Brain glioma: life expectancy, symptoms, causes and treatment
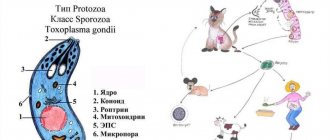
Brain glioma is a disease that includes a group of tumor pathologies localized in the meninges. The impetus for the development of gliomas is pathologically overgrown auxiliary cells of the nervous system.
Gliomas account for more than half of all brain tumors; the disease affects not only adults, but also children. The life expectancy of patients depends on the degree of tumor.
Causes of tumor
Scientists have found that neoplasms appear due to the rapid proliferation of immature glial cells. This is how benign and cancerous gliomas appear.
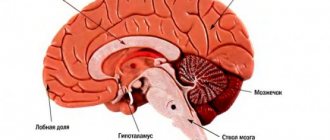
Tumors form in the gray or white matter around the central canal, in the posterior part of the pituitary gland, cells in the cerebellum, or in the retina. Glioma develops slowly from the volume of a small grain to a round body with a diameter of 10 cm. Metastases spread in rare cases. The exact reasons for the growth of cancerous glioma have not been determined, but scientists are inclined to believe that they lie at the genetic level when the structure of the TP53 gene is disrupted.
It is difficult to treat this disease precisely because it is poorly understood. This tumor has clear contours and affects one area of the brain. Metastases almost never develop.
Classification
Gliomas include a variety of tumors depending on which cells are affected. Thus, they can arise from ependyma, astrocytes and other cells. The most common types are:
- Ependymoma - occupies about eight percent of all brain tumors, mostly affecting the ventricles;
- Diffuse astrocytoma - this disease occurs in every second case. This tumor is usually located in the white matter of the brain. The most common glioma is the brainstem;
- Mixed tumors - include altered cells from the above types, can occur in any part of the brain;
- Oligodendroglioma is a pathology that occurs on average in every tenth patient out of a hundred. Localized along the ventricles, can grow into the cerebral cortex;
- Neuromas - a tumor originating from the myelin sheaths, is benign in nature, but can provoke tissue malignancy. This is an optic nerve glioma or chiasmal glioma;
- Vascular tumors are a rare brain pathology with tumor growth into the vessels;
- Neuronal-glial tumors are the rarest type of disease; both neurons and glial tissue are involved in the pathological process.
Classification of gliomas
First of all, any neoplasm in the body is divided into:
- malignant, with rapid growth and the ability to metastasize;
- benign, slow-growing and usually surrounded by a capsule that prevents it from growing into nearby structures.
It must be remembered that in relation to tumors of the central nervous system, this fact is of conditional significance. After all, any “plus tissue” in the cranial cavity that creates additional volume sooner or later leads to swelling and displacement of the brain. And this can ultimately cause death.
Gliomas are also classified according to their location into:
- supratentorial, located above the “roof” of the cerebellum in the cerebral hemispheres, lateral ventricles;
- subtentorial, lying below this level in the posterior cranial fossa.
It is equally important to distinguish between neoplasms according to histological characteristics, that is, taking into account the cells from which it was formed and the degree of malignancy. After all, the choice of treatment method depends on this.
By origin
Brain glioma, according to the WHO classification, is classified as a neuroepithelial tumor group. And depending on which glial cells it originated from, it is classified into:
- astrocytic glioma. In the structure of neoplasms, the central nervous system takes first place, as it occurs in 50% of cases. It can be benign nodular (for example, piloid astrocytoma) and malignant diffuse (anaplastic astrocytoma, glioblastoma). The latter form can occur at lightning speed with signs of a stroke;
- oligodendroglioma, which is observed in only 5% of patients. A distinctive feature of the neoplasm is the presence of petrification in its thickness, that is, areas of calcification. This “plus tissue” is located in half the cases in the frontal lobe;
- ependymal glioma. This tumor grows from cells lining the walls of the ventricles and the central spinal canal. At the same time, it is capable of spreading both into their lumen and into the thickness of the brain substance.
There are also mixed forms of pathology - oligoastrocytoma and subependymoma, or subependymal astrocytoma.
According to the degree of malignancy
Brain glioma is classified according to the degree of malignancy, which is determined by the rapid growth of the tumor and the atypicality of its cells. Highlight:
- Grade I gliomas, which take many years to significantly increase in size. Typically, such “plus tissue” is delimited from healthy cells by a capsule. These include piloid astrocytoma, pleomorphic xanthoastrocytoma, etc.;
- second-degree gliomas are borderline neoplasms that have a certain degree of atypia and easily degenerate into more dangerous tumors;
- third-degree gliomas, for example, anaplastic astrocytoma, consist of cells that are strikingly different from healthy ones as a result of disrupted mitosis processes and the presence of altered nuclei;
- Grade IV gliomas have lightning-fast growth and are accompanied by necrosis inside the tumor and destruction of the vessels supplying it.
It must be remembered: the lower the degree of malignancy, the less often the pathological process relapses and the greater the chance of recovery for the patient.
Glioma symptoms
The symptoms of a growing glioma directly depend on which part of the brain the tumor occupies. The neoplasm compresses tissues and membranes, which leads to cerebral symptoms:
- Severe headaches that cannot be relieved by taking analgesics and antispasmodics.
- The appearance of heaviness in the eyeballs.
- Nausea resulting from headaches. Patients also complain of periodic vomiting, which also occurs at the peak of an attack.
- Cramps.
If a glioma compresses the cerebrospinal fluid pathways and ventricles of the brain, hydrocephalus develops and intracranial pressure increases. In addition to general cerebral symptoms, glioma also affects the occurrence of focal manifestations of the disease, these are:
- Dizziness.
- Unsteadiness during normal movement.
- Visual impairment.
- Hearing loss or tinnitus.
- Speech function disorder.
- Decreased sensitivity.
- Decreased muscle strength, which causes paresis and paralysis.
In patients with brain glioma, mental changes are also detected, expressed by disorders of all types of memory and thinking, and certain disturbances in behavioral function.
Symptoms
General cerebral clinical symptoms include:
- Chronic headache that is not relieved by painkillers.
- Nausea and vomiting.
- Discomfort and pressing sensations in the eye sockets.
As the disease progresses, the outflow of cerebrospinal fluid is disrupted, resulting in hydrocephalus (water on the brain).
Focal symptoms of this disease include vestibular ataxia, decreased visual acuity, decreased tactile and pain sensitivity, decreased muscle tone, and mental disorders.
Stages of development
According to the international classification of diseases, the stages of tumor development are assessed according to the degree of danger to the patient’s life. It is customary to divide the disease into four groups or stages of development:
- 1st degree – benign formation with a tendency to slow development. Has the most favorable course of the disease. With timely measures taken, it is possible to extend the patient’s life to 8-10 years. This grade corresponds to congenital benign glioma.
- Grade 2 – the tumor begins to slowly but steadily increase in size. The first signs of degeneration into a malignant formation appear. Signs of deterioration are manifested in a constant increase in neurological and other symptoms.
- Grade 3 – anaplastic glioma. At the third stage, the disease has symptoms characteristic of a malignant neoplasm. Life prognosis does not exceed 2-5 years. There is no metastasis to other areas of the body, but sometimes the spread of cancer to different parts of the hemispheres is observed.
- The prognosis for diffuse brainstem glioma is extremely unfavorable. The patient rarely lives more than 2 years.
- Grade 4 – a large tumor of a malignant nature with a tendency to rapid tumor growth. The prognosis is unfavorable. The patient's life expectancy is up to 1 year. At this stage, inoperable malignant glioma is diagnosed.
Diffuse glioma in young patients is treated radiologically. After a short-term improvement, the disease returns in a more severe form.
Diagnostics
Low-grade gliomas are very rarely diagnosed in the initial stages because they may not have clinical symptoms. In most cases, they are discovered during computed tomography or magnetic resonance imaging after traumatic brain injury or to evaluate vascular disease. In such situations, brain examinations are prescribed by neurologists. When losing vision or hearing, patients turn to specialists in a narrow field, who must be aware of insidious pathologies in the brain.
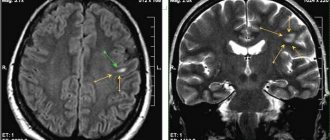
To adequately assess brain glioma, the patient is referred for magnetic resonance imaging. It is this type of diagnosis that allows you to accurately determine the location of the tumor, its volume and the affected area in a three-dimensional image.
Depending on the symptoms, the patient may be referred for echoencephalography, multivoxel or magnetic resonance spectroscopy, or positron emission tomography. For the most accurate diagnosis, a biopsy is prescribed - a microscopic examination of part of the biological material.
Glial tumors
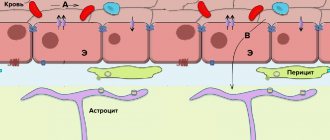
Glial tumors belong to the group of primary intracerebral tumors, since the source of their growth is neuroglial cells (astrocytes, oligodendrocytes) - tissue that provides the structural framework and vital activity of brain neurons.
In neuro-oncological practice, these tumors occupy almost a leading position, second only to metastatic tumors in frequency of occurrence. The modern classification of glial tumors is quite extensive and the format of this article does not allow us to cover all the features of these tumors. However, it is worth noting that glial tumors are very heterogeneous in their structure, the presence of certain genetic mutations, aggressiveness, clinical course, diagnostic features, susceptibility to treatment and the overall prognosis for the lives of patients. Other in histological structure, but similar in treatment strategy, are ependymal and embryonal tumors of the central nervous system, among which the most common are ependymomas and medulloblastomas.
All gliomas are divided according to the degree of malignancy into 4 degrees:
Grade I gliomas , such as piloid (pilocytic) astrocytomas, are well demarcated from healthy brain tissue, grow slowly, and their pathological impact is determined almost exclusively by size and location in the brain
Gliomas of the second to fourth degrees are prone to infiltrative growth and do not have a clear border with healthy brain tissue. This is one, but not the only factor that influences the aggressiveness of the course of such tumors, as well as the choice of possible treatment methods and their effectiveness.
Of particular note is the ability of some diffuse astrocytomas to progress (mutate) over time and acquire a more aggressive (malignant) course. A typical example of this is diffuse (grade II) and anaplastic (grade III) astrocytomas progressing to glioblastoma (grade IV)
Some grade III-IV tumors can metastasize within the brain and spinal cord (anaplastic ependymomas, medulloblastomas, less commonly, anaplastic astrocytomas), or are prone to multifocal growth (glioblastomas). The literature describes isolated cases of extracerebral metastasis of malignant gliomas.
Which diagnostic method is best to use for glial tumors?
Computed tomography is informative only for identifying the localization of the pathological focus, the presence of perifocal edema, and compression of the brain. It is not informative in the differential diagnosis of various types of gliomas.
Magnetic resonance imaging (MRI) . Almost the entire range of MRI scanning modes is used, including contrast enhancement, spectroscopy, ASL perfusion and others. Based on MRI data, in most cases one can assume the benign or malignant nature of the tumor, and even suggest its histological variant, but it is impossible to establish a reliable histological diagnosis.
Positron emission tomography (PET) uses brain-specific metabolites that selectively accumulate in the tumor. Fluorodeoxyglucose, widely used in the diagnosis of extracranial tumors, is not specific to glial tumors and is not used in their diagnosis. Radioactively labeled methionine and fluorocholine are most widespread and important in neurooncology.
Biopsy. The biopsy material is collected either by stereotactic puncture with a special needle through a small (up to 1 cm) trefination hole, or during surgery. Tumor tissue is not only examined under a microscope, but also undergoes a series of complex tests for the presence of certain biochemical factors, mutations and other signs, on the basis of which not only an accurate diagnosis is established, but also a prognosis for the further development of the disease and the potential sensitivity of the tumor to drug therapy is determined.
How to treat glial tumors?
First-degree gliomas respond quite well to surgical treatment, the effectiveness and radicality of which is determined mainly by the localization of the tumor and the involvement of functional areas of the brain.
Gliomas of the second to fourth degree require combined treatment. In most cases, it is based on surgery - aimed at removing or reducing the volume of the tumor that puts pressure on the brain, radiotherapy - in the standard fractionation mode with marginal coverage up to 5-20 mm, 1.8-2 Gy (depending on the degree of malignancy) per 30 sessions and chemotherapy , which in some cases can be prescribed simultaneously with a course of radiation therapy. A special method of irradiation is craniospinal irradiation , in which, in addition to the tumor itself (most often anaplastic ependymomas and medulloblastomas) or its postoperative bed, the entire brain and spinal cord is irradiated to affect or prevent the appearance of tumor metastases along the cerebrospinal fluid pathways of the central nervous system. Recently, as in general oncology, drugs with a targeted effect on tumors have appeared and are constantly being improved - targeted therapy , which suppress the work of enzyme systems of tumor cells, growth factors of tumor vessels, but are not true toxins in relation to cells.
Radiosurgery . Despite the widespread idea of radiosurgery in general, and of the Gamma Knife in particular, as a panacea for all tumors, this is not true in the case of grade 2-4 gliomas. And the most significant point that determines the limited use of radiosurgery is, oddly enough, the “targeting” of radiation with a high dose gradient at the tumor/healthy brain boundary, because this border is difficult and very conditionally determined using MRI and SCT. Even the additional information that PET provides does not reflect the true picture of the process.
However, Gamma Knife is used in the following cases :
- small, well visualized and with clear contours according to MRI, tumors with confirmed benign (grade I) histology (by stereotactic biopsy) or with low metabolic rates according to PET with methionine or fluorocholine
- remains of benign (grade I) tumors after surgery
- relapses of benign (grade I) astrocytomas after previous removal
- continued local growth of gliomas, ependymomas and medulloblastomas, as well as the appearance of new ones, incl. multiple sites of their growth in the brain at a distance from the primary focus, provided that a full course of radiation therapy has previously been completed and there are no prospects or limited possibilities for further systemic treatment (chemotherapy, targeted therapy).
Treatment of brain glioma
The only method that helps achieve significant improvements in the patient’s well-being is brain neurosurgery. The operation is complicated by the fact that any mistakes by the surgeon lead to serious dysfunction of the human body, paralysis and death.
Removal of brain glioma is carried out using several methods:
| Endoscopy | Using an endoscope, surgical instruments and a video camera are inserted into the cranial cavity. After the tumor is removed, chemotherapy is given. Repeated operations to remove glioma are required in more than 50% of cases. |
| Radiotherapy | used in the initial stages of cancer and as a preventive method after surgery. |
Glioma has genetic causes of formation. Therefore, after surgery, the tumor may form again. The use of genetic engineering drugs can reduce the size of a malignant tumor and facilitate surgery.
These newer drugs target cancer cells, killing them. The size of the tumor does not change, the patient can live longer without pain. Genetic engineering drugs make it possible to avoid repeated surgery.
Treatment
Complex treatment includes surgery, radiation and chemotherapy, as well as radiosurgical techniques. Radiation and chemotherapy are equally used both for inoperable gliomas and at the postoperative stage.
Surgical method
Complete surgical removal of the tumor is only possible if the tumor has no signs of atypia. In all other cases, the glioma cannot be completely removed. The effectiveness of operations to remove gliomas has improved thanks to the use of intraoperative brain mapping techniques, during which an accurate model of the patient’s brain is built and the exact location of the tumor is indicated.
Chemotherapy
For chemotherapy of brain gliomas, drugs such as Temozolomide, Carmustine and Vincristine are used. Pan-European chemotherapy protocols are used to create an individual treatment plan.
Radiation therapy
Radiation exposure for brain gliomas is used both at the preoperative and postoperative stages. Before surgery, radiation therapy can reduce the size of the tumor, and after surgery, radiation exposure destroys the remains of atypical cells and helps avoid relapse. Also, this method is used for inoperable gliomas to reduce the growth rate of the tumor.
Radiosurgery
Stereotix radiosurgery techniques are used to treat small gliomas that do not grow into nearby tissues. The Cyber Knife and Gamma Knife systems are used for therapeutic purposes.
Folk remedies
Despite the dubious effectiveness of alternative medicines, many traditional healers and herbalists recommend using mistletoe decoction, Aconite, horse chestnut decoction and propolis tincture for therapeutic purposes for brain glioma.