also, brain abscesses can form due to the development of a purulent complication after a planned neurosurgical operation or severe head injury. As a rule, they are caused by Staphylococcus aureus. Postoperative consequences account for approximately 0.5%-1.5% of the total structure of brain abscesses. With penetrating traumatic brain injuries, that is, with open wounds of the skull with disruption of the integrity of the dura mater, the risk of infection with the development of purulent-septic pathogenesis is extremely high.
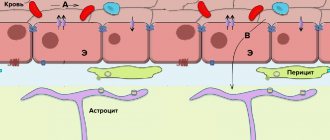
Infection of the brain with pyogenic bacilli can occur through one of the following mechanisms:
- by contact - direct transfer of infected material through the area adjacent to osteitis/osteomyelitis, or retrograde through emissary veins (for example, with ENT infections, osteomyelitis of the jaw, etc.);
- hematogenous (metastatic) route - dissemination of the pathogen occurs through the bloodstream from a distant (primary) zone of infection (as an option, with endocarditis, pulmonary lesions, urogenital, intestinal infections, etc.);
- in a traumatic way - infection of nervous tissue through direct interaction of the wound surface with the external environment (this is local post-traumatic and post-surgical infection).
It is especially worth emphasizing that weakened people with complex diagnoses: diabetes, cancer, drug addiction, AIDS are significantly susceptible to this disease.
How is a brain abscess treated in Israel?
The treatment strategy for brain abscess in each case is planned individually, depending on the causes of the disease, the location of the pathological process, and the severity of symptoms. Painful signs can be very different.
Many patients exhibit the so-called triad of symptoms:
- General cerebral signs: headaches, dizziness, decreased vision and photophobia, epileptic seizures, bradycardia, slow thinking, confusion.
- General infectious manifestations: increased body temperature, fever and chills, increased sweating, general weakness, loss of appetite, nausea and vomiting, weight loss.
- Focal symptoms: appear in cases where the abscess puts pressure on functionally significant areas of the brain. For example, if the pathological process is localized near the cerebellum, the patient may experience unsteadiness in gait, poor coordination of movements, decreased muscle tone, and repeated involuntary eye movements.
Since all these symptoms rapidly intensify as the size of the purulent focus increases, a brain abscess requires immediate treatment.
Doctors at the Top Assuta clinic use the following methods for this:
- Stereotactic aspiration . A special syringe with a hollow needle is inserted into the pathological focus, with which doctors suck out the purulent contents, and then wash the cavity with an antiseptic solution and/or antibacterial drugs. The procedure is performed using a minimally invasive method under CT guidance, so the risks of damage to adjacent healthy brain tissue are minimized. However, in most cases, it is not possible to completely remove all the pus the first time, and after some time aspiration has to be repeated.
- Abscess drainage . A more effective method of treating intracerebral abscesses involves installing a special drainage system into the purulent cavity. With its help, not only is all the pus pumped out, but the pathological focus is also washed with saline and antibiotics. Depending on the severity of the pathology, such treatment can last for several days. The drainage procedure is also carried out without major damage to the cranial tissue, so recovery after it is quite quick.
- Craniotomy (craniotomy) . In some cases, brain abscesses are removed using an open method. To do this, a small fragment of the skull bones is cut out, after which doctors carefully separate the capsule with purulent contents and remove it. In Israeli clinics, craniotomy is performed using modern minimally invasive methods under the control of high-precision neuronavigation equipment, so such operations are completely safe for patients.
- Drug therapy . Since the development of purulent processes is always caused by bacterial infections, to successfully eliminate the pathology, doctors must prescribe antibiotic therapy to patients. Specific types of drugs are selected individually in each case, based on the type of pathogen identified. At the initial stages of disease progression, as well as in cases of hard-to-reach localization of the pathological focus, antibiotic therapy can be used as an independent treatment; in other cases, it is carried out in combination with removal of the abscess to prevent the development of complications and prevent relapses. Additionally, symptomatic medications may be prescribed: corticosteroids, anticonvulsants, nootropics and others. Provided timely treatment with antibiotics and evacuation of purulent contents from the brain, the prognosis for patients is quite favorable - in almost 90% of cases, Israeli specialists manage to save a person’s life and maintain its good quality.
Pathogenesis: how does the process develop?
The development of the disease consists of 4 separate stages, or stages:
- The first stage is early infiltration. During the first 3 days after entry of the pathogenic agent, a poorly demarcated diffuse focus of inflammation is formed with destruction of brain tissue and swelling around it.
- The second stage is late cerebritis. The center of focal inflammation undergoes suppuration and necrotization on days 4-9, which is accompanied by the formation of a cavity. The cavity is filled with semi-liquid purulent exudate. Fibroblasts accumulate along the outer part.
- The third stage is the formation of the gliosis capsule. From 10-13 days the protective capsule of the abscess begins to form. Thus, there is an intensification of the growth of the layer of fibroblasts bordered by a rim of neovascularization. Along with this, reactive astrorcytosis is noted.
- The last stage (4th stage) is the final formation of the capsule. The capsular component around the filled purulent cavity is fully compacted (reactive collagen takes part in this). The necrotic focus takes on clear outlines.
Further processes at the last stage depend on the virulence of the pathogenic flora, the route of spread, the immune status of the patient, and the level of hypoxia of the affected brain structures. The correctness of diagnostic and therapeutic measures will no less affect the degree of progression of AGM. As a rule, the disease cannot regress on its own. Without adequate therapy, in the vast majority of cases, the internal volume of the abscess increases, and the appearance of new infected areas along the periphery of the capsule cannot be ruled out.
How does a brain abscess develop?
There are several options for the development of a brain abscess:
- hematogenous (inflammatory processes in the lungs, gastrointestinal infections and sepsis);
- through infection as a result of traumatic brain injury;
- purulent-inflammatory (caused by inflammation in the nose and ears);
- infected (complications after neurosurgical interventions).
After infection penetrates, an abscess forms within three weeks and has the following stages:
- The first three days: the development of encephalitis (local tissue inflammation), which can be eliminated with antibacterial therapy.
- Days 4-9: inflammation progresses, the cavity filled with pus increases.
- 10-13 days: the formation of a protective capsule around the purulent focus, this prevents the process from spreading.
- Third week: compaction of the capsule with pus. Depending on the treatment taken at this stage, the brain abscess may begin to develop in the opposite direction or increase in size, and new foci of inflammation may also begin to appear.
Symptoms of a brain abscess
The difficulty of independently detecting a brain abscess is that it does not have unique symptoms, but only those that can be attributed to any other inflammatory diseases or brain diseases:
- general malaise;
- weakness;
- chills;
- vomit;
- apathy;
- headache;
- eye irritation from light;
- increased intracranial pressure;
- mental disorders, nervousness.
Therefore, if the above symptoms appear, you should consult a doctor as soon as possible. When a specialist diagnoses an abscess, the main reason for a more accurate examination will be the presence of an inflammatory process, which is accompanied by the appearance of neuropsychiatric disorders. To diagnose a brain abscess, the following are used:
- CT scan;
- MRI of the brain;
- MS spectroscopy;
- Ophthalmoscopy (detection of signs of intracranial pressure);
- Blood test (detecting signs of inflammation).
As a result of the diagnosis, the stage of the brain abscess will be determined and treatment will be selected.
Clinical picture: what symptoms should alert you?
Clinical signs of a brain abscess can be expressed in different ways - from a terrible headache to a whole complex of symptoms of cerebral disorders. The concentration field of pain in the head is directly related to the location of the abscess. But, note, local signs may not be so pronounced, or even be absent altogether. This combination of situations prevents timely diagnosis and the rapid adoption of specialized treatment measures, the speed of which determines the prognosis of the outcome. Symptoms that should prompt you to immediately consult a doctor:
- intense headaches, they are predominantly of a bursting, pressing, pulsating nature in a certain place (often worsening in the morning);
- febrile phenomena with intoxication - chills, body hyperthermia, nausea, vomiting, dizziness, loss of strength;
- hyperesthesia of various types - unpleasant sensations when touching the skin, crawling and tingling, intolerance to bright light and noise;
- visual acuity disorder, eye proptosis, eyelid swelling, facial swelling;
- hearing impairment in the form of a sensation of sounds in the ears, a decrease or exacerbation of sound perception;
- Kerning's symptom - the inability to extend the lower limb from a bent position at an angle of 90 degrees in the hip joint and knee joint;
- Brudzinski's symptom - when one leg is passively flexed, the opposite leg reflexively bends or when the head is passively brought forward, the limbs involuntarily bend;
- sharp pain phenomena along the trigeminal and occipital nerves, when pressing on the outer wall of the ear canal or on the area of the zygomatic bone;
- stiffness of the neck muscles, making it difficult to lower the head to the chest and throw it back;
- unexplained muscle pain in the limbs, cramps, epileptic seizures;
- disturbance of cardiac and respiratory rhythm (bradycardia, Cushing's reflex), increased systolic (upper) pressure;
- increasing depression of consciousness with possible fainting, problems with coordination, inhibition of brain activity.
Everyone should understand that such symptoms are not normal for the body, especially if they tend to recur. Therefore, rather than being dissatisfied and getting disabling complications or exposing yourself to mortal risk, it is better to worry once again and undergo a differential diagnosis. If the disease is confirmed, qualified medical care is urgently required.
Brain abscess
Brain abscess is a limited purulent melting of the brain substance, i.e. focal accumulation of pus in the substance of the brain.
Etiology, pathogenesis
The reason is the entry of streptococci, staphylococci, pneumococci, less often other microbes into the medulla from purulent foci located in the middle or inner ear (otogenic abscesses), paranasal sinuses (rhinogenic abscesses), from an osteomyelitic focus in the bones of the skull, phlegmon of the soft tissues of the head. That is, a source of infection is needed. The main source of infection is otitis media, often chronic (about 70% of all brain abscesses). In newborns, there may be infections of the upper respiratory tract of the mother, caused by neonatal sepsis, umbilical infection, pneumonia.
The infection spreads from the middle and inner ear in two ways: by contact through the dura and pia mater or through the lymphatic and bloodstream. In 16-24% of cases, the abscess occurs as a result of bacterial microembolism in the blood vessels (metastatic abscesses). The main source of metastasis is the lungs (abscess pneumonia, empyema, bronchiectasis, lung abscess), and less commonly, ulcerative bacterial endocarditis. Bacterial emboli can also enter through the capillary network of the lungs with pyoderma, phlegmon, osteomyelitis of tubular bones, and actinomycosis. Traumatic brain injury plays a certain role, especially when accompanied by fractures or cracks in the bones of the base of the skull, opening the entry gate for infection. Brain abscess is a common complication of a penetrating or blind gunshot wound.
Boys get sick 2 times more often than girls.
Symptoms, course:
The initial period is the body’s reaction to the introduction of infection into the brain tissue - general malaise, lethargy, loss of appetite, increased temperature (from subfibril numbers - 37.2 - 37.4 and above), intense headache, vomiting, high fever, meningeal signs (pain in the cervical - occipital spine, inability to reach the chest with the chin).
Changes in the blood test - polynuclear leukocytosis, increased ESR, moderate pleocytosis in the cerebrospinal fluid.
Latent period - with high virulence of the pathogen, the brain tissue melts and an abscess capsule is gradually formed around the resulting cavity filled with pus, limiting the purulent process (after 4-6 weeks) - the patient’s condition improves, the child becomes more active, complaints disappear.
The manifest stage is a clinically obvious stage; a number of factors contribute to entering it - minor trauma, for example to the head, various acute diseases, for example acute respiratory infections, acute respiratory viral infections, etc.
Clinically, several groups of symptoms can be distinguished:
- Inflammatory – as described above.
- Symptoms of increased intracranial pressure - in children, especially 5-7 years old - a rapid increase in the size of the skull, due to which there are no headaches for a long time. An X-ray of the skull shows divergence of the sutures (coronal, sagittal, more pronounced digital impressions...) - resulting in severe headaches and vomiting, frequent and repeated.
- Focal symptoms depend on the location of the abscess. For example, it is located in the cerebral hemispheres - movement disorders and seizures occur. (sometimes seizures can be one of the first manifestations of this disease, especially in young children.
The extreme stage is the terminal period - mortality is about 1/3 of patients. Especially with multiple brain abscesses, when there is spread to the cerebrospinal fluid system and the membranes of the brain. (children 3 – 4 years old).
For diagnosis they use: computer, magnetic resonance imaging, cerebral angiography.
Differentiated diagnostics.
Brain abscess with focal meningoencephalitis or meningitis, with echoencephalography data (displacement of the midline brain structures in supratentorial abscess) and computed tomography playing a decisive role. The latter makes it possible to distinguish an abscess from a brain tumor.
Treatment.
Surgery. There are various ways:
The Spasokukotsky-Bakulev method consists of repeated punctures (from 2 to 13) with suction of pus and the introduction of antibiotics and disinfectants into the abscess cavity. (there are practically no contraindications, there is no need to remove the scar-wrinkled capsule during recovery, in small children puncture can be done through an open fontanel or a broken suture) - it is not effective only for multi-chamber and multiple abscesses.
N. N. Burdenko - removal of the abscess along with a well-formed capsule. (used in middle-aged and older children).
The oldest method is wide opening and subsequent drainage of the abscess. – when an elastic catheter is used, through which antibacterial agents are periodically washed and introduced into the cavity.
Massive doses of antibiotics must be prescribed before and after surgery.
Forecast. Serious. With single abscesses after surgery, recovery occurs in 70-80% of cases.
Diagnostic procedures for identifying AGM
Suspecting a disease, the patient is subjected to thorough examinations to refute or establish the fact of its presence on reasoned grounds. It is necessary to take into account that in the late period the clinical picture is similar to that of brain tumors. The principle of differentiation plays a huge role in diagnosis. It is based on anamnesis data about the patient’s infectious and inflammatory diseases and the use of imaging methods.
Computed tomography with contrast is a fundamental method that allows one to distinguish purulent pathogenesis in brain tissue from intracranial neoplasms, to establish the exact location, size, type and multiplicity of the lesion, and perifocal signs. The following are used as auxiliary diagnostic techniques to clarify the diagnosis:
- magnetic resonance imaging;
- echoencephalography;
- cerebral angiography;
- abscessography.
The patient is given directions for general laboratory tests, which are a mandatory part of any diagnostic program. But, as experts point out, laboratory tests, unlike neuroimaging methods, do not play a key role in making a diagnosis. For example, ESR, high C-reactive protein values, and elevated white blood cell counts characterize many body conditions associated with inflammation and infections. That is, these are not specific, but general infection indicators. Moreover, cultures for bacteremia in a dominant amount (almost 90% of patients) ultimately turn out to be sterile.
Diagnosis of brain abscess in Israel
To confirm the diagnosis and determine the most optimal methods of therapy, doctors first prescribe a comprehensive examination to each patient. At Top Assuta it can be completed in just 3-4 days - the clinic has ultra-modern diagnostic equipment, so the research results are always 100% error-free.
If a patient cannot come to Israel for one reason or another, he can consult with one of the leading specialists at the hospital via Skype. The doctor will analyze all the documents provided and draw up his opinion on them, after which, during the video consultation, he will answer all your questions and recommend effective treatment methods.
- Day 1
- Day 2
- Day 3
Inspection and consultation
Immediately after arriving in the country, the patient, accompanied by a case manager, goes to see the attending physician. The doctor clarifies the symptoms, systematizes the medical history, and then writes out directions for laboratory and instrumental studies.
Diagnostic procedures
Israeli specialists use the following methods for diagnosing brain abscess:
- CT scan.
- Magnetic resonance imaging.
- Echoencephaloscopy.
- Extensive blood tests.
- Craniography.
- Lumbar puncture and others.
Medical consultation
Having established the final diagnosis, the attending physician, together with colleagues (neurologists, neurosurgeons and other specialized specialists), develops an individual therapy program for the patient.
Treatment methods for brain abscess
This pathology is a neurosurgical problem and is almost always treated surgically. Surgery must be combined with antibiotic therapy. Neurosurgeons, depending on the severity of the medical problem, indications and contraindications, use 3 methods of surgical removal of a brain abscess.
- Simple inflow and outflow drainage of a purulent cavity. Surgical intervention involves removing pus through a catheter device installed in the capsule. The procedure is performed under local anesthesia. After pumping out the pathological fluid and washing the cavity with saline, bactericidal drugs are administered. Treatment can last several days, so the drainage elements are not removed until therapy is completed.
- Stereotactic biopsy of intracerebral abscesses. Surgical intervention is carried out by analogy with the minimally invasive drainage procedure. But in this case, the puncture method is used. The lesion cavity is punctured, washed with an antiseptic solution and/or an antibiotic in liquid form of a certain concentration. The procedure is suitable for people with deep-seated pathogenesis or critically ill patients in need of emergency medical care. Needle aspiration may also be part of the preparation for open surgery.
- Classical open surgery to remove purulent formation. This is a radical operation under the control of an intraoperative microscope, including “cutting out” a bone flap in the projection of the area of suppuration and dissection of the dura mater. The session takes place under general anesthesia. Through the created access, the purulent cavity is partially emptied of the pathological substance. Next, a gentle encephalotomy is performed, followed by isolation and resection of the capsule. After capsulotomy and hemostasis, the surgical field is washed with an antiseptic and drained. The dura mater is sutured, the cranial defect is covered with a bone flap, and the latter is fixed. The dissected skin is compared and sutured layer by layer.
Open surgery.
Conservative injection, oral antibiotic therapy in an enhanced and prolonged mode is appropriate especially at the beginning of the development of the infectious process, when no more than 14 days have passed. In this case, the size of the lesion should not exceed 2 cm in diameter, maximum 3 cm, and the problem area should not have signs of capsule formation.
In practice, however, specialists more often deal with an already advanced disease that has a delimiting capsule. A non-surgical approach is not practical here; the problem is dealt with exclusively using the surgical interventions mentioned above.
Brain abscess (Cerebral abscess)
At the encephalitic stage of the abscess (history of up to 2 weeks), as well as in the case of a small brain abscess (up to 3 cm in diameter), conservative treatment is recommended, the basis of which should be empirical antibacterial therapy. In some cases, it is possible to perform a stereotactic biopsy for the purpose of final verification of the diagnosis and isolation of the pathogen.
Abscesses that cause brain dislocation and increased intracranial pressure, as well as those localized in the area of the ventricular system (pus entering the ventricular system often leads to death) are absolute indications for surgical intervention. Traumatic brain abscesses located in the foreign body area are also subject to surgical treatment, since this inflammatory process cannot be treated conservatively. Despite the poor prognosis, fungal abscesses are also an absolute indication for surgery.
Contraindications to surgical treatment are brain abscesses located in vital and deep structures (the optic thalamus, brain stem, subcortical nuclei). In such cases, it is possible to carry out a stereotactic method of treatment: puncture of the brain abscess and its emptying, followed by washing the cavity and administering antibacterial drugs. Both single and multiple (through a catheter installed for several days) rinsing of the cavity is possible.
Severe somatic diseases are not an absolute contraindication to surgical treatment, since stereotactic surgery can also be performed under local anesthesia. An absolute contraindication to surgery can only be an extremely serious condition of the patient (terminal coma), since in such cases any surgical intervention is contraindicated.
Drug treatment
The goal of empirical (in the absence of culture or when it is impossible to isolate the pathogen) antibacterial therapy is to cover the maximum possible range of pathogens. Recommended treatment programs:
- For brain abscess without a history of TBI or neurosurgical intervention, the following treatment algorithm is indicated: vancomycin; III generation cephalosporins (cefotaxime, ceftriaxone, cefixime); Metronidazole. In the case of post-traumatic brain abscess, metronidazole is replaced with rifampicin.
- The causative agent of brain abscess in patients with immunodeficiency conditions (except HIV) is most often Cryptococcus neoformans, less often Candida spp or Aspergillius spp. Therefore, in these cases, amphoreticin B or liposomal amphoreticin B is prescribed. After the abscess disappears (according to neurovisualization studies), fluconazole is used for 10 weeks, subsequently the dose is halved and left as a maintenance dose.
- In patients with HIV, the causative agent of brain abscess is most often Toxoplasma gondii, so empirical treatment of patients should include sulfadiazine with pyrimethamine.
After isolation of the pathogen from culture, treatment must be changed, taking into account the antibiogram. If cultures are sterile, empirical antibiotic therapy should be continued. The duration of intensive antibiotic therapy is at least 6 weeks, after which it is recommended to change the antibiotics to oral ones and continue treatment for another 6 weeks.
The prescription of glucocorticoids is justified only in the case of adequate antibacterial therapy, since only with a positive prognosis can glucocorticoids cause a decrease in the severity and reverse development of the brain abscess capsule. In other cases, their use may cause the inflammatory process to spread beyond the primary focus.
Surgery
The main methods of surgical treatment of intracerebral abscesses are simple or inflow-outflow drainage. Their essence is to install a catheter into the abscess cavity, through which the pus is evacuated, followed by the administration of antibacterial drugs. It is possible to install a second catheter of a smaller diameter (for several days), through which a rinsing solution is infused (most often, 0.9% sodium chloride solution). Drainage of the abscess must be accompanied by antibacterial therapy (first empirical, then taking into account the sensitivity of the isolated pathogen to antibiotics).
Stereotactic aspiration of abscess contents without installing a drain is an alternative method of surgical treatment of brain abscess. Its main advantages are lenient requirements for the qualifications of medical staff (close attention and special knowledge are required to control the functioning of the inflow and outflow system) and a lower risk of secondary infection. However, in 70% of the use of this method, repeated aspirations are necessary.
In the case of multiple brain abscesses, it is necessary first of all to drain the focus that is most dangerous in terms of complications (breakthrough of pus into the ventricular system, brain dislocation), and also the most significant in the clinical picture. In the case of empyema or subdural abscess of the brain, drainage is used without using the inflow and outflow system.
Where is the best place to get treatment?
It is preferable to have surgery abroad, in clinics that are impeccably equipped with advanced personnel (neurosurgeons, anesthesiologists, rehabilitation specialists, etc.), and high-tech equipment for diagnostics and surgery. This will allow you to count on minimizing the likelihood of developing intra- and postoperative consequences: osteomyelitis of the cranial bones, epilepsy, hydrocephalus, cerebral hematoma, paralysis of the body, etc.
Central Military Hospital of Prague.
An excellent neurosurgical base, as confirmed by world experts and patient reviews, is located in the Czech Republic. Czech medical institutions are recognized as advanced in providing surgical care to patients with various lesions of the nervous system, including operations for brain abscesses of any location and severity.
In the Czech Republic, all surgical services are well-thought-out innovative tactics that require safe access, comfortable and painless manipulation, rapid rehabilitation and restoration of quality of life to the level of a healthy person. The cost of procedures on the brain here is 2 times less than in Germany or Israel, and this is with no less high-quality execution of the treatment process.
Diagnostics
A thorough diagnosis of a brain abscess with the study of anamnesis allows us to identify the focus of the infectious inflammatory process and the corresponding neurological manifestations. The examination method is computed tomography of the brain. Already on the first day, the study makes it possible to identify areas with changes in the shape and density of tissues. The contrast agent accumulates unevenly and is located closer to the periphery of the inflammatory focus.
An already formed abscess has clear contours and rounded outlines. To clarify information on the disease, magnetic resonance imaging is performed. The disease can be diagnosed using this method in the first day from the onset of development. Pathology is differentiated from primary and metastatic tumors. Laboratory diagnostics are uninformative.
To prescribe effective antibacterial therapy, the sensitivity of the identified pathogen to antibiotics must be taken into account. It is extremely important to start treatment as soon as possible. The disease is fatal in 10% of cases. In half of the patients, the formation of epileptic syndrome occurs.
Treatment
Treatment of brain abscess is carried out in several areas:
- Indications for abscess drainage: abscess size greater than 2.5 cm or presence of volumetric impact
- Additional antibiotic therapy according to the antibiogram
- Antibiotic therapy is the only treatment method in the presence of concomitant meningitis, ependymatitis, hydrocephalus and risk factors that are a contraindication to surgery
- Treatment continues for 6-8 weeks.