Traces of hemoglobin in the urine of adult men, women, and children of all age groups are the first sign of a pathological condition of blood vessels, dysfunctional disorders in the hematopoietic system, kidney disease and other organs of the excretory system.
The appearance of signs of hemoglobin in urine indicates intravascular hemolysis of red blood cells, as well as a gradual change in the cellular composition of the blood. This is a dangerous symptom that can occur due to the presence of hematological factors, as well as due to the negative influence of external factors.
How and under what conditions is it formed in urine?
Traces of hemoglobin in the urine of men, women and children should be completely absent. The appearance of this substance in urine is called hemoglobinuria. In the bloodstream of healthy people, on average, about 10% of all red blood cells are destroyed, which release free hemoglobin.
In this regard, the blood plasma contains about 4 mg% of this protein compound. Free hemoglobin actively interacts with haptoglobin, forming strong biochemical bonds. This compound is not able to overcome the kidney filter, since its molecular weight ranges from 160 to 320 kDa.
The molecular complex, consisting of free hemoglobin and haptoglobin, enters the tissues of the liver and spleen, where it undergoes chemical decomposition with the formation of final metabolites of pigment metabolism.
If in the human body these biochemical processes proceed stably, and the kidneys, liver and spleen perform their functions, then hemoglobin molecules do not penetrate into the urine, as they break down into their constituent substances inside the body. Hemoglobinuria develops only when a critical amount of free hemoglobin (over 100 mg%) enters the blood plasma.
Haptoglobin, which is found in the bloodstream, is not able to bind excess concentrations of free hemoglobin, which entails its active reabsorption by kidney cells.
Absorbed hemoglobin accumulates in the epithelial tissues of the proximal canals, and then, through the process of chemical oxidation, can be converted into the substances hemosiderin and ferritin. Part of the absorbed hemoglobin enters the urine, which is subsequently detected during laboratory testing for biochemical parameters.
Traces of hemoglobin in the urine of women, men and children appear after prolonged or short-term exposure to external factors, or are one of the symptoms of a painful condition of internal organs. The table below details conditions the presence of which can lead to the formation of free hemoglobin in urine.
| Factors influencing the appearance of traces of hemoglobin in urine | Description of pathological processes |
| Nocturnal hemolysis of red blood cells | In this case, hemoglobin enters urine exclusively at night, when a person is sleeping and the pH of his blood is at a lower level. This pathological condition of the body is caused by the presence of a hematological disease in the form of acquired anemia, a type of which is extremely rare in medical practice. Mass death of red blood cells occurs in attacks. In the shortest possible period of time, a large amount of free hemoglobin is released into the blood plasma. The tissues of the liver and spleen are not able to ensure the rapid binding and breakdown of this substance. Such hemoglobinuria most often occurs in men and women whose age ranges from 20 to 40 years. Nocturnal hemolysis of red blood cells is associated with heavy physical activity, chronic infection, intoxication of the body, and the consequences of prolonged use of iron-containing drugs. After eliminating the negative influence of external and internal factors, urinalysis indicators stabilize, and free hemoglobin ceases to saturate the blood plasma. |
| Severe intoxication of the body | Contact with chemical or biological substances, overdose of potent drugs that have toxic properties can lead to massive hemolysis of red blood cells. In this regard, a sharp change in the cellular composition of the blood occurs, the death of red blood cells with the release of free hemoglobin. This is a dangerous condition of the body that requires emergency treatment measures. |
| Continuous static load | Traces of hemoglobin in urine can periodically appear in absolutely healthy people who have been on their feet for a long time or have traveled long distances on foot. Similar symptoms are often found in soldiers practicing marching formation, travelers, and athletes who engage in race walking or marathon running. In this case, hemolysis of red blood cells is associated with a static effect on the plantar part of the foot, the consequences of which are damage to red blood cells with the release of excess amounts of free hemoglobin. Traces of protein compounds are not found in urine after a short rest and recovery of the body. |
| Negative effects of cold | After prolonged swimming in cold water or hypothermia due to being in the open air, paroxysmal hemoglobinuria develops. The amboceptor hemolysin is formed in human blood, which binds to red blood cells, causing their premature hemolysis. The danger of the pathological process lies in the fact that with severe hypothermia, changes in the cellular composition of the blood can be irreversible. Once normal body temperature is restored, signs of free hemoglobin in urine disappear in humans. On average, this occurs after 24-48 hours. |
| Autoimmune reaction | This reason for the appearance of traces of hemoglobin in urine is very rare. The conditions for the development of a pathological state of the body are due to the fact that the cells of the immune system regard red blood cells as foreign and extraneous agents. Red blood cells are constantly under attack, which ultimately leads to an increase in the level of free hemoglobin, the detection of traces of it in the urine and the development of severe anemia. |
| Blood transfusion | In the case of transfusion of donor blood, which has an incompatible antigenic structure, acute hemolysis of red blood cells develops with the release of large amounts of hemoglobin. The protein compound saturates the composition of urine, and the symptoms of hemoglobinuria persist for several days. |
| Diseases of infectious origin | Bacterial pathogens of diphtheria, typhoid fever, syphilis, scarlet fever cause the death of red blood cells and the appearance of an excess amount of free hemoglobin. As the patient recovers, the biochemical composition of urine stabilizes. |
| Pathologies of the genitourinary system | Acute inflammatory diseases of the tissues of the kidneys, bladder and urethra can lead to destruction of their structure and the appearance of ulcerative formations. Hemolysis of red blood cells is caused by local secretions of blood and the breakdown of its cells. After eliminating the underlying disease, traces of free hemoglobin in the urine disappear |
Regardless of the conditions under which hemoglobin molecules appear in urine, its presence indicates a diseased state of the body. A person with a similar symptom should undergo a comprehensive examination aimed at detecting pathology.
BLOOD IN URINEClinical aspects
In a healthy person, hemoglobin and red blood cells are not detected in the urine.
Blood in the urine can be detected by the presence of red blood cells (hematuria syndrome) or by the breakdown products of red blood cells (hemoglobinuria, siderinuria syndromes).
Hematuria.
Single red blood cells are found in the urine of even completely healthy people. In practically healthy people, up to 1 million red blood cells are released per day, which corresponds to the content of 1 red blood cell in 1 μl of urine.
Microhema guria
-
the color of urine is not changed, red blood cells are detected by microscopy of urine sediment using an indicative method (more than 5 red blood cells in the field of view) and more effectively - quantitative methods (more than 1000 red blood cells in 1 ml of urine or more than 1,000,000 red blood cells per day).
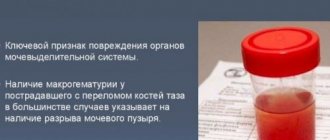
Gross hematuria
manifested by the color of urine; the color of urine, depending on the number of red blood cells, can be pink, reddish, red, or the color of “meat slop.” The boundary between micro- and macrohematuria is considered to be the presence of approximately 0.5 ml of blood in 1 liter of urine (about 2500 red blood cells in 1 µl of urine).
According to etiology, hematuria can be divided into the following groups:
1. Hematuria associated with kidney disease (unilateral and bilateral) - renal hematuria
2. Hematuria from the urinary tract - postrenal form
3. Hematuria with hemorrhagic diathesis (prerenal form)
With all these pathological processes, there can be both micro- and macro-hematuria. Renal hematuria can be functional, temporary, or organic.
Functional hematuria (usually micro-hematuria) is characteristic of early childhood. The cause of this hematuria is the failure of the renal filter, its increased permeability. The kidneys of an infant react to the slightest irritation: a blow, careless palpation of the lumbar and abdominal region. Functional hematuria in adults is observed during hypothermia and overheating, during heavy physical activity (sports, marching) and is usually combined with albuminuria. Functional hematuria includes orthostatic hematuria and hematuria with hyperlordosis (curvature of the spine) in adolescents, the leading symptom of which is transient orthostatic proteinuria and constant proteinuria with lordosis.
Temporary hematuria is observed with toxic infections (sepsis, influenza, scarlet fever, infectious mononucleosis, mumps, rubella, bronchopneumonia, tonsillitis, etc.) and, apparently, also has a functional nature.
Some drugs have a potential nephrotoxic effect (aminoglycoside antibiotics, analgesics, cyclosporine A, cytostatic drugs, methenamine, sulfonamides). The use of these drugs may lead to interstitial nephritis (non-infectious). In most cases, changes in the kidneys are reversible after stopping the medication. However, their prolonged use can lead to the development of chronic interstitial nephritis. An indicator of proximal tubular damage in this case is microhematuria and tubular proteinuria (<1.5 g protein/day).
Renal hematuria may be primarily associated with acute glomerulonephritis in cases where the glomeruli are damaged to such an extent that they allow cellular elements of the blood to pass through. In acute glomerulonephritis, hematuria is the main symptom in the first days of the disease. Diffuse damage to the glomeruli (glomeruli) is accompanied by macrohematuria, focal - microhematuria, proteinuria and hypertension. During the recovery period, red blood cells disappear faster than other symptoms normalize. “Residual hematuria” in acute glomerulonephritis is a direct sign of persistent glomerulonephritis. Chronic nephritis and nephrosis are accompanied by moderate hematuria. Hematuria can be caused by circulatory disorders leading to secondary renal failure (renal vein thrombosis, venostasis due to heart failure or trauma, kidney stones, kidney or urinary tract tumors).
According to various estimates, stones in the kidneys and bladder are present in 1-3% of the adult population, that is, we can talk about an etiological disease. The most common stones are oxalate (55%), urate (25%) and phosphate (20%). Often the presence of urinary stones is combined with an increased level of uric acid in the urine. With urolithiasis, renal hematuria is observed in approximately 20% of cases and, as a rule, is combined with leukocyturia. Microhematuria is the first symptom of urolithiasis, manifested against the background of pain in the lumbar region, and is the main test for the early diagnosis of urolithiasis.
Hematuria is observed in a third of patients with pyelonephritis. Pyelonephritis is diagnosed clinically in 5-8% of women and elderly men. Typically, a diagnostic examination includes the determination of bacteriuria and leukocyturia.
Hematuria should always be considered as an indication of a possible tumor of the kidney, urinary tract or bladder. A kidney tumor may present with painful hematuria long before a definitive diagnosis of malignancy is made. Therefore, if hematuria of unknown etiology is detected, it is necessary to exclude a tumor process.
Hematuria, not associated with organic damage to the renal parenchyma, complicates congenital and acquired coagulopathies (thrombocytopenia or thrombocytopathy, Werlhoff disease, Rendu-Osler disease, hemophilia, defects in coagulation factors, severe liver damage). Hemorrhagic diathesis, accompanied by hematuria, may be a manifestation of a side effect of anticoagulant therapy.
To differentiate renal hematuria from postrenal hematuria (from the urinary tract), a 3-glass sample can be used: the predominance of blood in the first and third portions of urine indicates damage to the bladder or urethra.
With unilateral isolated hematuria, one can think about kidney cancer, kidney tuberculosis, renal vein thrombosis. In case of bilateral renal hematuria, the presence of hypocoagulation can be assumed; it is recommended to conduct a study on the content of uric acid, immunoglobulins, circulating immune complexes, C3 and C4 complement components, cryoglobulins, HBS antigen and other markers of hepatitis, and antistreptococcal antibodies in the blood.
When hematuria is combined with fever and other systemic manifestations of diseases, it is necessary to conduct a bacteriological examination of urine and blood, a blood test for LE cells and antinucleolar factor.
Painful hematuria that occurs after renal colic is characteristic of urolithiasis and renal infarction. Painful hematuria, accompanied by blood clots, is observed with tumors of the urinary system. Hematuria in combination with acutely developed hypertension makes one think of acute nephrotic syndrome.
Hemoglobinuria
There are two possible sources of hemoglobin in the urine - red blood cells that enter the urine and are hemolyzed in it, or plasma hemoglobin that passes through the kidney filter (if its level in the blood plasma is high). The presence of free hemoglobin in the urine during hematuria is a common phenomenon, since urine is not a physiological environment for red blood cells, and in it they are quickly destroyed. How quickly this happens depends on several factors, the main of which are the osmotic stability of red blood cells and the length of stay of cellular elements in the urine. On the other hand, there is no direct relationship between the rate and degree of hemolysis on urine osmolality, pH, concentration of sodium chloride, ascorbic acid or protein. The faster diagnostic technology develops, the more chemical diagnostic methods replace the microscopic method.
True hemoglobinuria is caused by intravascular hemolysis. In this case, hemoglobin appears in the urine after the haptoglobin-binding capacity of plasma and tubular reabsorption of hemoglobin are saturated. Under normal conditions, this occurs when the concentration of free hemoglobin in the serum is approximately 60 μmol/L (1 g/L) or higher. Hemoglobinuria is observed with toxic infections, chemical toxicosis, with damage to red blood cells by phenylhydrazine, aniline dyes and/or sulfonamides and is combined with severe hemolytic anemia. Along with hemoglobin, myoglobin may be present in the urine, which has approximately the same effect on the results of the urine strip test as hemoglobin. Myoglobinuria is detected when the serum myoglobin level is 9-12 µmol/l (150-200 mg/l) or higher. Hemoglobin and myoglobin can appear in free form after severe damage to muscle tissue (crash syndrome). The appearance of hemoglobin is observed during transfusion of incompatible blood and as a complication of difficult childbirth. Sometimes hemoglobin in the urine can be detected after physical activity (so-called march hemoglobinuria). There are other forms of paroxysmal hemoglobinuria in which slight acidification of the plasma during sleep can cause hemolysis.
With true hemoglobinuria, there are no red blood cells in the urine sediment; with hemolysis of red blood cells directly in the urine, dissolved hemoglobin is combined with still remaining cells.
The finding of hematuria or hemoglobinuria may be an important clinical symptom of a serious disease and requires further clinical investigations aimed at identifying the causes.
Table No. 1 presents the indications for examination using diagnostic test strips for determining red blood cells and hemoglobin in urine (Uribel, Uripolian, Albufan, Pentaphan, Uriskan, Combourg-Test, etc.):
Table No. 1
Mass examination
| Diagnostics | Monitoring | |
| pregnant women | glomerulonephritis | pregnancy |
| athletes | nephrosclerosis | kidney disease |
| school age children | nephrosis | urolithiasis disease |
| newborns | pyelonephritis cystitis | transplantation |
| hospitalized | urogenital tuberculosis | diabetes |
| patients belonging to the “line of first contact” | urolithiasis disease | hypertension |
| aged people | Fanconi syndrome | systemic lupus erythematosus |
| eclampsia | kidney and urinary tract injuries | |
| tumors | polycystic kidney disease | |
| hemolytic anemia | eclampsia | |
| diabetes | ||
| hypertension | ||
| transfusion reactions during blood transfusion | ||
| muscle damage | ||
| toxic and hypoxic damage or degenerative changes in glomerular capillaries | ||
| tubular renal atrophy | ||
| kidney stone disease | ||
| congestive kidney with right ventricular failure of the heart | ||
| tubular necrosis |
Hemoglobinuria must be differentiated from other possible causes of urine color, such as alkaptonuria, melaninuria, porphyria, administration of drugs such as pyrazolone, amidopyrine or phenazopyridine, phenolic laxatives, or consumption of foods that can give a red tint to urine (beets).
Alkaptonuria
is
a hereditary disease, homogentisic acid is released in the urine, causing the child’s urine to darken when standing in the air, alkalizing or heating. Homogentisic acid is excreted in the urine in case of C-hypoavitaminosis. To detect homogentisic acid, add 3-4 drops of 10% sodium hydroxide solution to 0.5 ml of urine. If a blue-violet color develops after 1-2 minutes, the reaction is positive. In the absence of homogentisic acid in the urine, the urine remains colorless.
Melaninuria
observed in patients with melanoma. With metastases to the liver, a large amount of colorless melanogen is released, which is oxidized to melanin in the excreted urine. The addition of ferric chloride, bromine water, potassium bichromate, and dilute sulfuric acid to such urine causes a black-brown color.
Neither alkaptonuria nor melaninuria give positive staining to the diagnostic zones for blood and hemoglobin on the Urigem test strips
Test principle
The test is based on the pseudoperoxidase effect of hemoglobin, which catalyzes the oxidation of the chromogen by stabilized organic hydroperoxide.
Sensitivity and Specificity
At this point in time, the reaction zones of any manufacturer of test strips for free hemoglobin are very sensitive. As control microscopic examinations of urine have shown, the test does not respond to normal physiological levels of hemoglobin and red blood cells. A weakly positive reaction appears in the presence of hemoglobin, even in a concentration equivalent to approximately 3-5 red blood cells in 1 μl of urine. 5-10 red blood cells in 1 μl of urine appear as tiny light green dots or specks in the reaction zone. The test is less sensitive to intact red blood cells. Therefore, whenever the test results are positive, it is necessary to repeat it one or more times and refer the patient for further detailed examination.
The reaction zone of the tests reacts approximately the same way to the presence of myoglobin as it does to hemoglobin.
Myoglobin is a muscle pigment, the renal myoglobin threshold is 9-12 µmol/l (150-200 mg/l). Myoglobinuria is divided into traumatic and non-traumatic (Table No. 2). In terms of its chemical structure, myoglobin is close to hemoglobin, therefore chemical tests for hemoglobin give a positive reaction to myoglobin.
Table No. 2
| Myoglobinuria traumatic | Non-traumatic myoglobinuria |
| Extensive muscle tissue injuries (pressure syndrome, crash syndrome) | Muscle vascular thrombosis |
| Electric shock | Convulsions |
| Myositis | |
| Amyotrophy | |
| CO poisoning | |
| Paroxysmal myoglobinuria | |
| Epidemic myoglobinuria | |
| Myocardial infarction |
Differential diagnosis is carried out using a qualitative test: 2.8 g of crystalline ammonium sulfate is dissolved in 5 ml of urine and filtered through a paper filter. If myoglobin is present in the urine, then the color of the filtrate is red-brown; if there was hemoglobin in the urine, the color corresponds to the color of normal urine, since ammonium sulfate precipitates 80% of the hemoglobin.
The test is much less sensitive to leukocytes; it only indicates their presence in the urine with a weakly positive reaction if more than 50-100 leukocytes are in 1 μl of urine.
A positive test reaction may occur in the presence of bacterial peroxidases; in samples significantly contaminated with bacteria or fungi, the test may give a false positive result.
Influence of Side Factors
The sensitivity of the test is affected by the specific gravity of urine and the presence of various inhibitors of physiological and medicinal origin (mainly ascorbic and gentisic acids). In a urine sample of low specific gravity and low concentration of inhibitors, the sensitivity of the test can be increased by one square of the color scale. In samples with a high specific gravity in the presence of a large number of inhibitors, on the contrary, the sensitivity can be reduced by one square of the color scale. The results of determining blood and hemoglobin in urine are not affected by either the pH value or the presence of nitrites.
Test score
A positive test result is indicated by a change in the color of the reaction zone of the test strip. In the presence of free hemoglobin (hemoglobinuria or hemolysis of initially present red blood cells), the entire sensory zone turns more or less homogeneous green. Unchanged (whole) red blood cells (microhematuria) appear as intensely colored green dots or spots on the unstained reagent zone or uniform green coloring of the entire zone (macrohematuria). Coloration is assessed semi-quantitatively by comparison with a color scale. If the color of the reagent zone is intermediate between two squares of the scale, then the result is determined by the closest color zone of the scale or the average value.
Color scale for determining red blood cells (1st scale) and free hemoglobin (2nd scale).
Symptoms
Traces of hemoglobin in the urine of women, men and children are detected by the results of a study of the constituent components of urine.
Signs of pathology appear as follows:
- frequent urge to urinate;
- attacks of spasmodic pain in the lumbar spine from the side of the kidneys;
- urine takes on a rich dark brown hue;
- decreased physical activity;
- fast fatiguability;
- dizziness and a feeling of lack of air (occurs with severe hemoglobinuria, which led to the development of chronic anemia);
- headache;
- decreased blood pressure;
- pale skin;
- drowsiness.
Most patients who have traces of hemoglobin in their urine do not always experience the full list of these symptoms. The presence of this protein substance can be diagnosed completely by chance based on the results of a routine examination.
Especially if there are chronic foci of bacterial infection in the human body, he plays intensive sports, comes into daily contact with chemicals of toxic etiology, or takes medications with hemolytic properties.
Characteristics of forms of hemoglobinuria
Paroxysmal nocturnal hemoglobinuria
A distinctive feature of paroxysmal nocturnal hemoglobinuria (Marchiafava-Miceli disease) is attacks of intravascular hemolysis (hemolytic crises), developing mainly at night. The disease is registered with a frequency of 1:500,000. Hemolytic crises can be provoked by hypothermia, infection, vaccination, blood transfusions, physical activity, and surgical interventions.
Paroxysms of hemolysis of red blood cells are accompanied by fever, arthralgia, drowsiness, chest pain, abdominal and lower back pain. Signs of increasing iron deficiency anemia are general weakness, yellowness of the skin and mucous membranes. Characterized by enlargement of the liver and spleen. Dark-colored urine is observed in only a quarter of patients with paroxysmal nocturnal hemoglobinuria.
The most dangerous manifestations of paroxysmal nocturnal hemoglobinuria are thrombosis of mesenteric vessels, renal vessels, and peripheral vessels. Thrombosis of the hepatic veins is accompanied by a sharp increase in the size of the liver, progressive ascites, and varicose veins of the esophagus. Persistent hemosiderinuria often leads to tubular nephritis; at the height of a hemolytic crisis, acute renal failure may develop.
Paroxysmal nocturnal hemoglobinuria often develops in patients with aplastic anemia, preleukemia or acute myeloid leukemia, and therefore requires a complete hematological examination of the patient.
Morning hematuria is detected in the urine of patients with paroxysmal nocturnal hemoglobinuria
March hemoglobinuria
The symptoms of marching hemoglobinuria are usually more subtle and develop gradually. Chills and fever are uncharacteristic. Weakness is noted, which may also be a consequence of general physical fatigue from the forced march. At the same time, a pathognomonic sign of this form of hemoglobinuria is the dark color of urine. After the cessation of the marching load, the state of health returns to normal, the urine becomes lighter.
It has been noticed that almost all people who are faced with marching hemoglobinuria have pronounced lumbar lordosis. This form of hemoglobinuria has no independent clinical significance.
Cold paroxysmal hemoglobinuria
A rare form of hemolytic anemia - paroxysmal cold hemoglobinuria occurs in attacks. Paroxysms of cold hemoglobinuria are usually provoked by hypothermia and are accompanied by hyperthermia (sometimes up to 40°C), severe chills, nausea and vomiting, and abdominal pain. Hepato- and splenomegaly, yellowish color of the skin and sclera, and characteristic color of urine are detected.
Paroxysmal cold hemoglobinuria caused by acute viral infections usually resolves with the underlying disease. With syphilis and malaria, the disease can last for years.
Indications for the study
Traces of hemoglobin in the urine of women, men and children can only be detected in a biochemical laboratory.
The attending physician prescribes a urine test for the patient for the presence of molecules of this protein substance if there are signs of the following pathologies:
- inflammatory processes in the organs of the genitourinary system, the development of which is accompanied by purulent and sanguineous discharge;
- severe burns of the skin surface affecting more than 30% of the body;
- intoxication of the body caused by prolonged exposure to toxic substances of chemical or biological origin;
- infection with scarlet fever, diphtheria, typhoid fever, malaria, syphilis;
- rejection of donor blood;
- the period of rehabilitation after surgery (the factor of internal bleeding is excluded);
- perforated ulcer;
- severe injuries to the kidneys, liver and spleen;
- prolonged hypothermia of the body;
- all types of anemia.
A urine test for the presence of traces of hemoglobin is carried out during the process of diagnosing the patient, during the course of treatment, and also 1-2 weeks later following the results of recovery. For example, infection with a streptococcal infection requires repeated urine testing 10 days after the symptoms of the disease disappear.
Preparing and conducting analysis
In order for the results of a general urine test to be as reliable as possible, it is recommended to follow the following preparation rules before giving urine:
- on the evening before donating urine, do not eat vegetables and fruits, the natural pigments of which can change the color shade of urine (carrots, cranberries, beets);
- 24 hours before visiting the laboratory, stop taking medications with diuretic properties;
- 3 days before the test do not drink alcohol;
- 12 hours before the examination, do not eat food with a high content of hot spices, the presence of which can lead to irritation of the mucous membrane of the urinary system;
- 5 days before diagnosis, stop taking medications, the side effects of which can lead to hemolysis of red blood cells.
These are the basic rules for preparing for a urine test for signs of traces of hemoglobin. Otherwise, a person must lead a normal lifestyle so that the results of a urine test are objective.
The step-by-step process for taking a test to detect traces of hemoglobin is as follows:
- After waking up from sleep, you must perform thorough genital hygiene using soap, warm water and a clean, dry towel.
- Take a sterile container for collecting urine, which can be purchased directly from a laboratory or pharmacy.
- Flush a small amount of morning urine down the toilet to cleanse the urethra, and then fill a jar with urine for testing.
- Close the container with a lid, and then deliver the biological material for laboratory testing within 1 hour.
On average, at least 50 ml of urine will be required. This is the minimum amount of urine required for this type of analysis.
Women are advised to refrain from donating urine during menstruation, as well as 2 days after the end of menstruation. This is necessary in order to minimize the risk of blood drops getting into the urine. Their presence will lead to distorted results.
Decoding the results
The results of the examination should be deciphered by the attending physician, who conducts an initial examination of the patient and then prescribes a urine sample. A person who does not have health problems should not have signs of hemoglobin in the urine.
The presence of even a small amount of this substance indicates a painful state of the body.
When to see a doctor
A visit to a general practitioner should take place within the first 24 hours after a person discovers the following symptoms indicating the presence of hemoglobin in urine:
- brown or red urine;
- dizziness and loss of strength;
- rapid physical fatigue;
- pallor;
- feeling of lack of air;
- drowsiness;
- headache;
- prolonged drop in blood pressure;
- cardiopalmus;
- nausea;
- loss of appetite;
- frequent urge to urinate.
The appearance of hemoglobin molecules in urine is just one of the symptoms of the underlying disease, the elimination of which will ensure the stabilization of biochemical processes in the body.
How to get it back to normal
In order to normalize the biochemical composition of urine, as well as to prevent further release of free hemoglobin, it is necessary to eliminate the cause of intravascular hemolysis of red blood cells.
Hemoglobinuria caused by exposure to cold or heavy physical exertion does not require the use of drug therapy. The use of medications is advisable only in the case of intoxicated breakdown of red blood cells or acquired anemia.
Medications
In order to normalize free hemoglobin levels, the following medications can be used:
- Troxerutin - this is an angioprotective agent that strengthens the walls of veins and capillaries, prevents vascular damage and hemolysis of red blood cells (1 capsule is prescribed 2-3 times a day for 1 week, and the average cost of the medication is 165 rubles);
- Active iron is an organic drug that replenishes the physiological loss of hemoglobin while measures are taken to eliminate the causes of hemoglobinuria (the medication is taken at the same time, 1 tablet per day with food, and its cost is 105 rubles per pack);
- Activate iron with lactoferin is a drug that replenishes iron deficiency, and also stabilizes the level of hemoglobin in the blood, normalizes metabolic processes (take 1 tablet per day, and the average price of the drug is 550 rubles for 20 tablets);
- Detralex is a medicine that stabilizes the condition of capillaries, prevents vascular damage and hemolysis of red blood cells (1 tablet per day is prescribed, and the cost of the medicine is 230 rubles for a blister of 10 tablets).
The above drugs help prevent further breakdown of red blood cells, maintain the tone of the walls of blood vessels, and stabilize hemoglobin levels. Without eliminating the main causes that change the biochemical composition of blood and urine, the use of these medications will not have a lasting therapeutic effect.
Traditional methods
Traditional medicine is not able to influence the stabilization of free hemoglobin levels. Therefore, their use is not advisable.
Other methods
If it is necessary to carry out emergency treatment measures to stabilize the cellular composition of the blood, the method of hematological transfusion is used. The patient is given a transfusion of donor blood components to saturate the body with additional red blood cells.
The treatment procedure is performed in a hospital inpatient department. Hematological transfusion is indicated for use in patients who have experienced massive hemolysis of red blood cells with critical loss of hemoglobin and the risk of death.
Treatment of hemoglobinuria
Therapeutic tactics for various forms of hemoglobinuria are determined by a hematologist. March and paroxysmal cold hemoglobinuria usually resolve without special intervention. In the case of the development of chronic autoimmune cold hemoglobinuria, glucocorticoids and immunosuppressants (cyclophosphamide, azathioprine) are prescribed.
Therapy for paroxysmal nocturnal hemoglobinuria is mainly symptomatic: red blood cell transfusions, administration of indirect anticoagulants, and iron supplementation. For red bone marrow hypoplasia, glucocorticosteroids (prednisolone), anabolic drugs (methandienone) or androgens, and antithymocyte immunoglobulin are prescribed. In cases of severe hypersplenism, splenectomy may be warranted. If there is no effect from other methods of treating paroxysmal nocturnal hemoglobinuria, the issue of bone marrow transplantation from an HLA-compatible donor is decided.
In order to prevent the development of hemoglobinuria, it is recommended to avoid provoking factors: poisoning, intoxication, infectious diseases, excessive physical exertion, injuries, etc.
Possible complications
Patients with traces of hemoglobin in their urine should undergo a thorough examination with further treatment of the underlying disease.
The lack of qualified therapy can lead to the development of the following complications:
- rapid weight loss;
- decreased ability to work;
- erectile dysfunction in men;
- digestive dysfunction;
- development of hemolytic anemia;
- functional disorders in the kidneys;
- thrombosis of the great vessels;
- pulmonary hypertension;
- bone marrow failure;
- aplastic anemia;
- oxygen starvation of the tissues of internal organs caused by a constant deficiency of hemoglobin;
- progressive hemolysis of red blood cells with a radical change in the cellular composition of the blood;
- the onset of death caused by vascular thrombosis, impaired renal function and severe anemia.
Traces of hemoglobin in the urine of women, men and children are determined by biochemical examination of urine. The appearance of molecules of this protein compound indicates a disruption in the functioning of the organs of the hematopoietic system, kidneys, liver and spleen tissues, exposure to particularly dangerous toxic substances, heavy physical exertion or prolonged hypothermia of the body.
Traces of hemoglobin in the urine appear due to the massive death of red blood cells, the breakdown of which leads to the release of an excess amount of this protein compound into the blood plasma. The lack of timely examination and qualified therapy leads to the development of a large number of complications affecting the performance of internal organs.
General urine analysis (with microscopy of urinary sediment)
What is a general urine test?
A general urinalysis includes assessment of the physicochemical characteristics of urine and microscopy of sediment. This study allows you to evaluate the function of the kidneys and other internal organs, as well as identify the inflammatory process in the urinary tract. Together with a general clinical blood test, the results of this study can tell quite a lot about the processes occurring in the human body and, most importantly, indicate the direction of further diagnostic search.
Physico-chemical characteristics of urine:
- color;
- transparency;
- specific gravity (relative density);
- pH (acidity);
- protein;
- glucose;
- bilirubin;
- urobilinogen;
- ketone bodies;
- nitrites;
- hemoglobin.
Microscopy of urinary sediment (the study is done in case of pathology in a general urine analysis or at the request of the customer).
Indications for the purpose of analysis:
- diseases of the urinary system;
- suspected diabetes mellitus;
- assessment of the toxic state of the body;
- assessment of the course of the disease;
- monitoring the development of complications and the effectiveness of treatment;
- Persons who have had a streptococcal infection (tonsillitis, scarlet fever) are recommended to take a urine test 1-2 weeks after recovery.
Color
Normal urine has a straw-yellow color of varying intensities. The color of urine in healthy people is determined by the presence of substances formed from blood pigments (urobilin, urochromes, hematoporphyrin, etc.). The color of urine changes depending on its relative density, daily volume and the presence of various coloring components entering the human body with food, medications, and vitamins. Normally, the more intense the yellow color of the urine, the higher its relative density and vice versa. Concentrated urine has a brighter color. However, the normal color of urine does not indicate that it is the urine of a healthy person.
Transparency
Normal freshly passed urine is clear. A small cloud of turbidity may also appear in normal urine due to epithelial cells and mucus. Severe cloudiness of urine can be caused by the presence in it of red blood cells, leukocytes, fat, epithelium, bacteria, and significant amounts of various salts (urates, phosphates, oxalates). The causes of cloudy urine are determined by microscopy of sediment and chemical analysis.
Specific gravity (relative density)
Measuring urine specific gravity is a simple test that measures the ability of the kidneys to concentrate urine and dilute urine. A decrease in the concentrating ability of the kidneys occurs simultaneously with a decrease in other renal functions. Normally functioning kidneys are characterized by wide fluctuations in the specific gravity of urine during the day, which is associated with periodic intake of food, water and fluid loss from the body (sweating, breathing).
Protein
Protein is normally absent in urine or there are small traces of it, since protein molecules are large molecules that are not able to pass through the membrane of the glomeruli.
The appearance of proteinuria in the urine can be:
- physiological (orthostatic, hypothermia, after increased physical activity);
- glomerular (glomerulonephritis, the action of infectious and allergic factors, hypertension, cardiac decompensation);
- tubular (amyloidosis, acute tubular necrosis, interstitial nephritis, Fanconi syndrome);
- prerenal (myeloma, muscle tissue necrosis, erythrocyte hemolysis);
- postrenal (for cystitis, urethritis, colpitis).
Glucose
Normally, there is no sugar in the urine, since all glucose, after being filtered through the glomerular membrane of the kidneys, is completely absorbed back into the proximal tubules.
The appearance of glucose in the blood, glucosuria, can be:
- physiological (under stress, taking increased amounts of carbohydrates in older people);
- extrarenal (diabetes mellitus, pancreatitis, diffuse liver damage, pancreatic cancer, hyperthyroidism, Cushing's disease, pheochromocytoma, hyperthyroidism, acromegaly, traumatic brain injury, stroke, poisoning with carbon monoxide, morphine, chloroform);
- renal (renal diabetes, chronic nephritis, acute renal failure, pregnancy, phosphorus poisoning, certain medications).
Glucose is a substance with a high renal excretion threshold. The renal excretion threshold is the concentration of a substance in the blood, exceeding which leads to the cessation of its reabsorption in the tubules. When the blood glucose concentration is more than 8.8-9.9 mmol/l, sugar appears in the urine.
Urobilinogen
Urobilinogen bodies (I-urobilinogen, d-urobilinogen, third urobilinogen, stercobilinogen) are derivatives of bilirubin and are normal products of catabolism, which under physiological conditions are formed at a certain rate, constantly excreted in feces and in small quantities in urine. Normal urine contains traces of urobilinogen. Its level increases sharply with hemolytic jaundice (intravascular destruction of red blood cells), as well as with toxic and inflammatory lesions of the liver, intestinal diseases (enteritis, constipation). With subhepatic (obstructive) jaundice, when there is complete blockage of the bile duct, there is no urobilinogen in the urine.
Ketone bodies
Ketone bodies include acetone, acetoacetic and beta-hydroxybutyric acids. A healthy person excretes 20-30 mg of ketones per day in urine. An increase in the excretion of ketones in the urine, ketonuria appears when there is a violation of carbohydrate, fat or protein metabolism.
Nitrites
There are no nitrites in normal urine. In urine, they are formed from nitrates of food origin (when eating plant foods) under the influence of bacteria, if the urine was in the bladder for at least 4 hours. Detection of nitrites in the urine (positive test result) indicates infection of the urinary tract. However, a negative result does not always exclude bacteriuria. Urinary tract infection varies among different populations and is dependent on age and gender. The following categories of people are more susceptible to an increased risk of asymptomatic urinary tract infections and chronic pyelonephritis, other things being equal:
- girls and women;
- elderly people (over 70 years old);
- men with prostate adenoma;
- diabetic patients;
- patients with gout;
- patients after urological operations or instrumental procedures on the urinary tract.
Bacteriuria
False-positive reactions (bacterial contamination of the sample during collection and storage; when taking phenazopyridine).
Hemoglobin
Normally absent. Hemoglobinuria is the result of intravascular, intrarenal, urinary hemolysis of red blood cells with the release of hemoglobin, or muscle damage and necrosis, accompanied by an increase in plasma myoglobin levels. Hemoglobinuria is characterized by red or dark brown (black) urine, dysuria, and often lower back pain. Hemoglobinuria must be distinguished from hematuria, alkaptonuria, melaninuria, and porphyria. With hemoglobinuria, there are no red blood cells in the urine sediment, anemia with reticulocytosis and an increase in the level of indirect bilirubin in the blood serum are detected.
Microscopy of urinary sediment
In urinary sediment, organized sediment is distinguished (cellular elements, cylinders, mucus, bacteria, yeast fungi) and unorganized (crystalline elements).
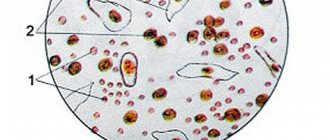
Red blood cells
2 million red blood cells are excreted in the urine per day, which, when examining urine sediment, is normally less than 3 red blood cells per field of view for women, and 1 red blood cell per field of view for men. Anything higher is hematuria.
Highlight:
- gross hematuria (when the color of urine is changed);
- microhematuria (when the color of urine is not changed, and red blood cells are detected only under a microscope).
In urinary sediment, red blood cells can be unchanged (containing hemoglobin) and changed (deprived of hemoglobin, leached). The appearance of leached red blood cells in the urine is of great diagnostic importance, because they most often have a renal origin and are found in glomerulonephritis, tuberculosis and other kidney diseases. Fresh, unchanged red blood cells are more likely to cause damage to the urinary tract (urolithiasis, cystitis, urethritis).
Leukocytes
Leukocytes in the urine of a healthy person are contained in small quantities (in men 0–3, in women and children 0–6 leukocytes per field of view). An increase in the number of leukocytes in the urine (leukocyturia) indicates inflammatory processes in the kidneys (pyelonephritis) or urinary tract (cystitis, urethritis). To establish the source of leukocyturia, a three-glass test is used: the predominance of leukocytes in the first portion indicates urethritis or prostatitis, in the third - cystitis, an even distribution of leukocytes in all portions can most likely indicate kidney damage.
So-called sterile leukocyturia is possible. This is the presence of leukocyturia in the absence of bacteriuria and dysuria (with exacerbation of chronic glomerulonephritis, contamination during urine collection, condition after treatment with antibiotics, bladder tumors, renal tuberculosis, interstitial analgesic nephritis).
Urethral syndrome. This is frequent, painful urination and leukocyturia in the absence of bacteriuria. Occurs predominantly in women. In 30-40% of cases in women with symptoms of urinary tract infection, bacteriuria cannot be detected. The reasons for the negative result are that the true causative agent of this condition, as a rule, is anaerobic bacteria, ureaplasma, chlamydia, gonococcus, and viruses. And they all require sowing on special media.
Epithelial cells
Epithelial cells are almost always found in urinary sediment. Normally there are no more than 10 of them in the field of view.
Epithelial cells have different origins:
- cells of stratified squamous keratinizing epithelium (washed off with night urine from the external genitalia);
- cells of stratified squamous non-keratinizing epithelium (from the distal parts of the male and female urethra and vagina, of little diagnostic value);
- transitional epithelial cells (lining the mucous membrane of the bladder, ureters, pelvis, large ducts of the prostate gland);
- cells of the renal (tubular) epithelium (lining the renal tubules).
Cylinders
The cylinder is a protein that is coagulated in the lumen of the renal tubules and includes in its matrix any contents of the lumen of the tubules. The cylinders take the shape of the tubules themselves (cylindrical cast). In the urine of a healthy person, single cylinders can be detected in the field of view of a microscope per day. Normally, there are no casts in a general urine analysis. The appearance of casts (cylindruria) is a symptom of kidney damage. The type of cylinders has no special diagnostic significance.
Bacteria
Normally, urine in the bladder is sterile. When urinating, microbes from the lower part of the urethra enter it, but their number is not > 10,000 in 1 ml. Bacteriuria is defined as the detection of more than one bacterium in the field of view (qualitative method), which implies the growth of colonies in culture exceeding 100,000 bacteria per 1 ml (quantitative method).
It is clear that urine culture is the gold standard for diagnosing urinary tract infections. The presence of bacteria in the urine in the absence of complaints is regarded as asymptomatic bacteriuria. A similar condition often occurs with organic changes in the urinary tract; in women who are promiscuous and in older people. Asymptomatic bacteriuria increases the risk of urinary tract infection, especially during pregnancy (infection develops in 40% of cases).
The detection of bacteria in a urine test indicates an infectious lesion of the urinary system (pyelonephritis, urethritis, cystitis, etc.). The type of bacteria can only be determined through bacteriological examination.
Yeasts
The detection of yeast of the genus Candida indicates candidiasis, which most often occurs as a result of irrational antibiotic therapy, the use of immunosuppressants, and cytostatics.
Determining the type of fungus is possible only through bacteriological examination.
Slime
Mucus is secreted by the epithelium of the mucous membranes. Normally absent or present in urine in small quantities. During inflammatory processes in the lower parts of the urinary tract, the mucus content in the urine increases. An increased amount of mucus in the urine may indicate a violation of the rules of proper preparation for taking a urine sample.
Crystals (disorganized sediment)
Urine is a solution of various salts, which can precipitate (form crystals) when the urine stands. Low temperature promotes the formation of crystals. The presence of certain salt crystals in the urinary sediment indicates a change in the reaction towards the acidic or alkaline side. Excessive salt content in urine contributes to the formation of stones and the development of urolithiasis. At the same time, the diagnostic value of the presence of salt crystals in urine is usually small.