How is acetone formed in the body?
When carbohydrates enter the body, they are broken down into glucose and absorbed into the blood in the intestines. One part of the organic compounds is absorbed by cells with the release of energy, and the second is transformed into glycogen and accumulates in the liver tissue. With serious energy consumption - stress, exhausting physical work - glycogen again enters the bloodstream.
In most people, the liver has a high storage capacity, so energy reserves do not run out for a long time. But in 17-20% of young children, the liver tissue accumulates only a small amount of glycogen. And if it is exhausted, lipids (fats) begin to be used as an energy resource. When they are broken down, acetone or ketone bodies appear. If metabolic products are not removed from the blood for a long time, the child’s well-being worsens.
Acetone irritates the vomiting receptors, causing uncontrollable vomiting. Dehydration only aggravates the carbohydrate deficiency, as a result of which the concentration of acetone in the body increases.
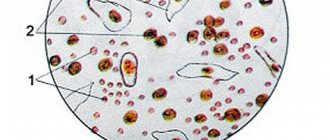
Norm of acetone in urine
Ketone bodies are metabolic products that are secreted by the liver tissue. They are involved in metabolism and the release of energy from lipids. These include:
- beta-hydroxybutyric acid;
- acetone;
- acetoacetic acid.
Acetone is a product of the breakdown of fat cells.
It is formed in the blood in very small quantities. Therefore, during a general urinalysis (UCA), only traces of acetone are detected. Its level in daily urine does not exceed 0.01-0.03 g.
What does ketone content in urine mean?
An increase in acetone content compared to the norm is called acetonuria or ketonuria. Particularly characteristic of acetonuria is the excretion of ketone bodies in the urine, these include acetoacetic acid, hydroxybutyric acid and acetone itself.
From a practical point of view, each indicator is not analyzed separately, but such a generally accepted concept as “acetone” is used. It is formed through insufficient oxidation of proteins and fats by the human body, and in high concentrations it is toxic.
Exceeding the rate of ketone formation before their oxidation and elimination is fraught with such consequences as:
- dehydration;
- damage to the gastrointestinal mucosa;
- increased blood acidity;
- damage to brain cells up to swelling;
- cardiovascular failure;
- ketoacidotic coma.
Why does a child's ketone levels increase?
If acetone is detected in a child’s body, this means that the metabolism of amino acids or lipids is impaired. Due to functional immaturity, the gastrointestinal tract malfunctions. With poor nutrition, 5% of children develop metabolic disorders. If a child’s body lacks carbohydrates, lipid metabolism is activated. When fats are broken down, a lot of acetone is formed, which leads to poisoning.
The main reasons for the increase in acetone:
- insufficient intake of glucose from food;
- the predominance of lipids in the diet;
- impaired absorption of carbohydrates in the intestine;
- underfeeding in infants;
- following a strict diet;
- bacterial or inflammatory damage to the gastrointestinal tract;
- dehydration.
An increase in the level of acetone in the urine is accompanied by a violation of water-electrolyte balance and a pathological effect on the gastrointestinal tract and nervous system of the child.
Changes in ketone levels are sometimes a manifestation of disease:
- gastroenteritis;
- hemolytic anemia;
- brain tumors;
- thyrotoxicosis;
- infectious toxicosis;
- Itsenko-Cushing's disease;
- decompensated diabetes mellitus;
- hepatocellular carcinoma;
- blood cancer (leukemia).
Factors that provoke acetonuria include:
- excessive psycho-emotional stress;
- frequent relapses of ARVI;
- neuroinfections;
- binge eating;
- vitamin and mineral deficiency;
- abuse of meat food.
An increased level of acetone in the body of newborns in 80% of cases is associated with late toxicosis in the mother.
The risk group includes children with neuro-arthritic diathesis, as they are susceptible to rapid depletion of the nervous system and glycogen reserves in the liver.
Why does acetone appear in diabetes mellitus?
In order to fully understand the development of this disease, it is necessary to understand the occurrence of the disease. First of all, you need to include three substances such as:
- acetoacetate,
- beta-hydroxybutyric acid,
- propanone
All these substances are products of the breakdown of not only endogenous fats, but also proteins. The reasons for their appearance in the human body are:
- low carb diet,
- presence of symptoms such as vomiting or diarrhea for a long time,
- starvation,
- chemical poisoning,
- suffered a severe infectious disease,
- dehydration,
- overheating.
Also one of the reasons may be decompensation of diabetes. If we talk about disorders of blood sugar levels, the problem of the presence of acetone in the urine can arise under two different conditions:
- Hyperglycemia. In this case, due to the insufficient amount of insulin consumed by the body, excess sugar is not absorbed by brain cells. For this reason, they begin to break down and form ketone bodies. When they increase significantly, the liver cannot cope with their utilization, and they end up in the urine.
- Hypoglycemia. In this case, its occurrence is provoked due to the production of a large amount of the hormone or a lack of glucose in food. The reason may be the lack of a substrate, which is necessary to produce energy at the required rate, for the production of which the body uses other substances.
Acetone itself does not pose a serious threat to life in case of diabetes. It simply indicates that the body does not have enough insulin in the required dose. Of course, this cannot be considered the norm either. It is imperative to monitor your glycemic level and undergo mandatory examination by an endocrinologist. Do not forget that against the background of this symptom, ketoacidosis may develop. It causes dizziness, general weakness, and pale skin. All this indicates acidification of the body, which in turn requires normal and correct therapy.
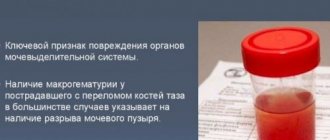
Signs of elevated acetone
An increased amount of acetone in the blood serum is found in 20% of children of the younger age group. Metabolic disorders are indicated by signs of intoxication and a characteristic odor emanating from the mouth.
How to determine acetonuria in a child:
- vomiting for more than 2-3 days;
- pale skin;
- muscle weakness;
- elevated temperature;
- low urine output;
- nervous excitement;
- cutting pain in the abdomen;
- diarrhea or constipation;
- decreased appetite;
- white coating on the tongue;
- sleep disturbance;
- irritability.
An increased content of acetone in the systemic bloodstream leads to poisoning and deterioration of the child’s well-being. Irritability, muscle cramps, and fever appear.
An increase in the level of acetone bodies is accompanied by intoxication. As a result, the functioning of the central nervous system is disrupted and the vomiting centers are irritated. Therefore, the child has no appetite and does not stop vomiting.
Symptoms of the disease
This pathology occurs in type I diabetes mellitus, but can also occur in type II diabetes. Therefore, at the first signs of illness, immediately consult a doctor to prescribe treatment.
Symptoms include:
- Abdominal pain.
- Vomit.
- Cardiopalmus.
- Acetone smell on your breath (or other unusual odor).
- Dehydration of the body (dehydration).
- Disorientation in space, confusion.
- Unconsciousness (or coma).
Ketone bodies are found in urine.
Why are high levels of ketones in urine dangerous?
The accumulation of acetone in the body is fraught with acetone syndrome, which manifests itself:
- lacrimation;
- feverish condition;
- tachycardia;
- persistent vomiting;
- severe dehydration;
- sleep disturbance;
- neurological disorders;
- arrhythmia.
If the problem is ignored, the liver increases in size (hepatomegaly). Patients with severe acetone syndrome exhibit meningeal symptoms - involuntary flexion of the limbs, tension in the neck muscles.
What tests reveal an increase in acetone in children?
Ketone bodies are determined by the results of a general urine test. The doctor prescribes tests when a child detects characteristic symptoms of acetonuria - a specific odor from the mouth, constant vomiting, decreased urine output, pale skin.
Laboratory research
Acetone in a child is determined according to OAM data. The key purpose of the test is to detect the amount of ketone antibodies in urine. To eliminate errors in the results, preparations for diagnosis are made 2 days before the biomaterial is submitted to the laboratory.
Preparation for OAM:
- 2 days before the study, exclude fatty and coloring foods from the diet;
- refuse hormonal medications and dietary supplements;
- Avoid psycho-emotional stress and physical exertion.
When collecting urine, the following rules must be taken into account:
- Only morning urine collected after waking up is used as a biomaterial;
- before collecting biomaterial, the genitals are washed with neutral soap;
- the first portion of urine (40 ml) is passed, and the middle portion (60-100 ml) is collected in a plastic container.
The container for collecting biomaterial should not touch the skin.
The collected liquid is transferred to the laboratory within 1-2 hours after collection.
To determine the cause of acetonuria, additional studies are prescribed:
- clinical blood test;
- blood test for glucose;
- Ultrasound of the urinary system;
- CT scan of the brain.
Based on the diagnostic results, the doctor distinguishes the disease from meningitis, intestinal infections, and cerebral edema.
Home test for acetonuria
To check the acetone content in a child’s body, it is enough to purchase a test strip at the pharmacy. It is impregnated with a reagent that changes color upon contact with ketone bodies. The degree of acetonuria is determined according to the scale:
- up to 0.5 mmol/l – absent;
- 5 mmol/l – mild;
- no more than 4.0 mmol/l – average;
- 10 mmol/l – severe.
If there is a lot of acetone, you need to make an appointment with your pediatrician. Doctors advise using indicator strips at home to monitor the effectiveness of treatment.
Preparing for urine tests
General rules:
- ATTENTION! On the eve of the study, consumables (container with adapter and test tube) must be obtained in advance from any laboratory department
- 10-12 hours before the test it is not recommended to consume: alcohol, spicy and salty foods, as well as foods that change the color of urine (beets, carrots)
- If possible, avoid taking diuretics
- After cystoscopy, a urine test can be prescribed no earlier than 5-7 days later.
- Women are not recommended to take a urine test during menstruation
- The patient collects urine independently (with the exception of children and seriously ill patients)
- Before taking the test, perform a thorough toileting of the external genitalia:
- in women, use a cotton swab moistened with warm soapy water to clean the external genitalia (treating the labia by moving the swab in front and downwards); dried with a clean cloth, previously ironed with a hot iron.
- in men - the external opening of the urethra is toileted with warm water and soap, then washed with warm water and dried with a clean napkin, previously ironed with a hot iron.
General urine analysis
- For general analysis, use the first morning portion of urine (the previous urination should be no later than 2 am)
- Before collecting urine, perform a thorough toilet of the external genitalia. For men, when urinating, completely pull back the skin fold and release the external opening of the urethra. For women, spread the labia. Unscrew the lid of the container and place it with the urine transfer device facing up
- Attention! Do not touch the sterile straw or the inside of the cap with your hands.
- Flush the first small amount of urine into the toilet, and then collect the middle amount of urine in a container
- The container should be filled no more than ¾ of its volume. Minimum - 30 ml, maximum - 80 ml
- Screw the lid on tightly, carefully holding the edges. Stir the contents of the container 3-5 times, carefully turning it 180°
- Label the tubes with patient information. Enter Last Name I.O. Attention! Block letters
- Carefully peel back the sticker on the tube cap, but do not tear it off completely!
- Place the test tube, cap down, into the recess on the container lid. Press down on the bottom of the tube and push the cap through. After filling the test tube with urine, remove it from the container
- Mix the contents of the test tube 8-10 times, carefully turning it 180°. Deliver the test tube with urine to the laboratory department on the day of taking the biomaterial
24-hour urine collection
Collect urine for 24 hours using normal drinking regimen (1.5 - 2 liters per day):
- At 6-8 o'clock in the morning, empty the bladder (pour out this portion of urine)
- Within 24 hours, collect urine in a clean container with a capacity of at least 2 liters. During collection, the container with urine must be stored in a cool place (optimally in the refrigerator on the bottom shelf at +4° +8°C), preventing it from freezing
- Collect the last portion of urine at exactly the same time the next day when collection began the day before.
- Measure the amount of urine and pour 50-100 ml into a special sterile container. Be sure to write on the container the volume of urine collected per day (daily diuresis)
Urinalysis according to Nechiporenko
Collect urine in the morning (immediately after sleep) using the 3-glass sample method: start urinating in the toilet, collect the middle portion in a special sterile container, finish in the toilet
The second portion of urine should prevail in volume. Deliver a medium portion of urine to the laboratory in a urine tube. Report the time of urine collection to the registrar. It is allowed to store urine in the refrigerator (at t +2° +4°), but not more than 1.5 hours.
Urine analysis according to Zimnitsky
Urine for research is collected throughout the day (24 hours), including at night.
- 1 serving: from 6-00 to 9-00 am
- 2 servings: from 9-00 to 12-00
- 3 serving: from 12-00 to 15-00
- 4 servings: from 15-00 to 18-00
- 5th portion: from 18-00 to 21-00
- 6th portion: from 21-00 to 24-00
- 7th portion: from 24-00 to 3-00
- 8 portion: from 3-00 to 6-00
In the morning at 6-00 (on the first day of collection), you should empty your bladder, and this first morning portion of urine is not collected for research, but poured out.
In the future, during the day it is necessary to consistently collect 8 portions of urine. During each of eight 3-hour periods of time, the patient urinates one or more times (depending on the frequency of urination) into a container with a volume of at least 1 liter. The volume of urine in each of the 8 portions is measured and recorded. Each portion of urine is mixed and 30-60 ml is taken into a separate special sterile container. If the patient has no urge to urinate within three hours, the container is left empty. Urine collection is completed at 6 a.m. the next day. All 8 containers are delivered to the laboratory, on each of which it is necessary to indicate the portion number, the volume of urine excreted and the time interval for urine collection.
Report the amount of liquid you drink per day to the receptionist.
Functional tests
- Rehberg test (blood creatinine, 24-hour urine creatinine) Before performing the test, it is necessary to avoid physical activity, exclude strong tea, coffee, and alcohol. Urine is collected throughout the day: the first morning portion of urine is poured into the toilet, all subsequent portions of urine excreted during the day, night and the morning portion of the next day are collected in one container, which is stored in the refrigerator (t +4° +8° C) in during the entire collection period (this is a necessary condition). After completing urine collection, measure the contents of the container, be sure to mix it and immediately pour it into a special container, which must be delivered to the laboratory. Report the volume of daily urine to the treatment nurse. After this, blood is taken from a vein to determine creatinine.
Biochemistry of urine
When preparing for a biochemical urine test, pay attention to what kind of urine needs to be collected (one-time or daily) for each type of analysis.
- Collection of urine for determination of oxalates. Only single urine is used as material for the study.
- Sulkowicz test (urine calcium, qualitative test) Immediately after sleep on an empty stomach, collect the entire morning portion of urine in a dry, clean container
- Mix all collected urine. Pour 40-50 milliliters of the total volume of urine into a special sterile container and close the lid tightly. You cannot take urine from a vessel or potty.
- Urine in a container is delivered to the laboratory
Urine tests for hormones
- Urinalysis for catecholamines, namely: Adrenaline + Norepinephrine
- Adrenaline+Norepinephrine+Dopamine
- Comprehensive study of catecholamines, serotonin and their metabolites
- Urine analysis for the content of intermediate metabolites of catecholamines: metanephrine, normetanephrine
IMPORTANT ! To study 24-hour urine, a preservative is required - 15 g of citric acid (the powder must be obtained on the eve of the study in the Laboratory office along with a container for urine). Before routine urine collection to determine catecholamines, preparations containing rauwolfia, theophylline, nitroglycerin, caffeine, and ethanol should not be used for 3 days. If possible, do not take other medications, as well as foods containing serotonin (chocolate, cheeses and other dairy products, bananas), and do not drink alcohol. Avoid physical activity, stress, smoking, pain, which causes a physiological rise in catecholamines. First, a preservative - powder (citric acid) obtained in the laboratory - is poured into the bottom of a clean large container into which urine will be collected. The first portion of urine is poured into the toilet, the time is noted and the urine is collected in a container with a preservative exactly during the day, the last urination into the container should be 24 hours from the time recorded (for example, from 8.00 am to 8.00 am the next day). As an exception, you can collect urine for 12, 6, 3 hours, or use a single portion of urine collected during the daytime for analysis. At the end of the collection period, measure the total volume of urine excreted per day, mix it, pour some into a specially provided container and immediately bring it for examination. When submitting the material, be sure to note the time of collection and the total volume of urine.
- Determination of DPID in urine Collect urine before 10 am. Collect and deliver the 1st or 2nd morning urine sample to the laboratory
Collection of urine for microbiological studies
- Urine culture (with determination of sensitivity to antibiotics) Urine collection must be carried out before the start of drug treatment and no earlier than 10-14 days after the course of treatment. Collect urine in a special sterile container: DRAIN THE FIRST 15 ml OF URINE INTO THE TOILET. Collect the next 3-10 ml in a special sterile container and screw the lid on tightly. Deliver the biomaterial to the laboratory within 1.5-2 hours after collection. It is allowed to store the biomaterial in the refrigerator (at t +2° +4° C) for no more than 3-4 hours. If delivered to the laboratory later than the specified time, the results of urine culture may be unreliable.
Urine collection for determination of UBC (bladder cancer antigen)
It is recommended to collect a morning urine sample. An arbitrary portion of urine that has been in the bladder for 3 hours or more is subject to examination. The biomaterial is delivered to the laboratory within 3 hours after collection in a special container.
2 glass sample:
- For the study, a full portion of urine is collected, which has been in the bladder for at least 4-5 hours; it is preferable to collect the first morning urine
- The patient begins urinating into the first container and finishes into the second, it is important that the second portion of urine is larger in volume
- Attention! Do not touch the sterile straw or the inside of the cap with your hands.
- Each container should be filled to no more than ¾ of its capacity. Minimum - 30 ml, maximum - 80 ml
- Screw the lid on tightly, carefully holding the edges. Stir the contents of the container 3-5 times, carefully turning it 180°
- Label the tubes with patient information. Enter Last Name I.O. Attention! Block letters
- Carefully peel back the sticker on the tube cap, but do not tear it off completely!
- Place the test tube, cap down, into the recess on the container lid. Press down on the bottom of the tube and push the cap through. After filling the test tube with urine, remove it from the container
- Mix the contents of the test tube 8-10 times, carefully turning it 180°
- Both tubes of urine are delivered to the laboratory, and the portion number must be indicated on each tube. Storage in the refrigerator is allowed (+2…+4), but no more than 1.5 hours
3 glass sample:
- For the study, a full portion of urine is collected, which has been in the bladder for at least 4-5 hours; it is preferable to collect the first morning urine.
- The patient begins to urinate into the first container, continues into the second and finishes into the third, it is important that the second portion of urine is larger in volume (about 80% of all urine).
- Attention! Do not touch the sterile straw or the inside of the cap with your hands.
- Each container should be filled to no more than ¾ of its capacity. Minimum - 30 ml, maximum - 80 ml.
- Screw the lid on tightly, carefully holding the edges. Stir the contents of the container 3-5 times, carefully turning it 180°
- Label the tubes with patient information. Enter Last Name I.O. Attention! Block letters
- Carefully peel back the sticker on the tube cap, but do not tear it off completely!
- Place the test tube, cap down, into the recess on the container lid. Press down on the bottom of the tube and push the cap through. After filling the tube with urine, remove it from the container.
- Mix the contents of the test tube 8-10 times, carefully turning it 180°
- All three tubes of urine are delivered to the laboratory, and the portion number must be indicated on each tube. Storage in the refrigerator is allowed (+2…+4), but no more than 1.5 hours.
Cytological examination of urine:
- It is necessary to collect urine after morning urination
- Urine collected during morning urination is not used for this study. Cells left overnight in the bladder may be destroyed
- Mix all collected urine. Pour 40-50 ml into a special sterile container and deliver to the laboratory department
How to reduce ketone levels
For moderate acetonuria, hospitalization is not required. The treatment regimen is determined by the doctor taking into account the OAM data. The main goals of treatment include:
- reducing the amount of acetone in the body;
- restoration of carbohydrate and lipid metabolism;
- normalization of liver functions.
To prevent acetone syndrome, diet, drug therapy and physiotherapy are prescribed.
Colon lavage
To cure a child, it is necessary to reduce the acetone content in the body. Indications for the use of cleansing enemas are:
- vomit;
- loose stools;
- weakness;
- lack of appetite;
- elevated temperature.
Features of performing an enema:
- sodium bicarbonate solution is used as a washing liquid;
- before administration, the tip of the enema or bulb is lubricated with Vaseline;
- the rubber tip is inserted into the anus to a depth of 3.5-5 cm;
- 150-500 ml of liquid is injected into the rectum (the volume depends on the age of the child);
- Without opening the enema, the tip is carefully removed from the anus.
The procedure is performed once a day, but only on the recommendation of a pediatrician.
Frequent drinking
Treatment of acetone in children at home requires compliance with the drinking regime. To restore water and electrolyte balance and prevent dehydration, use the following as a drink:
- weak tea with honey or sugar;
- fruit compotes;
- herbal decoctions.
If the child is vomiting, they give powders with electrolytes and carbohydrates - Regidron, Gidrovit, Orsol, Electral. To restore liver function, it is recommended to give your baby alkaline mineral water.
Diet
Diet therapy is one of the most effective methods of preventing acetone syndrome in a child. To compensate for the lack of glucose, easily digestible carbohydrates are introduced into the diet:
- berries;
- milk;
- yogurt;
- dried fruits;
- vegetables;
- muesli;
- honey;
- watermelon;
- cottage cheese;
- fresh fruits;
- pancakes.
The consumption of foods with protein components, lipids and amino acids is limited. During treatment the following are excluded from the menu:
- fish;
- meat broths;
- smoked meats;
- fast food;
- offal;
- fat meat.
If a baby has acetonuria, it is necessary to increase the frequency of breastfeeding. If the baby is bottle-fed, use anti-reflux formulas with a high glucose content.
Medicines and enterosorbents
Drug therapy is aimed at eliminating intoxication and liver dysfunction. For acetonuria, the following groups of drugs are used:
- antiemetics (Domperidone, Cerucal) – eliminate nausea and vomiting;
- sedatives (Glycine, Atomoxetine) – have a calming effect on the nervous system, reducing anxiety and irritability;
- antispasmodics (Drospa forte, No-shpa) - relieve cramping pain in the abdomen.
Children with severe intoxication are prescribed infusion therapy. It involves intravenous administration of saline preparations and glucose.
To improve the condition of the liver, herbal hepatoprotectors are used - Hofitol, Artichol, Holosas, etc. For symptoms of hypovitaminosis, multivitamin products are recommended - Multivit, Supradin Kids, Vitrum, Pikovit, Aevit. To quickly remove toxins, sorbents are used - Polysorb Polyphepan, Filtrum, Enterosgel. Drinking alkaline water speeds up the elimination of toxins in the urine.
When is a 24-hour urine test prescribed?
A 24-hour urine test is prescribed primarily to check the functioning of the kidneys, as well as to monitor substances excreted from the body in the urine during the day.
Indications for prescribing a 24-hour urine test are:
- suspicion of certain kidney diseases;
- diabetes. The test is used to monitor daily urine glucose levels;
- pregnancy. The test is used to assess how well the expectant mother's kidneys cope with increased stress.
Until what age can acetone levels increase?
An excess of acetone in the blood serum occurs in 17-20% of young children. According to statistics, acetonuria first appears at 2-3 years of age. In children 6-7 years old, the concentration of ketone bodies increases sharply, which is associated with changes in the functioning of the gastrointestinal tract.
By puberty - 11-13 years - signs of acetonuria disappear in most children. If the level of acetone increases slightly, this indicates a metabolic disorder due to poor nutrition.
Fluctuations in the amount of ketones in infants in 90% of cases are due to insufficient nutrition.
Main causes of the disease
The mechanism of development of the disease is the breakdown of proteins and fats with the formation of ketone bodies and their accumulation in the blood of children. Subsequently, the blood is filtered by the kidneys and ketonuria develops. The condition is extremely dangerous for the child, since ketones have a negative effect on the body’s cells, including brain cells, leading to the development of metabolic acidosis, due to which the child can fall into a coma and die.
Parents often wonder why their baby's acetone levels have increased. This condition has different causes, but one of the most common is a decrease in blood glucose concentration, which occurs due to metabolic disorders.
- In particular, glucose concentration may decrease due to prolonged fasting, when the body does not receive enough nutrients.
- Diabetes mellitus is also one of the most common causes of the appearance of ketones in the urine in children, because with this disease, the absorption of glucose is impaired, since the body lacks insulin.
- Another reason for the appearance of ketone bodies in the urine of children may be an unbalanced diet (excessive consumption of proteins and fats), which disrupts the digestive processes.
- There is another serious disease that can provoke an increase in acetone levels in children. This is a hereditary (or acquired) enzymatic deficiency, due to which the body is unable to properly digest carbohydrates. Factors provoking the pathological condition may include reasons such as:
- fear and severe nervous overload;
- physical overload;
- mental stress;
- unhealthy diet;
- and excessive exposure of children to the sun (heatstroke).
- An increase in the level of acetone in a baby’s urine can also be caused by diseases of an infectious nature, elevated body temperature, or exacerbation of chronic diseases.
- Sometimes an increased amount of the substance is observed in the postoperative period, with various injuries and damage, poisoning.
- Another reason for this phenomenon may be the presence of cancer or mental illness.
Prevention
To prevent an increase in the amount of acetone in the urine in children, you should:
- balance the diet;
- do not feed your baby fast food;
- sign up for moderate exercise sports or dancing;
- observe drinking regime;
- walk in the fresh air more often;
- promptly treat metabolic diseases (obesity, diabetes).
Children with acetone syndrome need to undergo a course of vitamin therapy twice a year, take hepatoprotectors and sedatives. It is recommended to periodically determine the level of ketone bodies with a test strip. A child with diabetes should be registered with an endocrinologist. Timely detection and treatment of diseases prevents dangerous complications.
Folk remedies for acetone
Surely every person suffering from a sugar disease is interested in how to remove acetone in urine in diabetes . There are many different methods, but the most effective and frequently used among patients are: garlic, walnut leaves, sauerkraut.
The most popular method is taking a product such as garlic. A healing drink is prepared on its basis. To do this, several heads of the product are cleaned and crushed in a garlic press. The finished raw materials are poured with boiling water. This tea should steep for 15 minutes, after which it is taken a quarter glass three times a day.
No less popular is a medicine made from walnut leaves. To prepare, take fresh leaves, wash them well and pour a glass of boiling water. The drink should be allowed to brew for 10-20 minutes, after which it should be strained and taken half a glass twice a day.
If you are looking for the easiest method to remove acetone from the body with diabetes , then you should pay attention to sauerkraut. Not only does it help to quickly get rid of this problem, but it also has no restrictions on use. But you can eat it in large quantities for no more than two months. If the cause of the problem is “hungry acetone,” which appears due to the exclusion of carbohydrates from the patient’s diet, then you need to eat jam, honey and even sweets in small quantities. At the same time, be sure to adjust your diet. It would be a good idea to pay attention to playing sports. If you do not have the opportunity to exercise in a specialized gym, then daily exercise is a good option. Pay more attention to walks in the fresh air. Only an integrated approach will help get rid of the problem in a short period of time. It is important that before to remove acetone for diabetes, be sure to go to your doctor for consultation.
Source