Enamel hypoplasia is a non-carious lesion of teeth that occurs before tooth eruption during the development of its tissues. The term “enamel hypoplasia” is conditional, since changes are also observed in other tooth tissues - dentin and pulp.
Terminology of dental enamel hypoplasia
Dental enamel hypoplasia is a qualitative and quantitative violation of tooth enamel. This definition of the disease is most often found in Russian-language literature. In international sources, enamel hypoplasia (including prenatal and neonatal) refers only to its quantitative changes - thinning, pits, grooves. Qualitative changes (changes in color, transparency) in foreign literature are opacity, hypomineralization, dismineralization and non-endemic mottling of enamel (ICD-C).
Causes of occurrence and code according to ICD 10
The main cause of the disease is an insufficient amount of nephrogenic tissue.
Its components are structurally and functionally sound, so the kidney affected by hypoplasia is small in size, but its structure does not suffer in any way.
The code in the International Classification of Diseases, Tenth Edition is Q 60.5.
The pathology is congenital and is usually detected in children.
In cases where a healthy kidney fully performs the functions of 2 organs, the disease can be detected in adults when complaints of increased pressure and swelling appear.
Typically, signs appear as a result of previous pyelonephritis or under the influence of unfavorable environmental factors.
In the fetus
Pathology is formed at the stage of intrauterine development. There can be many reasons: hereditary predisposition, oligohydramnios, maternal infections (rubella, measles), fetal pyelonephritis, abnormal presentation, kidney bruises.
The lifestyle of a pregnant woman matters. If she smokes, drinks alcohol, stays in the sun for a long time, or is exposed to ionizing radiation, the risk of developing hypoplasia increases.
Pathology of the newborn
In newborn children, the pathology is diagnosed during the first days of life if there is bilateral damage. Unilateral hypoplasia is also recorded in cases of impaired urinary function, the presence of pathological reflexes, uncontrollable vomiting, and intoxication. The reasons for the development of the disease are the same as in the fetus.
Illness in a child
The etiology of the pathology in a child is the same as in children of the first year of life. In the presence of a healthy kidney, the clinical picture may be completely absent, but with inflammatory processes in the organ, the condition may worsen.
In such situations, symptoms of hypoplasia arise and a characteristic clinical picture of the disease is formed.
Often the diagnosis is made during a medical examination before the child enters kindergarten or school. The child may feel completely healthy.
Clinical picture
In the case of damage to one kidney and the full functioning of the second, the symptoms of the pathology may not appear during the entire life of the patient.
If this does not happen, the organs are prone to inflammation, then such patients often suffer from pyelonephritis.
They are worried about pain, frequent urination, and increased body temperature.
Patients are often diagnosed with arterial hypertension, which is difficult to correct with medications. Removal of the affected kidney is often required.
Patients have pale skin, swelling of the face and upper body in the morning. Chronic renal failure often develops.
Symptoms in a child
Children suffering from hypoplasia, in addition to the above symptoms, have complaints of nausea, low-grade fever, bloating, hair loss, and diarrhea.
They lag behind in mental and physical development, the skeletal system does not correspond to their age (the structures of the skull protrude, the legs are bent).
Urination in children can be painful, mixed with pus and blood. They often complain of weakness, thirst, and pain in the lumbar spine. Convulsive syndrome and cryptorchidism in boys can be diagnosed.
In newborn children, there is a lack of reflexes, intoxication with metabolic products occurs as a result of the fact that the organs do not perform their functions fully.
If the hypoplasia is bilateral, life expectancy can range from several days to several months. The indicator depends on the degree of developed renal failure.
Causes of enamel hypoplasia
There are several groups of causes of enamel hypoplasia. Depending on the period of their exposure, temporary or permanent teeth are affected.
Enamel hypoplasia of primary teeth
In the occurrence of enamel hypoplasia of primary teeth, the key etiological factors are:
- Causes of prenatal hypoplasia (the main period of exposure to a negative factor is pregnancy):
- Maternal diseases: hormonal disorders, epilepsy, rubella, toxoplasmosis, alcoholism;
- Physical factors (irradiation);
- Insufficient intake of vitamins, micro- and macroelements from food.
- The causes of neonatal hypoplasia (in the neonatal period - the first 56 days of a child’s life) can be prematurity, birth trauma, asphyxia, hemolytic disease of the newborn.
Enamel hypoplasia of permanent teeth
Hypoplasia of the enamel of permanent teeth is most often associated with diseases of the child that disrupt the metabolism in the body.
These are diseases:
1) Central nervous system: the mineral metabolism of phosphorus and calcium is disrupted, the amount of magnesium and potassium in the blood and bones decreases;
2) Endocrine system:
- Hyperthyroidism promotes the supply of calcium and phosphorus to the teeth and bones. With hypothyroidism, these elements are washed out.
- Against the background of insufficiency of the parathyroid glands, the content of calcium and phosphorus in the blood increases, decreases in the bones, nails, hair, and the lens are also affected;
3) Toxic dyspepsia and other diseases of the digestive system (due to insufficient absorption of calcium and phosphorus);
4) Hypovitaminosis C, D, E (up to rickets);
5) Acute infectious diseases;
6) Allergic diseases;
7) Insufficient nutrition.
Also, the quality of the enamel of permanent teeth depends on the condition of their temporary predecessors. Chronic apical periodontitis, mechanical trauma and removal of primary teeth with trauma to the follicle of a permanent tooth can lead to its hypoplasia.
Who to contact and diagnostic methods
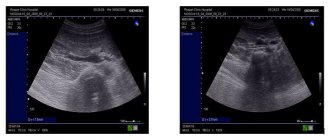
Treatment and diagnosis are carried out by pediatricians and general practitioners, nephrologists, and urologists. Patients undergo general and biochemical blood tests, and a general urine test. The following instrumental examinations are prescribed:
- ultrasound examination of the kidneys and the entire abdominal cavity;
- radiography of organs;
- computed and magnetic resonance imaging;
- Urography and angiography are also performed, showing the excretory function of organs and the state of blood circulation in them.
These techniques help to carry out differential diagnosis, which is carried out with dysplasia and a wrinkled kidney.
Methods of therapy
Treatment of kidney hypoplasia is complex, determined and corrected only by a doctor. There are no methods for complete recovery; therapy is usually symptomatic.
Traditional remedies
The prescription of any medications depends on the characteristics of the pathology. If patients are diagnosed with arterial hypertension, the selection of therapy is carried out in accordance with the standards.
The antihypertensive treatment regimen is individual, established and adjusted by the doctor. Commonly used drugs:
- groups of ACE inhibitors (enalapril, perindopril, lisinopril);
- beta blockers (bisoprolol, nebivalol);
- sartans (losartan, valsartan);
- diuretics (indapafone, spironolactone).
It is important to note that antihypertensive therapy is rarely successful, and patients usually require kidney removal to normalize blood pressure.
If patients are diagnosed with pyelonephritis, they are prescribed antibacterial therapy using drugs from the fluoroquinolone group. Often such patients are also indicated for nephrectomy.
Preparations with a high content of vitamin D and uroseptics are useful. Patients should also adhere to recommendations for dietary correction - the amount of salt, liquid and protein should be limited.
You should eat easily digestible foods, cooked or steamed. Fatty, fried, canned foods, and carbonated drinks are prohibited. You can drink clean water and fruit drinks.
In what cases is surgery necessary?
In addition to resistant arterial hypertension and bilateral lesions, surgery may be necessary for organ dystopia. Patients undergo removal of one or two kidneys. It is carried out through abdominal or laparoscopic nephrectomy. Tactics are selected individually.
Traditional methods
Traditional therapy methods are based on the use of herbs. Herbal medicine is carried out in conjunction with traditional medicine; before doing this, you should consult a doctor.
Herbal infusions from juniper, parsley, bearberry, horsetail, chamomile, calendula, mint, St. John's wort, and marshmallow are useful.
These plants help cleanse the body of toxic metabolic products and have an antiseptic effect on the organs of the urinary tract.
They can be brewed either separately or in various combinations. Drink decoctions 3-4 times a day half an hour before meals.
Treatment of children
Treatment of pediatric patients is in many ways similar to treatment of adults. A significant difference lies in cases where bilateral kidney damage is diagnosed.
In such situations, it is necessary to remove the affected organs, otherwise life expectancy will be short.
Patients after double nephrectomy require a transplant. Before transplantation, they need to attend hemodialysis sessions to cleanse the body of toxic substances.
If one kidney is affected and the functions of the second are at a satisfactory level, patients do not need surgery; it is enough to constantly visit the doctor and follow all lifestyle recommendations.
If the affected organ does not function well, it should be removed.
Nutrition and lifestyle tactics for children are the same as for adults. You can periodically take uroseptic drugs of plant origin.
Results and discussion
When analyzing case histories and protocols of pathological studies, the presence of concomitant malformations of various organs and systems was established in 43.6% of patients.
The results of the analysis of the distribution of developmental defects according to the principle from the cranial to the caudal end of the body are presented in the table.
The largest number of concomitant defects in these children were identified in the pelvic area, mainly in the organs of the urinary system.
Most often, renal hypoplasia was combined with dystopia, renal duplication and megaureter. A large number of concomitant defects were also identified in the chest area. There were relatively few defects in the abdominal cavity (see table).
The development of most of the identified defects is based on hypoplastic processes. These data indicate a significant disruption of the normal processes of intrauterine development, which are characterized by a delay or stop in the stages of organ maturation. It should be noted that pulmonary hypoplasia, detected in every fourth child with GP, and foot defects are pathogenetically related to the primary defect - GP and develop in connection with oligohydramnios, which indicates a significant decrease in kidney function even in the prenatal period.
Among the deceased children with HP, the majority were children from 0 to 1 month (74; 76.3%), 60 of them with severe bilateral kidney damage, 7 (7.2%) children died at the age of 1 month to 1 year. Then the number of deaths sharply decreases; 5 (5.1%) children died between the ages of 1 and 3 years, and 1 (1.0%) child died between 3 and 7 years. Due to decompensation of the underlying disease, 10 (10.3%) patients died between the ages of 7 and 15 years.
Renal failure was the cause of death in more than half of the deceased (54.8%). In the neonatal period, in 19.2% of cases, death occurred from pulmonary heart failure due to severe pulmonary hypoplasia. Infectious diseases were the cause of death in 29.6%, including sepsis in 13.4% of cases (of which 1.9% were urosepsis). During histological examination, oligonephronic hypoplasia or hypoplasia with dysplasia predominated in the kidneys. Simple hypoplasia was rare in the deceased, usually in combination with severe malformations of other organs and systems.
Complications
The disease may become more complicated. The most commonly diagnosed conditions are:
- dystopia, or organ displacement;
- narrowing of the ureters;
- violation of the structural components of the kidneys - pelvis, cups;
- stone formation;
- arterial hypertension;
- infectious diseases;
- renal failure of varying severity.
Some of the complications are common, so it is important to identify the disease as early as possible, which will help avoid unwanted conditions.
Prognosis and prevention
If there is bilateral damage, the prognosis of the disease is unfavorable. In rare cases, patients live longer than 1 year. In the situation of unilateral hypoplasia, the prognosis is more favorable. If a healthy kidney is able to perform its functions in full, the patient’s life expectancy is average.
It is important for patients to avoid hypothermia, physical overload, lead a healthy lifestyle, and follow advice on nutrition and water-salt regime. Only in this case can one hope for a full and long life.
Kidney hypoplasia is a disease that requires early diagnosis and timely treatment and prevention. Only following all the doctor’s recommendations and regular medical supervision can ensure the patient a full and long life.
Classifications of enamel hypoplasia
The most common classification of enamel hypoplasia is the classification of M.I. Groshikov. It is based on different etiologies and the number of teeth affected. Based on this, methods of treatment and prevention of various forms of hypoplasia differ.
Systemic enamel hypoplasia
Systemic enamel hypoplasia is a disorder in the structure of all teeth, but more often in groups associated with close periods of formation and eruption.
Such diseases in the ICD-C (1995) as prenatal enamel hypoplasia, neonatal enamel hypoplasia, enamel hypoplasia, non-endemic mottling are nothing more than “systemic enamel hypoplasia” according to M.I. Groshikov.
Features of the clinical manifestation of defects in systemic enamel hypoplasia:
- appearance from the moment of eruption;
- symmetrical, of the same size on teeth of the same name;
- localized parallel to the chewing surface or cutting edge, most often on the tubercles or vestibular surface.
There is also a relationship between the defect and the action of the damaging factor:
- The type of defect (qualitative or quantitative change in enamel) depends on the intensity of the factor;
- Localization of the defect - depending on the time of its exposure;
- The width of the defect depends on the duration;
- The number of defects indicates the frequency of action of the damaging factor.