Stroke: types, signs, prevention
28.06.2019
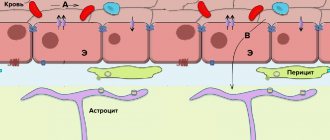
Stroke is an acute disorder of cerebral circulation due to blockage of blood vessels or their rupture. After a vascular accident, neurological symptoms develop within a few minutes or hours, which progress, sometimes leading to death. Recently, cases of stroke have become more frequent at young ages, up to 30 years.
Kinds
The main classification of strokes (according to ICD-10) takes into account the cause and mechanism of stroke.
- An ischemic stroke is characterized by a cessation of blood flow to the brain tissue. The reason is a violation of blood flow, blockage of an artery with a blood clot and/or narrowing by an atherosclerotic plaque (atherothrombotic), vasospasm, and a decrease in pressure. Most often develops at the age of 50-69 years. The incidence is 64-75% among all types of stroke.
- Hemorrhagic stroke is a hemorrhage into the substance of the brain or under the arachnoid membrane due to rupture of a vessel as a result of high blood pressure, atherosclerosis, vasculitis, aneurysms, coagulation disorders. Patients aged 50-69 years are at high risk. At 39-49 years old it is less common. The incidence is 15-20% among all types of stroke.
There are classifications that distinguish types of stroke taking into account other signs.
1. By severity:
- minor, including microstroke (transient ischemic attack) - a passing disturbance of cerebral circulation with complete disappearance of neurological symptoms within 1 day to 3 weeks;
- moderate severity;
- severe, extensive stroke of the brain - damage to a large area with pronounced neurological symptoms and severe condition, sometimes with falling into a deep coma.
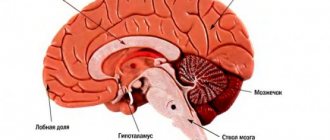
2. By location
- left or right hemisphere. Each side is responsible for different functions, so the symptoms will be different. For example, if the left half is affected, the movements of the right side of the body suffer, speech and memory are impaired. The person loses the ability to read and write.
When the right hemisphere is damaged, the movement of the left side of the body, the perception of oneself, one’s body, and the surrounding space are impaired, and mental disorders develop.
3. By quantity
- primary stroke (first) and repeated strokes (second, third, fourth). Repeated strokes are more severe because the lesion area increases each time.
4. By age
- in children, starting from the prenatal period, young, elderly. The severity of clinical manifestations and prognosis depend on the patient’s age, the cause of concomitant pathology, and the timeliness of diagnosis. The most difficult prognosis is for delayed detection of a stroke, a large lesion, a weakened body due to concomitant diseases, bad habits, and vitamin deficiency.
5. By localization
:
- in the vertebrobasilar basin with damage to the occipital lobe of the brain, cerebellum and brainstem - visual disturbances develop, gait changes;
- frontal lobes - speech and swallowing suffer;
- temporal lobes - memory, writing, speech deteriorate;
- parietal lobe - speech and speech understanding suffer.
First aid
Measures to reduce the temperature depend on the cause that caused it and are determined by the doctor. For this purpose, it is necessary to undergo a diagnostic examination.
It is not allowed to engage in treatment without the supervision of a doctor. Before contacting a medical facility, you can use antipyretic drugs. Under no circumstances should antibiotics or hormonal drugs be taken orally.
Before giving the patient medicine, you need to make sure that his swallowing function is not impaired.
If the temperature does not return to normal after taking medications, it is reduced in a hospital setting. To do this, the patient is injected with lytic mixtures by drip. If immediate hospitalization is not possible, you should avoid overheating and wipe the neck, elbows, and popliteal fossae with cool water.
Carefully! Some anti-inflammatory drugs help thin the blood. Taking them may cause bleeding.
Development and risk groups
The development of a stroke is caused by a sharp increase in blood pressure, physical activity, and emotional stress. In such situations, a vessel ruptures followed by hemorrhage or spasm with ischemia. Predisposing factors are diabetes mellitus, high cholesterol, heart, vascular and blood diseases, and excess weight. In these diseases, blood vessels lose their elasticity and their walls stretch. People who or their close relatives have had a stroke or heart attack should be especially careful.
There are scales that determine the degree of risk of developing a stroke: the Framingham scale for assessing individual risk of developing stroke, the London School of Hygiene questionnaire on cardiovascular diseases by J. Rose.
By undergoing such testing, you can identify the degree of risk, undergo an examination and undergo a course of treatment in a timely manner before your health is affected.
Risk groups are identified:
- by age and gender - the likelihood of a stroke increases after 30 years. Ischemic stroke occurs more often in men aged 50-69 years. The incidence of hemorrhagic stroke up to 60 years of age is the same in men and women, then higher in women;
- in terms of lifestyle - unfavorable factors include inactivity, bad habits, stress, heavy physical labor. These factors worsen health and provoke chronic heart and vascular diseases.
First signs and symptoms
Before a stroke, drowsiness, headache, numbness of the limbs, fatigue, spots before the eyes, nausea, dizziness, temperature fluctuations, and blood pressure jumps appear. These are the harbingers or first signs of a stroke that appear several hours or days before the disaster. Most often, these symptoms are ignored, or they are attributed to fatigue and overwork.
Symptoms of a stroke themselves are divided into general cerebral and focal. They can be of varying degrees of severity depending on the prevalence of the pathological process.
- General cerebral symptoms: headache, impaired consciousness up to loss of consciousness, stupor, agitation or weakness, disorientation in space and time, sweating, feeling hot, convulsions. Makes you feel sleepy and sometimes chills.
- The focal abnormalities of a stroke depend on which area of the brain is affected. They can be unilateral or bilateral. This group includes disturbances in speech, vision (visual hallucinations), gait, movements up to paralysis, and sensitivity.
Symptoms of ischemic cerebral stroke develop gradually, with focal symptoms predominant.
With a hemorrhagic stroke, the onset is rapid, with a predominance of cerebral symptoms.
There are several stages in the development of a stroke: the acute period (from the moment of the stroke to 3 weeks on average), the recovery period - from 2 weeks to 24 months.
Indications for intravenous thrombolysis
- The period from the onset of the first symptoms of a stroke is no more than 3 hours
- No history of stroke
- Absence of traumatic brain injury and myocardial infarction for 3 months
- No gastrointestinal bleeding for 3 weeks
- No abdominal surgeries for 2 weeks
- systolic blood pressure is less than 180 mmHg; Diastole blood pressure less than 110 mmHg
- If anticoagulants were previously prescribed, the INR should be below 1.7; the patient did not take warfarin, phenylin
- platelet count greater than/equal to 100,000 mm
- glucose content is greater than/equal to 2.7 mmol/l and not more than 22.5
- Absence on CT of signs of multifocal and extremely extensive infarctions (more than 1/3 of the hemisphere)
- The patient and his relatives should be aware of the potential effect and risk of thrombolysis
Monitoring the patient during thrombolysis
The general condition of the patient is assessed by the doctor during thrombolysis every 15 minutes, every 30 minutes for 6 hours after thrombolysis, then every hour until 24 hours have elapsed from the start of thrombolysis.
If a severe headache, nausea, or vomiting occurs, thrombolysis is stopped and a CT scan is urgently performed. Blood pressure is measured every 15 minutes for the first 2 hours, every 30 minutes for the next 6 hours, and then every hour until 24 hours after the start of thrombolysis.
When systolic blood pressure is greater than/equal to 180 mmHg or diastolic blood pressure is greater than/equal to 105 mmHg. antihypertensive drugs are prescribed (lobetalol 10 mg over 1-3 minutes, if necessary, the same dose is repeated every 10-20 minutes, maximum dose 300 mg).
Despite its proven effectiveness, thrombolytic therapy is used in European countries only in 1-7% of patients with ischemic stroke, which is due to strict criteria for selecting patients for this treatment method.
What to do if you have a stroke
There are techniques that allow you to identify signs of a stroke yourself. For example, they can be used if someone becomes ill on the street and you suspect a stroke. You need to ask the person to smile, speak, raise both hands. If the victim cannot comply with your request or there is asymmetry, you should immediately call for help and list all the symptoms.
At the same time, you need to provide first aid: lay the victim down, placing a small support under his head, and free him from clothes that are preventing him from breathing. He should not eat or drink or make sudden movements. When vomiting, turn your head to the side.
Further treatment is carried out in a hospital. First, diagnostics are carried out to clarify the diagnosis; computed tomography and magnetic resonance imaging, lumbar puncture and EEG (echoencephalography), angiography are prescribed. Then conservative (basic therapy, treatment of neurological complications) or surgical treatment is prescribed.
After the end of the acute period, rehabilitation is prescribed: massage, physical therapy and other activities, depending on the degree and type of disorder. The patient is observed by a neurologist, physiotherapist, speech therapist, and psychotherapist.
The brain has neuroplasticity: with the right approach, you can recover from a stroke, restore brain function and prevent stroke complications. The key factor is timely initiation of treatment, proper rehabilitation and regular exercise.
According to WHO, about 60% of patients do not require assistance by the end of the first year, and 30% of patients of working age can return to work.
Rehabilitation of patients after hemorrhagic stroke
The main task is to restore body functions that were damaged as a result of hemorrhage.
Rehabilitation must begin immediately after the operation. Doctors use an integrated approach to treat patients, which includes taking medications, changing diet and lifestyle, and choosing the right physical activity.
After a stroke, the patient requires long-term recovery. The help of loved ones and medical workers, compliance with all doctor’s instructions is required.
At first, the patient is in a hospital, then the rehabilitation program continues at home and in an outpatient setting.
In addition to taking medications, you will need additional therapy and auxiliary methods that will alleviate the condition and allow you to gradually return to normal activities:
- The patient is advised to exclude fatty and fried foods from the diet and eat food sparingly throughout the day in small portions. If swallowing is difficult, feeding is done through a tube.
- It is required to maintain sleep hygiene: go to bed and wake up at the same time, avoid active activities, and watch TV before bed.
- Physical activity – as far as possible for the patient, without tension and increased strength loads.
- It is necessary to perform physical therapy exercises. Initially, the physiotherapist prescribes passive gymnastics, which is performed by a medical professional or the patient’s relatives, then the exercise complex is expanded, and the degree of load gradually increases. The goal of physical therapy is to restore basic physiological capabilities.
- If speech functions have been damaged, sessions with a speech therapist are necessary.
Prevention
- Primary prevention consists of proper nutrition, exercise, giving up bad habits and stress, adequate sleep and rest, and regular medical examinations.
- Secondary prevention of stroke includes the elimination of risk factors - treatment of concomitant pathologies, regular monitoring by the attending physician, elimination of risk factors. This approach will help not only prevent stroke, but also improve overall health. According to WHO estimates, the creation of an adequate system of care for patients with stroke will make it possible in the coming years to reduce mortality during the 1st month of the disease by 20% and ensure independence in everyday life 3 months after its onset in at least 70% of patients.
Diagnosis of the disease
During the initial examination, the doctor collects anamnesis and conducts a neurological examination. In some cases, this is enough to make a diagnosis and classify the disease. If localization cannot be established, additional examinations are prescribed.
What diagnostic methods are used:
- emergency general and biochemical blood test;
- ECG;
- coagulogram to assess blood clotting;
- CT;
- MRI.
The images allow you to determine the location of the damaged area, its size and damage to the brain.
If it is necessary to identify the source of hemorrhage, CT angiography is prescribed.
FAQ
How is a stroke different from a heart attack?
Cerebral infarction is one of the types of stroke and it is ischemic in nature, i.e. accompanied by a cessation of blood flow to the brain. A characteristic feature is the gradual development of the clinical picture and the predominance of focal symptoms: disturbances in speech, vision, gait, movements up to paralysis, sensitivity.
Can a stroke and heart attack happen at the same time?
If we consider only the brain, mixed stroke occurs, when the causes of stroke include both hemorrhage and ischemia. They can occur simultaneously when a vessel ruptures in one area and blood flow stops in another. Also, ischemia can develop at the site of subarachnoid hemorrhage after some time.
If we consider a heart attack as a heart disease, then these conditions can also be diagnosed simultaneously. Moreover, a stroke can develop as a result of a heart attack: the functioning of the heart suffers, and insufficient blood flows to the brain. This is how we get a stroke.
Does a stroke only occur in the brain?
Stroke (Latin insultus “swoop, attack, blow”) is an acute disruption of the blood supply to the brain due to ischemia (infarction) or hemorrhage. If ischemia occurs in other organs, it is also called a heart attack. For example, myocardial infarction, intestinal, kidney, etc. It is characterized by severe pain, dysfunction of the affected organ and other symptoms.
Does stroke occur with normal or low blood pressure?
Arterial hypertension is one of the main, but not the only causes of stroke. Thrombosis, atherosclerosis, and diabetes mellitus, in which blood pressure is normal or even reduced, are also risk factors. In addition, with low pressure, the brain is not sufficiently supplied with oxygen, which is a prerequisite for the development of ischemic stroke.
Do children have strokes?
Stroke is also diagnosed in children. It can develop even in the perinatal period. Causes: abnormalities in the coagulation system, pathologies of the cardiovascular system, including vascular malformations, bad habits of the mother during pregnancy, oxygen starvation during childbirth, trauma.
In the perinatal period and up to one year, the disease is accompanied by anxiety, frequent crying, loss of appetite, impaired reflexes in the newborn period, strabismus, and convulsions. The diagnosis is made based on an examination by a pediatric neurologist, ultrasound of the brain, and tomography results. At older ages, symptoms are similar to those of stroke in adults.
The child's body is more flexible and responds more quickly to therapy. The main thing is to diagnose a stroke in time and begin treatment.
Can a stroke go away on its own?
There is such a condition - transient stroke. It is accompanied by a short-term circulatory disorder, but no irreversible changes in brain tissue occur. The external manifestations of such a stroke are the same as a normal one, but less pronounced: headache, dizziness, darkening of the eyes, changes in sensitivity in various parts of the body. And they pass within 24 hours. However, the condition requires qualified treatment and rehabilitation, elimination of risk factors, because in the future there is a possibility of a secondary stroke.
At what pressure can a stroke occur?
A stroke can develop at any pressure. Arterial hypertension causes hemorrhagic stroke, hypotension causes ischemic stroke.
Do pine cones help prevent stroke?
Pine cones lower blood pressure, so they should not be consumed if you have hypotension. The effect is due to the tannins contained in the buds. The composition also contains vitamins C and P - they strengthen the walls of blood vessels and improve blood circulation.
The advisability of using products based on herbal raw materials is decided by the attending physician after a detailed examination. In general, pine cones for stroke can only be used as a complementary method.
Temperature values
What does the temperature reading after a stroke indicate? It characterizes the degree of brain damage and reflects the dynamics of the victim’s recovery.
Based on the fluctuations of this criterion, it is customary to distinguish several values:
- Moderate hyperthermia – the level does not exceed subfebrile values (up to 37.50 C). May be a variant of the norm. The optimal value after a stroke is considered to be 37.20 C, but a deviation of 1 degree is not critical.
- If the readings increase above 38 degrees, further examination is necessary to determine the cause.
- A low temperature of up to 36.0 °C during an ischemic attack is a positive characteristic.
Based on the marks on the thermometer, you can predict the outcome of the disease. The higher they are, the less likely a person is to recover from a stroke. The temperature does not change immediately after the stroke is stopped, however, the later it rises, the worse the prognosis for the patient.
Complications of hyperthermia
Changes caused by high temperature during a stroke:
- acceleration of metabolism due to oxygen deficiency,
- necrosis of the inflammation focus,
- blood flow disturbance,
- expansion of the cerebral infarction zone during ischemia,
- focal changes in the structure of matter.
Without a rapid decrease in numbers, post-stroke pathologies develop, which can lead to a person’s disability or result in his death.
Violations during the rehabilitation period
The rise in temperature even after an impact is life-threatening. It does not matter whether the person suffered an ischemic or hemorrhagic type of stroke. Research by specialists shows that when hyperthermia occurs within a month, there is an increase in mortality. Factors contributing to the increase in indicators:
- the presence of an infectious process,
- insufficient patient care,
- bedsores,
- tracheostomy,
- diseases of the lower respiratory tract.
Despite the temperature deviation from the norm, the patient may not complain of health, there is no pain. A characteristic symptom of the complication is the low effect of taking antipyretics.
The longer the temperature remains outside the normal range, the greater the pressure on tissues and the higher the likelihood of complications.
.
Consequences of rising temperatures
Against the background of increased oxidative reactions in tissues, their need for oxygen simultaneously increases. Without restoration of normal blood supply, hypoxia quickly sets in. In the absence of adequate therapy, the rehabilitation process slows down, the patient may fall into a coma or die.