- Types of brain and spinal cord tumors
- How common are brain and spinal cord tumors?
- Risk factors for brain and spinal cord tumors in children
- Diagnosis of brain and spinal cord tumors
- Are stages determined for tumors of the brain and spinal cord?
- Treatment of central nervous system tumors
- What happens after treatment ends?
The term “central nervous system” (CNS) refers to the brain and spinal cord. Tumors of the central nervous system in children and adults often develop in different parts, from different types of cells, have a different prognosis (outcome) and require a different approach to treatment.
The brain is the center of thinking, feeling, memory, speech, vision, hearing, movement, etc. The spinal cord and nerves carry information from the brain to the rest of the body and back.
This information enables muscle movement, helps coordinate the function of internal organs, etc. The brain and spinal cord are bathed in cerebrospinal fluid. This fluid fills the ventricles of the brain.
The brain includes two hemispheres, the diencephalon, the cerebellum and the brainstem. Each part of the brain has its own functions. Tumors of different parts of the central nervous system impair different functions and cause a variety of symptoms.
Symptoms of a central nervous system tumor in young (under 3 years of age) children may not accurately reflect the localization (location) of the tumor and are often nonspecific, manifesting themselves in the form of irritability, crying, loss of appetite, and vomiting.
The hemispheres of the brain are responsible for thinking, emotions, speech, muscle movements, vision, hearing, tactile sensitivity and the sensation of pain.
Symptoms of tumors of the cerebral hemispheres depend on the area affected and include seizures, speech impairment, mood changes in the form of depression (depression), personality changes, weakness of one side of the body, visual, hearing or sensory impairment.
The diencephalon is responsible for sensation and body movement, temperature regulation, thirst, hunger and fluid balance in the body, as well as the production of pituitary hormones.
The cerebellum controls body movement. Tumors of this location lead to disturbances in gait, loss of precise movements of the arms and legs, and disturbances in the rhythm of speech.
The brain stem contains long nerves that carry signals to the muscles and provide sensation. Special centers in the brain stem are responsible for breathing and heart activity.
Tumors of this location can cause weakness, muscle stiffness, disturbances in sensitivity, hearing, facial expressions and swallowing. Double vision and gait disturbance are common early symptoms of a brain stem tumor.
The spinal cord contains long bundles of nerves that carry signals that control muscle movement, sensation, bladder and bowel function. Spinal cord tumors can cause weakness, numbness, and paralysis of the limbs.
Cranial nerves, located at the base of the brain, can become sources of tumor development.
The most common of these in children is optic nerve glioma, which can lead to blindness.
A tumor of the auditory nerve can cause deafness in one or both ears, a tumor of the facial nerve can cause facial paralysis, and a tumor of the trigeminal nerve can cause pain.
Types of brain and spinal cord tumors
Tumors of the brain and spinal cord can develop from a variety of cells and tissues. Some tumors contain different types of cells at the same time. There are primary (arising in the same organs) and metastatic (arising in other organs and spreading to the brain or spinal cord) tumors.
In children, metastatic tumors of the brain and spinal cord are less common than primary tumors. Unlike other tumors, brain and spinal cord tumors rarely metastasize (spread) to distant organs. They grow locally within the brain, destroying healthy tissue around it.
Astrocytomas develop from astrocyte cells and account for almost half of all pediatric brain tumors. They often spread widely into the brain and are called infiltrating astrocytomas. In rare cases, these astrocytomas spread to the spinal cord. With rare exceptions, they do not extend beyond the brain and spinal cord. These tumors can rarely be completely removed by surgery.
Infiltrating astrocytomas are classified as low-, intermediate-, and high-grade tumors. Low-grade astrocytomas grow slower than other tumors and are most common in children.
The most favorable prognosis (outcome) is observed in children with non-infiltrating astrocytoma, which is rare.
Oligodendrogliomas arise from oligodendrocyte cells. By the nature of their growth and spread, they resemble astrocytomas. Only in some cases is it possible to completely remove them.
Ependymomas develop from the ependymal cells of the ventricles of the brain and account for 9% of all brain tumors. As these tumors grow in size, they can interfere with the flow of cerebrospinal fluid from the ventricles, causing them to dilate. Unlike astrocytomas and oligodendrogliomas, ependymomas do not infiltrate normal brain tissue. In this regard, in many cases it is possible to completely remove the tumor.
Ependymomas of the spinal cord respond well to surgical treatment. Sometimes these tumors can spread into the spinal cord but do not spread beyond the central nervous system. Gliomas . Optic nerve glioma is a low-grade tumor and is often associated with the hereditary disease neurofibromatosis type 1. This tumor is rarely fatal, but can cause significant visual impairment.
Neuronal tumors develop from primitive stem cells and are diagnosed mainly in childhood.
Medulloblastomas arise from cerebellar neurons, are characterized by rapid growth and account for 15% of brain tumors in children.
Primitive neuroectodermal tumors (PNETs) are called pineoblastomas when they arise in the pineal gland, or neuroblastomas when they arise in the cerebral hemispheres. The prognosis of the disease is best in patients with medulloblastoma.
Gangliogliomas contain both mature neurons and glial cells. They respond well to surgical or combined treatment (surgery and radiation).
Tumors of the choroid plexus develop from the vessels of the ventricles of the brain and are, as a rule, benign (papillomas), which respond well to surgical treatment. Sometimes malignant variants of the tumor (carcinoma) also occur.
Craniopharyngiomas account for 6-9% of all CNS tumors in children. The average age of patients at the time of diagnosis of the disease is 8 years. Often tumors are located near the optic nerve, which makes surgical removal of the tumor difficult. They can put pressure on the pituitary gland, causing hormonal imbalances. These tumors are subject to surgical and radiation treatment.
Schwannomas develop from Schwann cells surrounding nerves. These tumors are usually benign and are located near the cerebellum. They are rare in children and, as a rule, are combined with a hereditary tumor syndrome - neurofibromatosis.
Meningiomas arise from the membranes of the brain and spinal cord and lead to their compression. They occur much more often in adults compared to children. These tumors are benign and can be treated surgically. However, sometimes they are located close to vital structures and make surgical intervention difficult. The malignant version of the tumor, meningiosarcoma, often recurs (occurs again) after surgery and rarely metastasizes (spreads) to other organs.
Chordomas arise in the initial or terminal part of the spinal cord and have a tendency to recur frequently.
Germ cell tumors of the central nervous system occur mainly in children and are most often represented by germinoma, the treatment of which is chemotherapy and radiation. Yolk sac tumors are rarely treated with surgery. In these patients, combined chemoradiotherapy is used.
Treatment of brain tumors in children in Israel – prices
At the Top Assuta clinic, patients are treated to experienced doctors, comfortable conditions, and an individual approach. It is important that high-quality medical care in Israel costs 30% less than in Europe and half as much as in America. You can find out the estimated cost of diagnosis and treatment from our medical managers by leaving a request on our website. The final price is determined only after a complete examination.
Diagnostic prices from $1790
from $1790 to $18700
Brain tumor
| Type of service | Prices |
| Basic diagnostic package | from $1790 |
| Non-surgical treatment | from $13600 |
| Operation | from $18700 |
The advantages of treatment at Top Assuta are undeniable
Treatment of brain tumors in children in Israel is a synthesis of modern techniques, the experience of doctors and advanced developments for the successful treatment of young patients.
- The clinic’s doctors annually perform hundreds of successful operations to remove brain tumors in children.
- Modern equipment makes it possible to make a diagnosis with 100% accuracy.
- Individual selection of a combination of treatment methods allows you to achieve recovery with a minimal likelihood of side effects.
- A loyal pricing policy makes treatment in Israel accessible to more patients.
- A representative of the international department helps in solving everyday and organizational issues.
- 5
- 4
- 3
- 2
- 1
(19 votes, average: 5 out of 5)
How common are brain and spinal cord tumors?
Tumors of the central nervous system occupy the second place among malignant tumors in children, second only to lymphomas and leukemia, and account for 14-20% of them. In Russia, 1.4 per 100 thousand children under the age of 16 fall ill annually, which is approximately 450 cases per year. Children of preschool age get sick more often: the peak incidence occurs at 2-7 years.
In the United States in 2004, it is expected that 18,400 cases of malignant tumors of the brain and spinal cord, as well as tumors of other parts of the nervous system, will be identified.
Of these, 1,700 central nervous system tumors will be diagnosed in children under 18 years of age.
Tumors of the cerebral hemispheres
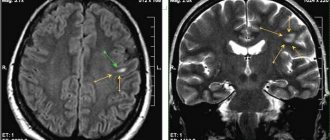
Supratentorial gliomas
are located in the cerebral hemispheres and account for about 30% of all brain tumors in children.
Treatment and prognosis depend on the location of the tumor and its growth rate. There are several types of such tumors: juvenile pilocytic astrocytoma, optic pathway glioma
(
optic glioma
) or
hypothalamic glioma
(see below),
oligodendroglioma
,
hemispheric astrocytoma
and
ganglioglioma
. Many of them cause seizures due to their location in the brain. If such a tumor is not in the area that controls speech, movement, vision or intelligence, then surgical removal is indicated. Sometimes only part of the tumor is removed, after which local radiation therapy and/or chemotherapy are additionally prescribed.
Gliomas of the visual pathways (optic gliomas).
About 5% of tumors in children are gliomas, developing in the area of the optic nerves and hypothalamus. Typically, these tumors are slow growing and respond well to surgery, radiation therapy, or chemotherapy. Because they affect the optic nerves and hypothalamus, children with these tumors often have visual and hormonal disturbances.
Craniopharyngiomas
are
nonglial tumors that make up 5% of all CNS tumors in children. Patients with these tumors are characterized by stunted growth because the affected area is near the pituitary gland. Vision problems are also common. The question of their treatment is quite complicated: complete removal of the tumor can lead to a cure, but at the same time it can cause disturbances in memory, vision, behavior and hormonal status. An alternative is partial excision combined with radiation therapy. After treatment of these tumors, children usually require long-term rehabilitation due to vision problems and/or hormonal disorders.
Germ cell tumors
make up a small part of brain tumors - about 4%. They develop in the region of the pineal gland or suprasellar region (i.e. “above the sella turcica”), above the pituitary gland. As a rule, they are diagnosed during puberty and occur in both boys and girls, but are slightly more common in boys. These tumors are often well treated with chemotherapy and radiation therapy used after surgical removal or biopsy, very often these tumors do not even need to be removed and biopsied, for diagnosis it is enough to look at tumor markers in the blood and cerebrospinal fluid (alphafetoprotein and human chorionic gonadotropin) and see characteristic changes on MRI , in addition, they are highly sensitive to chemotherapy and radiation and respond well even without surgical removal.
Tumors of the choroid plexus
constitute 1-3% of all CNS tumors in children.
The choroid plexuses are located in the ventricles of the brain, their main function is the production of cerebrospinal fluid. Tumors of the choroid plexus are benign ( papillomas
) and malignant (
choroid carcinomas
)
.
These tumors usually occur in young children (under 1 year of age) and often cause hydrocephalus. As a rule, they are removed surgically. For malignant tumors, chemotherapy is also prescribed, and in children over 3 years of age, radiation therapy.
Supratentorial PNETs
, pineoblastomas previously accounted for about 5% of all brain tumors in children. In the modern classification of CNS tumors, this term has been removed, because Using molecular genetic techniques, it was shown that under the mask of PNET, other tumors are masked, which cannot be distinguished using only a microscope and the eyes of a morphologist. Neurological symptoms depend on the location of the tumor - in particular, its proximity to the ventricles of the brain. For such tumors, treatment will depend on the diagnosis verified using molecular genetic methods.
Risk factors for brain and spinal cord tumors in children
Most CNS tumors are not associated with any risk factors and arise from unknown causes. However, some risk factors still exist.
Ionizing radiation is a proven factor that increases the risk of developing brain and spinal cord tumors. Ionizing radiation is used for both diagnostic and therapeutic purposes. Previously (50 years ago), low doses of radiation were used to treat ringworm (a fungal infection) of the scalp, which significantly increased the risk of developing brain tumors in the future. Currently, brain tumors can be caused by radiation therapy prescribed for another malignant tumor in the head and neck region.
Exposure to vinyl chloride (an odorless gas used in making plastics), exposure to aspartame (a sugar substitute), exposure to electromagnetic fields from cell phones or high-voltage lines, and head trauma are thought to increase the risk of brain tumors.
Family history (information about diseases in the family). Rarely, several cases of central nervous system tumors may occur in one family. There are known diseases that are accompanied by an increased risk of tumors of the brain and spinal cord.
- Neurofibromatosis type 1 (Recklinghausen disease) is the most common hereditary disease that increases the risk of tumors of the central nervous system and other parts of the nervous system (gliomas of the optic nerve and other localizations, neurofibromas of peripheral nerves).
- Neurofibromatosis type II is less common than Recklinghausen disease and is associated with the development of auditory nerve tumors, meningiomas, or spinal cord ependymomas.
- Tuberous sclerosis is also a hereditary disease and can be accompanied by the occurrence of non-infiltrating giant cell astrocytoma, as well as benign tumors of the skin, heart and kidneys.
- Hippel-Lindau disease increases the risk of developing hemangioblastomas (vascular tumors) of the cerebellum or retina, as well as kidney cancer.
- Li-Fraumeni syndrome leads to an increased risk of breast cancer, soft tissue sarcomas, leukemia, adrenal tumors, and gliomas.
Given the lack of precise causes of brain and spinal cord tumors in children, it is currently impossible to prevent most of them.
Treatment methods for brain tumors in children - effective and modern
Treatment of brain tumors of any nature should begin as early as possible, since the disease tends to progress quickly.
Drug therapy is needed to eliminate pain, relieve tissue swelling, and improve the general condition of the child. The drugs used are as safe as possible for the child’s body, but at the same time quite effective.
Chemotherapy . The Top Assuta clinic uses only modern chemotherapy drugs that have passed mandatory certification and are approved for use in pediatric oncology. Taking into account the child’s health status and the stage of development of the disease, doctors select the optimal combination of medications and their dosage. This allows for high effectiveness of treatment with a minimum number of side effects.
Immune therapy is the use of immunomodulators to stimulate the body's defenses to more effectively fight cancer. They use biological preparations based on cells of the immune system - interferon preparations, serums made individually for each patient from tumor cells.
Targeted therapy consists of targeted destruction of tumor cells. Targeted therapy drugs are monoclonal antibodies created from human white blood cells (leukocyte culture). Using transformation at the molecular level, they were “taught” to recognize special proteins produced by pathological cells. As a result, antibodies attack only cancer cells without affecting healthy ones.
Radiation therapy . Involves the use of linear accelerators for precise, short-term and effective impact. It is used before surgery to reduce the size of a tumor or after surgery to destroy remaining cancer cells. Healthy tissues are not damaged.
Radiosurgery . Doctors were able to remove brain tumors without blood, pain, anesthesia or tissue trauma. Cancer cells are burned out with a precisely directed beam of ionizing radiation while healthy tissue is preserved.
FUS ablation involves “vaporizing” the tumor with a high-intensity ultrasound beam. The undeniable advantage of the method is its targeted effect on tumor tissue.
Transnasal transsphenoidal tumor removal located in the pituitary gland is performed through the nasal passages - the tumor is captured with a special endoscope and also removed through the nasal cavity, or more precisely, through the sphenoid sinus.
Thus, there is no need to make incisions, the rehabilitation period is shortened - after 2 days the patient is already discharged. A shunt is performed to remove cerebrospinal fluid (CSF) from the cavities of the brain.
During the intervention, one end of the shunt is placed in the ventricle of the brain, and the other in the abdominal or thoracic cavity. The outflow of fluid allows you to relieve swelling, normalize intracranial pressure, and reduce pain. Surgery involves craniotomy (craniotomy). With its help, in most cases, the tumor can be completely removed. In Israeli clinics, trepanation is performed only after the precise location of the tumor has been established, in order to injure as little tissue as possible. Using various modern medical technologies, neurosurgeons remove the formation while minimally interfering with the cerebral structures. Brain surgery at Top Assuta takes place without pain or negative consequences for the body.
Treatment of brain tumors in children in Israel - parental reviews confirm this - is highly effective and zero traumatic for the child.
Diagnosis of brain and spinal cord tumors
For most patients, survival depends on the location of the tumor in the central nervous system and its extent. Currently, there are no methods for detecting brain and spinal cord tumors using blood tests or screening (pre-symptomatic diagnosis).
It must be emphasized that early detection of brain and spinal cord tumors has little effect on patient survival.
Symptoms of central nervous system tumors appear gradually and become more noticeable over time. However, some symptoms, such as a seizure, occur unexpectedly. For many children, an epileptic seizure is the first sign of a brain tumor.
Tumors that arise in the most important areas of the brain appear earlier than those that are localized in less important areas of the brain. Tumors of the central nervous system lead to disruption of certain body functions, depending on the location where they originate.
Tumors of the spinal cord often cause numbness and weakness of the extremities, while tumors of the base of the brain are accompanied by disturbances in movement and posture.
Tumors located inside the skull lead to increased intracranial pressure, which is accompanied by headache, nausea, vomiting, and blurred vision.
Headache is a common symptom of a brain tumor and occurs in 50% of cases.
In some children, increased intracranial pressure is accompanied by strabismus and double vision. In some cases, this can lead to complete loss of vision.
School-age children may experience decreased academic performance, increased fatigue, personality changes, and frequent vague intermittent headaches.
Young children may experience irritability, loss of appetite, developmental delays, and decreased intellectual and motor functions associated with increased intracranial pressure.
In infants, increased intracranial pressure can cause an increase in head size, bulging of the fontanelle, constant vomiting, and developmental delays.
Methods for diagnosing central nervous system tumors
Computed tomography (CT) in some cases in combination with intravenous contrast helps to determine the boundaries of the tumor and healthy tissue of the brain and spinal cord.
Magnetic resonance imaging (MRI) provides an even clearer picture of the tumor and surrounding tissue and is especially useful in diagnosing lesions of the brain stem and cerebellum.
Positron emission tomography (PET) uses low doses of radioactive glucose. It is taken up more by high-grade tumors and less by low-grade tumors compared to normal tissue. In addition, this method is used to evaluate the effectiveness of treatment.
Angiography (contrast study of blood vessels) of the vessels adjacent to the tumor helps to clarify the blood supply to the tumor.
Biopsy is the removal of a piece of tissue suspicious for a tumor for examination). In some cases, a piece of the tumor can be obtained using a so-called stereotactic fine needle biopsy under CT or MRI guidance.
A spinal tap is performed in the lumbar spine to obtain cerebrospinal fluid and examine it under a microscope to identify tumor cells.
A bone marrow biopsy can provide additional information about possible marrow involvement, especially in patients with medulloblastoma, which can spread beyond the central nervous system.
Blood and urine tests make it possible to evaluate the function of the liver, kidneys and other organs.
Brain tumors in children
Brain tumors in childhood account for 12-15% of all tumors and are characterized by a long asymptomatic period of illness, which allows them to reach a certain size before general brain symptoms appear with mild focal symptoms. This is due to the anatomical and physiological characteristics of the central nervous system and skull, the ability to stretch the cranial sutures and ventricles of the brain, and increase the subarachnoid fissures and cisterns of the brain.
Children with head tumors experience hydrocephalic symptoms , which include an increase in head circumference, delayed closure of the fontanels, divergence of cranial sutures, thinning of the bones of the cranial vault, the presence of digital impressions and blurring of the contours of the sella turcica on craniograms.
Hypertensive symptoms are also distinguished: vomiting, stupor, headache, forced head position, membrane symptoms. Headache and vomiting in young children usually appear later in the course of the disease. Regardless of the location of the tumor, statokinetic disorders (gait disorder, ataxia in the limbs, etc.), and often strabismus, are often observed. Paralysis, paresis and epileptic seizures are rarely observed.
Cerebellar tumors are classified as subtentorial; they occur mainly in childhood (from 3 to 12 years) - in 68-70% of cases.
Astrocytoma in children has a nodular shape, does not infiltrate the brain tissue, but sharply compacts, stretches and deforms the cortex, white matter, can grow into the cavity of the fourth ventricle and into the brain stem, and often has cystic cavities.
Medulloblastoma grows into the roof of the fourth ventricle, fills its cavity and can grow into the brain stem; in most cases, it comes from the lower part and has infiltrating growth. The clinical picture mainly depends on the histological structure of the tumor. Astrocytoma and angioreticuloma have a benign course, medulloblastoma and sarcoma have a malignant course.
In children, the first clinical symptoms of a tumor can be provoked by a head injury, an infectious disease (influenza, acute respiratory disease) and are manifested by an increase in intracranial pressure - headache attacks, at the height of which vomiting occurs. Sometimes vomiting can be the first sign of illness. With medulloblastoma and sarcoma, especially in young children, the first symptoms can be in the form of intoxication, loss of body weight and appetite, lethargy, fatigue, sometimes anxiety, irritability, asthenia, enlarged lymph nodes, changes in blood (leukocytosis).
Focal symptoms of a cerebellar tumor are bilateral, since in children the tumor is often localized in the cerebellar vermis. In this case, nystagmus, coordination disorder, decreased muscle tone are observed, static coordination is disrupted: the patient cannot stand, sit, and falls backward in the Romberg position. When the lower part of the cerebellar vermis is involved in the process, the patient deviates backward; when the upper part is affected, the patient deviates forward. The gait is disturbed: the child staggers in both directions, often falls; static ataxia is combined with asynergia.
When the cerebellar hemispheres are affected, scanned, unevenly modulated speech is characteristic, and on the side of the tumor there is large-scale horizontal nystagmus. Symptoms of damage to the V, VI, VII, VIII nerves may be observed in the form of decreased corneal reflexes, strabismus, diplopia, asymmetry of the nasolabial folds, dizziness and tinnitus, as well as ataxia in the limbs on the affected side (overshooting, dysmetria, hypermetria, adiadochokinesis and muscular atony). During the process in the upper part of the hemisphere, it is mainly the arm that suffers, and in the lower part – the leg. When walking, the patient deviates towards the affected hemisphere.
Depending on the histological characteristics of cerebellar tumors, the dynamics of the disease changes. With benign tumors (astrocytoma), symptoms increase slowly, focal symptoms can appear 1-2 years after the tumor appears, general cerebral symptoms - headache, nausea, vomiting, dizziness - are not constant during this time, remissions are possible. In the presence of medulloblastoma, the increase in symptoms is rapid - over several months, characterized by general physical exhaustion and additional focal symptoms indicating supratentorial or spinal localization.
are the most common tumors of the brain stem . Initially, one of the cranial nerves is involved, then an alternating syndrome develops (expressed as paralysis). As the tumor grows, the symptoms become bilateral, bulbar or pseudobulbar syndrome, paresis and paralysis of the limbs occur. Tumors growing from the outer surface of the trunk first manifest themselves as symptoms of damage to the cranial nerves, then conduction disorders occur. When the tumor is localized in the midbrain, oculomotor disorders develop: ptosis, diplopia, impaired convergence, accommodation, strabismus, and ultimately, alternating Weber syndrome occurs. Damage to the roof of the midbrain is accompanied by paresis of upward or downward gaze, nystagmus, hearing loss, and ataxia; Hypertensive symptoms appear later.
When a tumor of the bridge occurs, paresis of gaze towards the lesion, alternating syndromes of Millard-Hübler, Foville, ataxia, and autonomic disorders (impaired heartbeat, sweating) occur. If the tumor is located in the medulla oblongata, respiratory and cardiovascular disorders, bulbar and pseudobulbar palsies, and alternating Jackson and Schmidt syndromes develop. With tumors in the zone of the IV ventricle, liquorodynamic disorders and attacks of occlusion are observed, characterized by the appearance of a sudden headache, vomiting, and sometimes disturbances of consciousness, breathing problems and cardiac activity (Bruns syndrome). With tumors of the cerebellopontine angle (neurinoma of the VIII nerve), a sensation of ringing in the ear and dizziness occurs. Then symptoms of damage to the facial, trigeminal and abducens nerves, as well as cerebellar disorders, appear. One of the common symptoms of a cerebellar tumor is a forced position of the head with an inclination in the direction opposite to the tumor lesion of the cerebellar hemisphere, less often in the same direction. During a headache attack, the position changes, the head is thrown back or brought forward to the chest.
Brain dislocation syndrome, or dislocation syndrome, is caused by compression of the brain by a tumor, hemorrhage or other focal process with the appearance of secondary symptoms of brain damage at a distance from the pathological focus due to increased intracranial pressure. The brain is enclosed in a closed space, therefore, with an increase in intracranial pressure, the brain matter is squeezed into the foramen magnum, various cracks formed by dense processes of the dura mater (the greater falciform process, the cerebellar tentorium), partially blocking the cranial cavity into different floors and separating parts of the brain from each other. friend. Clinically, this is manifested by increased intracranial pressure in combination with symptoms of compression, brain deformation, which is characterized by increased headache, vomiting, anisocoria, upward gaze paresis, sluggish pupillary response to light, hearing impairment, vegetative-vascular symptoms, and bilateral pathological foot signs.
Neuroma is a benign tumor of the nervous system that develops from the cranial nerves. It is observed in middle-aged and older children. Neuroma manifests itself as a symptom complex, which is characterized by hearing loss, dizziness, noise, headaches, and facial numbness.
Meningioma is a tumor in the dura mater of the brain. As a rule, this is a benign tumor that grows slowly; this tumor cannot always be removed. Note that meningiomas can also be malignant, in which case they grow into other parts of the body. Symptoms of meningioma develop slowly, these include the following signs: general cerebral - increasing headache, double vision, loss of vision, nausea and vomiting, mental and memory disorders, epileptic seizures, weakness in the limbs.
Are stages determined for tumors of the brain and spinal cord?
CNS tumors differ significantly from other tumors.
Thus, tumors of the brain and spinal cord almost never spread beyond the central nervous system. As they grow, they disrupt vital body functions.
Currently, there is no generally accepted staging system for CNS tumors. The main emphasis is placed on prognostic factors, the most important of which are: the type of cells from which the tumor arose, the degree of malignancy, the age of the child, the radicality of the operation, the location of the tumor, the severity of symptoms, the spread of the process to other parts of the central nervous system.
Brain stem tumors
According to the previously existing opinion, any tumor of the brain stem was considered an infiltrative formation, diffusely growing into brain stem structures and, as a result, not subject to surgical removal. It has now become clear that in addition to diffusely spreading tumors (which, unfortunately, are the majority), there are limited nodular tumors in the trunk, the removal of which is quite possible. In such cases, to decide on the advisability of surgical treatment, the patient needs to consult a neurosurgeon. The dominant principle of trunk tumor removal is maximum resection of its tissue with minimal trauma to brain structures. In this regard, great hopes are placed on the development of microneurosurgical surgical techniques.
Unfortunately, about 80% of trunk tumors are inoperable. In relation to them, as well as as pre- and postoperative therapy, chemotherapy and radiation can be used. Chemotherapy is carried out using a combination of various cytostatic drugs. Radiation therapy achieves symptomatic improvement in 75% of patients. However, already in the early stages after treatment, many of them die. The technique of radiotherapy with an increase in the total dose of radiation has made it possible to slightly increase the life expectancy of children with stem tumors. In 30% of children, life expectancy after radiotherapy was 2 years.
Stereotactic radiosurgery is an innovative method for treating stem tumors today. It is possible to carry out 2 types of procedures: gamma knife and cyber knife. In the first case, a helmet is put on the patient’s head, irradiation is carried out from multiple sources so that their rays converge at one point corresponding to the location of the tumor. The effect is achieved due to the total impact of radiation sources, while the irradiation of healthy brain tissue is minimal, since each beam carries a small gamma energy. The procedure for targeting a tumor using a cyber knife is more automated. The robotic device itself directs the radiation to the area where the tumor is located, taking into account its movements due to the breathing or movements of the patient. However, so far these methods are effective mainly against benign tumors up to 3-3.5 cm in size.
Forecast
Benign tumors of the brain stem, due to their slow growth, can exist for up to 10-15 years, often having a subclinical course. But, unfortunately, most tumors in this area are malignant and cause death within several years or months from the onset of symptoms. Treatment in such cases only briefly prolongs the life of patients.