Non-immunological, caused by many factors, such as:
- infectious diseases;
- cardiovascular diseases;
- chromosomal abnormalities;
- malformations of the lungs or urinary tract;
- anemia (due to thalassemia or iron deficiency);
- episodes of congenital diaphragmatic hernia;
This clinical condition is found in approximately 1 in every 3000 pregnancies, but its incidence is generally underestimated due to the high likelihood that embryos/fetuses with this anomaly will result in early spontaneous abortions.
However, in approximately half of cases, hydrops fetalis is detected during an ultrasound examination performed in the third trimester of pregnancy, which may be followed by amniocentesis or periodic morphological ultrasound examinations aimed at establishing the severity.
Symptoms affecting the fetus or newborn vary depending on the severity of the clinical presentation and range from "mild" manifestations such as ascites or pallor and, in the most severe forms, the appearance of swelling and bruising of the skin (purple colored patches on the skin), severe anemia or pictures of respiratory distress or heart failure, which can also be fatal and cause serious concern to the doctor and the couple regarding the prognosis of the case.
Before diagnosis, expectant mothers may experience fetal hydrops as a decrease in fetal movement, and later the pregnant woman may develop “mirror syndrome,” characterized by a number of symptoms:
- anasarca (massive and diffuse swelling, subcutaneous, non-inflammatory);
- proteinuria (loss of protein in urine);
- hypertension.
Fetal death occurs in 55-98% of cases of nonimmune hydrops and, depending on the etiology, is usually due to heart failure and hypoxia.
Thanks to the ability to give women with Rh incompatibility a drug called RhoGAM (Rho immunoglobulin), fetal immune hydrops can be prevented, so its incidence has decreased significantly in recent years.
Clinical picture
The first symptoms of non-immune fetal hydrops can be seen on ultrasound. These include:
- decreased fetal activity;
- subcutaneous edema;
- ascites;
- tachycardia;
- the presence of fluid in the body cavities;
- polyhydramnios;
- enlarged heart;
- the abdomen is enlarged due to ascites.
A woman may experience symptoms such as hypertension and massive edema.
But the most obvious signs are observed immediately after birth. The clinical picture makes it possible to almost accurately identify the disease:
- First of all, the baby’s serious condition is observed.
- The sutures of the skull are open, the fontanelle is protruding.
- Swelling is observed.
- Subcutaneous tissue is poorly expressed, so body temperature is dependent on the environment.
- Suppression of reflexes and low blood pressure are also diagnosed.
- Ascites is often noted.
- Enlarged liver and spleen.
Why is this happening?
At the heart of fetal swelling is an accumulation of fluid that affects the fetal body, often the reason for this is:
- causes of severe complications;
- infectious diseases;
- immunological abnormalities.
The first important distinction that can be made concerns the immune or non-immune nature of this clinical condition:
- Immune hydrops: occurs due to a reaction occurring between antibodies to fetal red blood cells produced by the mother and antigens (the target of these antibodies) that are very often present in fetal blood cells (also called red blood cells) due to incompatibility with the maternal Rh factor;
- Non-immune hydrops: This condition is usually caused by increased interstitial fluid or lymphatic obstruction, potentially caused by several factors.
Including:
- cardiovascular diseases;
- arrhythmias;
- embolism;
- myocarditis;
- congenital anomalies such as tetralogy of Fallot or Ebstein malformation;
- chromosomal abnormalities such as Turner syndrome, trisomy 21, or Noonan syndrome;
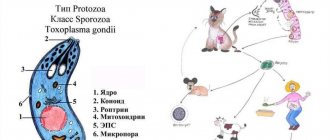
- infections, mainly;
- toxoplasmosis;
- rubella;
- chicken pox;
- syphilis;
- cytomegalovirus;
- herpes virus;
- parvovirus;
- AIDS and Lyme disease;
- urinary tract malformations or pulmonary malformations.
Hematological causes: including:
- thalassemia;
- bleeding;
- arteriovenous shunts;
- Iron-deficiency anemia;
- congenital diaphragmatic hernia;
- congenital metabolic defects;
- transaldolase deficiency;
- mucopolysaccharidosis;
- Niemann-Pick disease;
- twin pregnancy with fetal transfusion syndrome;
- severe pathological conditions of the mother;
- diabetes;
- hypoproteinemia;
- anemia;
- preeclampsia.
Consequences
With non-immune fetal hydrops, the consequences for the child in the future can be quite serious. Even when diagnosing pathology at an early stage of its development, there is a risk of complications, among which the most common are the following:
- pathologies of the respiratory system;
- severe pathologies of the brain and cardiovascular system;
- pathology of the skin;
- cardiovascular failure;
- cryptorchidism in boys;
- death.
What are the complications?
This clinical condition is found in approximately 1 in every 3000 pregnancies, but its incidence is generally underestimated due to the high likelihood that embryos/fetuses with this anomaly will result in early spontaneous abortions.
Fetal death occurs in approximately 55-98% of cases of nonimmune hydrops and, depending on the etiology, is usually due to heart failure and hypoxia.
In cases of immune hydrops fetalis, which may therefore be associated with maternal-fetal Rh incompatibility, pathological neonatal jaundice with deposition of bilirubin in the brain tissue can be observed.
diabetes
Nonimmune hydrops fetalis. Lecture notes
Definition. Non-immune hydrops fetalis (NIHF) is a pathological condition characterized by excessive accumulation of fluid in the serous cavities and soft tissues of the fetus, not associated with blood type incompatibility or maternal Rh factor [1].
Frequency. Given that the incidence of immune hydrops fetalis has decreased due to the widespread use of Rh sensitization prophylaxis, NIHF has become the dominant form of hydrops fetalis (occurs in 2/3 of cases). Its incidence in large studies is one in 250–350 pregnant women.
Pathogenesis of non-immune hydrops fetalis:
- primary myocardial or heart failure (congenital heart defects, arrhythmias or myocarditis);
- secondary myocardial or heart failure (severe anemia, atrioventricular shunt, placental tumor or feto-fetal transfusion syndrome);
- a drop in oncotic pressure (caused by a decrease in protein production due to congenital cirrhosis or hepatitis (infection) or an increase in protein loss associated with congenital nephropathy; hypoproteinemia leads to a decrease in oncotic pressure, which determines secondary damage to the capillaries and leads to additional protein losses);
- increased capillary permeability (severe hypoxia, infections, severe anemia, other reasons);
- obstruction or disturbance of lymphatic drainage (Turner's syndrome, chylothorax, chyloperitoneum);
- venous return obstruction (congenital adenomatous cystic malformation or diagram defect[2].
I. Cardiac causes:
- heart defects (left ventricular hypoplasia, atrioventricular canal, transposition of great vessels, tetralogy of Fallot, vascular atresia, dysplasia and stenosis, Ebstein anomaly, large ventricular septal defect, single ventricle, occlusion of the ductus arteriosus or foramen ovale);
- arrhythmias (tachyarrhythmia, supraventricular paroxysmal tachycardia (PSVT), atrial flutter, WPW syndrome, bradyarrhythmia, AV block, sinus node disorders);
- heart tumors (rhabdomyoma, teratoma);
- cardiomyopathy;
- atrioventricular shunt;
- heart failure (sacrococcygeal teratoma, chorangioma, vein of Galen aneurysm, feto-fetal transfusion syndrome (recipient));
II. Chromosomal pathology (monosomy on the X chromosome (Turner syndrome), trisomy on chromosome 21, triploidy, other trisomies (13, 18)).
How is the diagnosis made?
Diagnosis is made by a doctor through a history, clinical assessment and other tests such as:
- Ultrasound: reveals fluid accumulation in the second/third trimester of pregnancy and thickening of the placenta (> 5 mm) associated with the appearance of ground glass, which may indicate non-immune hydrops fetalis;
- Laboratory tests of the mother: blood group typing, detection of antibodies to fetal red blood cells (if fetal hydrops is suspected of an immunological nature), screening of antibodies to TORCHES-CLAP (to exclude a possible infectious etiology), hemoglobin electrophoresis. (if thalassemia is suspected), analysis for antibodies to SSA-SSB and alpha-fetoprotein, Kleihauer-Betke test (as part of assessing the compatibility of mother and fetus by Rh factor);
- Amniocentesis and serial morphological ultrasound examination: these are additional diagnostic tests aimed at establishing the severity of the clinical picture.
Diagnostic measures
To identify a pathological condition and the nature of its occurrence, a set of diagnostic measures is used. Let's look at them in more detail:
- The main diagnostic measure is ultrasound, which can reveal intrauterine signs of pathology and the degree of their development.
- The blood type and Rh factor are determined. This study is very important to exclude the immune nature of the disease.
- The doctor conducts a survey of the pregnant woman, which clarifies the presence of chronic diseases, infections and surgical interventions performed. Complications that arise during pregnancy and the general course of pregnancy are also important.
- General analysis of urine and blood.
- Blood chemistry.
- ECG.
- Examination of a woman for infections.
Intrauterine examinations of the fetus are prescribed to confirm non-immune hydrops fetalis during pregnancy:
- Examination of amniotic fluid.
- Cordocynthesis.
- PCR for suspected infections.
- Dopplerography.
What to do?
Treatment for hydrops fetalis is largely determined by the underlying causes and the presence of progressive symptoms.
In the prenatal phase, a therapeutic strategy can be developed only under certain circumstances and in the presence of anemia; Treatment is mainly based on intrauterine fetal blood transfusion.
In the most serious cases, when therapeutic intervention is not possible, premature delivery of the fetus using drugs that can induce labor or by caesarean section is indicated.
In the neonatal or postpartum period, the following are possible:
- blood transfusion (to remove any maternal antibodies to fetal red blood cells);
- pleural or abdominal drainage (fluid accumulated in these tissues can be aspirated with a syringe);
- artificial ventilation: for respiratory failure;
- taking medications to treat heart failure;
- stimulating diuresis with diuretics, which encourage the kidneys to excrete excess fluid.
MAKE AN APPOINTMENT
Abortion and contraception clinic in St. Petersburg - department of the medical gynecological association "Diana"
Make an appointment, tests or ultrasound via the contact form or by calling +8 (812) 62-962-77. We work seven days a week from 09:00 to 21:00.
We are located in the Krasnogvardeisky district, next to the Novocherkasskaya, Ploshchad Alexander Nevsky and Ladozhskaya metro stations.
The cost of a medical abortion in our clinic is 3,300 rubles. The price includes all pills, an examination by a gynecologist and an ultrasound to determine the timing of pregnancy.